

5 Top Mistakes After Total Hip Replacement | Avoid Common Post-Surgery Errors After Hip Replacement
This post contains affiliate links.
Welcome to your journey toward a pain-free, more mobile life post-total hip replacement. As an experienced orthopedic physical therapist with over four decades under my belt, I’m here to guide you away from frequent missteps that can hinder your recovery.
In this article, I will discuss the top five mistakes patients often make following hip replacement surgery, providing you with insights to avoid common pitfalls and foster a smoother, swifter rehabilitation process. Prepare to empower yourself with knowledge that ensures the best possible outcomes for your new hip.
Avoid the Top Five Common Mistakes After Hip Replacement Surgery
After total hip replacement surgery, the pathway to recovery can be straightforward, but it’s also fraught with potential missteps that you must conscientiously avoid to ensure a smooth and efficient healing process. As a seasoned orthopedic physical therapist, I’ve seen patients make critical errors that can hinder their outcome after surgery.
One of the top mistakes I see is neglecting recommended physical therapy sessions; these are designed to restore mobility and strengthen your new hip. It is common to experience discomfort, but adhering to your therapy schedule is crucial for optimal results after hip replacement.
Another common pitfall is over-exertion too soon after surgery. You might feel enthusiastic about your new joint, but remember that your body needs time to heal. Avoid strenuous activities that may compromise the integrity of your hip replacement.
Performing more activity, be it the recommended walking and exercise protocols recommended by the physical therapist, or Activity of Daily Living (ADLs), is by far and away the biggest mistake I see my Type A personality patients make.
Additionally, ignoring the prescribed weight-bearing restrictions can lead to undue stress on your healing hip. Although a common practice early in my career, restricting weight bearing on the new hip prosthes is not common today in the patients I see, unless there is a complicating factor such as a hip infection.
Also common is the tendency of some patients to shun the use of assistive devices. Using a walker is not a sign of weakness, but a step towards properly navigating the recovery period after total hip replacement.
My patients are using a walker early in their rehabilitation, not because of weight-bearing restriction, but because of confidence and balance.
While using the walker, my concentration is on the correction of abnormal gait patterns, such as unequal step stride, and also on ambulation endurance. I always keep my patients on the walker for a couple of days longer than they think necessary, but I never transition my patients to a cane.
A cane will reinforce the habit of limping that almost all my patients have developed from trying to decrease the weight-bearing pain before the hip replacement. Read my article: How Long After Hip Replacement Can You Walk Without a Limp?
Lastly, skipping follow-up appointments with your surgeon is a mistake to avoid. These check-ups are essential to monitor the progress of your hip replacement surgery and to address any concerns promptly. Whether you’re top of mind about safety or keen on getting back to your regular activities swiftly, being mindful of and steering clear of these common mistakes will pave the way for a successful recovery avoiding mistakes after total hip replacement surgery. Remember, avoiding these pitfalls is pivotal to benefit fully from your hip replacement.
Following Post-Operative Restrictions: Key to Joint Replacement Recovery
As an experienced orthopedic physical therapist, I’ve seen firsthand the consequences of patients not adhering to the post-operative restrictions given after total hip replacement surgery. It’s vital for a successful recovery that you follow these guidelines meticulously.
During the recovery period, the hip joint is vulnerable, and disregarding these limitations can lead to complications or even a revision surgery. After surgery, patients may feel a temptation to rush their progress, but remember, healing takes time and patience.
Total hip replacements require you to avoid certain movements that can dislocate the new joint, but there is a big difference in restrictions when comparing surgical approaches, the anterior versus posterior surgical approach. Read my article: Anterior vs. Posterior Hip Replacement: Pain, Surgery & Approaches Compared
Many complications can be avoided by simply following the doctor’s prescribed precautions. Ensure you are clear on the specific precautions given for your situation, whether it’s a matter of permitted activities or avoiding certain positions when sitting or lying down. Always keep in mind that the process of healing and fully integrating your total hip into your body’s biomechanics is delicate.
Engage diligently in physical therapy sessions and don’t neglect exercises that have been recommended for home practice. By faithfully following these measures, you’re not only safeguarding your total hip’s longevity but also improving your overall chances for a full recovery .
Inadequate Pain Management: A Common Post-Surgery Mistake After Hip Surgery
After undergoing a total hip replacement, it’s essential to address post-operative pain with the utmost care. Nevertheless, inadequate pain management is a frequent oversight and may significantly impede your recovery journey.
It is not uncommon to experience pain after surgery, but how you manage it can make a world of difference. It’s vital to communicate openly with your healthcare team regarding your comfort levels and requirements, to ensure that pain does not persist untreated.
Once you’ve had hip replacement surgery, remember that your joint is healing, and adequate pain relief is necessary to participate in rehabilitation. Managing pain after surgery isn’t just about comfort; it directly affects your ability to perform necessary exercises and impacts your overall recovery. Those who do not adequately control pain may experience limited mobility in their hip and compromised joint function.
Many patients fear becoming reliant on medication; however, used judiciously under your doctor’s guidance, pain relief post-total hip replacement can lead to a smoother and quicker recovery. Inadequate pain management after hip surgery can result not only in discomfort but can also deter you from resuming normal activities, thus extending the rehabilitation process.
A key aspect of recovery after surgery involves balancing rest and movement. Managing your pain will allow you to adhere to post-operative restrictions correctly and engage in prescribed activities at the right pace. Whether it’s medication or other pain management techniques, they should always be administered as per your healthcare provider’s instructions.
One good non-medication pain control method is using cold therapy.
The best way to use cold therapy is to use a cold therapy machine or cold gel freezer packs (Amazon links). My first choice is the Ossur Cold Rush Therapy Machine. A less expensive option is the Core Gel Cold Packs. Read my article: Ice After Total Hip Replacement: A PT’s Complete Guide

Taking this seriously is crucial for after surgery care. A joint that’s well taken care of after a hip replacement will have the best chance for a full return to function, enabling you to move past the pain and towards a more active lifestyle.
Swelling Control: Essential for Recovery After Joint Surgery
After hip replacement surgery, one of the most crucial factors for a successful recovery is effective swelling control. Swelling is a natural response after surgery, as the body initiates healing processes in the joint area. However, excessive swelling can lead to complications, impede mobility, and slow down the overall recovery process.
It’s important for patients recovering from total hip replacement to take active measures in reducing swelling to promote optimal healing. Keeping the affected hip elevated and applying ice can help manage the swelling in the initial days after the joint surgery.
My referring surgeons also instruct the patient to wear a full-length thigh-high TED hose to control swelling. Read my article: How Long to Wear Compression Socks After Surgery: Post-Surgery TED Hose Guide

Additionally, gentle and guided movements, as prescribed by your healthcare provider, encourage circulation and help disperse fluid buildup around the hip. Ignoring the significance of swelling control after hip replacement surgery is a common post-surgery error. It’s not just about comfort, prolonged swelling can affect the new joint’s function and longevity.
Following the recommended exercises and wearing compression garments, if advised, are part of the recovery regimen that shouldn’t be overlooked.
Moreover, adherence to post-operative restrictions plays a pivotal role in swelling control and joint recovery. Overexerting or engaging in activities too soon can aggravate swelling and compromise the integrity of the hip. The goal is a balance of rest and activity to ensure the hip has time to heal without becoming stiff or weak.
Incorporating these measures into your recovery routine can significantly influence the outcome of your total hip replacement. Remember, recovery is not just a phase; it’s the foundation upon which your new joint’s health and functionality are built. Patience and diligence in managing swelling after surgery are essential steps on the path to regaining mobility and resuming the activities you enjoy.
Physical Therapy Consistency: Best Practice for Hip Replacement Success
After hip replacement surgery, embracing physical therapy consistency is among the top predictors of a successful recovery. As an orthopedic physical therapist with over forty years of experience, I’ve seen the profound impact that dedication to therapy can have on patients’ outcomes.
It’s crucial not to underestimate the role of consistent physical therapy in your journey after hip replacement surgery. Good physical therapy practices, when adhered to regularly, can significantly enhance the stabilization and strengthening of your new hip joint. This consistency in therapy post-surgery maximizes your functional gains, minimizes potential complications, and restores mobility more effectively.
Ignoring the prescribed physical therapy protocols after hip replacement surgery is a common mistake I’ve witnessed among patients. It’s paramount that you maintain the best level of engagement with your recuperative exercises, ensuring that each session of physical therapy becomes a cornerstone in your recovery after surgery.
Rigorous adherence to therapy schedules not only improves your hip’s range of motion but also aids in managing post-surgical pain and swelling, key aspects highlighted in prior sections, such as “Inadequate Pain Management: A Common Post-Surgery Mistake After Hip Surgery” and “Swelling Control: Essential for Recovery After Joint Surgery.”
Remember, the goal of therapy after a hip replacement is to return you to your best possible function. Embark on this journey with the understanding that your hip and overall health depend on the good execution of your therapy plan. The best outcomes are not merely linked to the surgical technique or the surgeon’s skill, but are equally tied to the patient’s commitment to their physical therapy regimen. Indeed, consistency is key in the narrative of your hip’s recovery journey.
Home Exercise Importance After Joint Institute Surgery Treatment
Understanding the home exercise importance cannot be overstated after hip replacement surgery. As a seasoned orthopedic physical therapist, I’ve observed countless patients navigate the post-surgery journey. Integrating exercises into your daily routine at home plays a pivotal role in your recovery after undergoing a total hip replacement at a joint institute. Through meticulously designed exercises, you’ll foster strength and flexibility in the hip.
Exercises, when done correctly and consistently, can significantly expedite your journey to reclaiming your mobility. Regrettably, a common mistake post-surgery is neglecting the home component of your rehab protocol. The total hip replacement procedure is merely the initial step towards your mobility restoration, and an institute specializing in joint surgery generally provides comprehensive guidance for the regimen you should follow at home. These exercises are tailored to maintain the integrity of your new hip, hence their importance is second to none.
Many might feel a sense of relief after hip replacement surgery, leading to complacency when at home. It’s crucial to integrate home exercises into your recovery plan provided by your joint institute. Consistent physical therapy at home, as well as in-clinic sessions, are best practices for hip replacement success.
It’s also important to control post-surgery swelling through recommended exercises. Moreover, inadequate pain management is a common mistake that can deter you from sticking to your exercises; however, adhering to your pain management plan allows you to engage more efficiently in your at-home regime.
As an orthopedic physical therapist, I guide my patients through exercises focused on the hip and joint recovery after surgery, stressing the importance of maintaining consistency.
The impact of home exercises on the long-term success of your total hip replacement cannot be understated, showcasing the critical nature of incorporating them into your daily life post-surgery. Remember, after hip replacement surgery, the journey to recovery is a marathon, not a sprint, and with the right exercises, you’ll reach your milestones confidently and safely.
Neglecting Overall Health: A Top Mistake After Surgery
As an orthopedic physical therapist with a history of rehabilitating hundreds, if not thousands of patients, I’ve witnessed many patients make the crucial mistake of neglecting overall health after hip replacement surgery.
Beyond the specific recovery from surgery, your entire well-being is pivotal for a successful healing process. In the United States, the number of joint surgeries has ascended, bringing forth an emphasis on comprehensive health management post-surgery. It’s not enough to focus narrowly on the operated bone; rather, a holistic approach is essential.
After surgery, patients sometimes underestimate the value of nutrition, hydration, and even mental health. It’s a misconception that once surgery is completed, the hardest part is over. However, surgery marks the beginning of a journey. Health related habits such as smoking, poor diet, and inactivity can hinder recovery, impacting not only the new joint but also the function of the entire body. Recall that the goal is to return to activities that were hampered by your hip condition prior to surgery; this requires the whole system’s cooperation.
Moreover, complications like infections can be a threat if overall health is not taken into account. It’s not uncommon to miss subtle signs of systemic issues when you’re solely focused on the surgical area.
Following post-surgery instructions from your joint institute or surgery treatment center is critical. This includes adhering to prescribed home exercises and recognizing that swelling control, pain management, and physical therapy consistency are part of a wider health strategy. To forego or de-prioritize these after-surgery practices would be a considerable error.
Don’t fall into the pitfall of neglecting overall health after hip replacement surgery. A comprehensive health focus will support bone integrity and facilitate a united effort towards recovery, a principle upheld in every successful recuperation narrative shared by thousands of patients across the United States.
Bonus Tips from Texas Joint Institute for Post-Hip Replacement Care
The Texas Joint Institute is renowned for pioneering comprehensive care practices across the United States, and their insights can immensely benefit patients after hip replacement surgery.
First and foremost, it’s vital to adhere to the post-operative restrictions provided by your surgeon. These are designed to protect the integrity of the new hip joint and ensure proper healing. Moreover, managing pain after surgery isn’t just about comfort; it’s crucial for enabling participation in physical therapy and daily activities, thus fostering a quicker recovery.
Swelling is a natural response after joint replacement, but it must be controlled to prevent complications. Techniques such as ice, compression, and elevation are simple yet remarkably effective. Speaking of physical therapy, maintaining consistency in your physical therapy sessions contributes to restoring strength and mobility to your hip joint.
This same principle applies to following through with your home exercise regimen to reinforce the progress made during therapy. It’s essential to not overlook the importance of overall health in the recovery phase. Adequate nutrition, hydration, and rest play significant roles in healing after surgery.
The Texas Joint Institute’s bonus tips encapsulate their commitment to exceptional joint replacement care, offering guidance for patients to navigate the journey of recovery securely. By avoiding the top mistakes and embracing these bonus tips, you’re more likely to enjoy a successful return to your active lifestyle.
Read my other articles about Total Hip Replacement
Frequently Asked Questions
Q: What are some common mistakes after total hip replacement surgery? A: After hip replacement surgery, patients often make mistakes like neglecting prescribed physical therapy sessions, overexerting themselves too soon, avoiding the use of assistive devices like walkers, and skipping follow-up appointments with their surgeon. All of these actions can hinder your recovery and negatively affect the outcome of your surgery.
Q: What are the consequences of not adhering to post-operative restrictions? A: Ignoring post-operative restrictions can lead to complications or even the need for revision surgery. These limitations are in place to protect your new hip joint during the vulnerable phase of healing. Activities that could dislocate the new joint, such as deep bending or crossing your legs, should be avoided in the posterior approach to total hip replacement.
Q: Why is managing pain after hip surgery so important? A: Adequate pain management is key to a successful recovery because it allows you to participate effectively in rehabilitation exercises, which are necessary for healing. Uncontrolled pain can lead to reduced mobility in the hip, prolonged recovery, and an increased risk of complications.
Q: How can I effectively control swelling after hip replacement surgery? A: To manage swelling, keep the operated hip elevated when possible, apply ice, and engage in prescribed gentle movements to encourage circulation. Avoid overexertion and adhere to your surgeon’s guidelines regarding rest and activity balance.
Q: What role does physical therapy consistency play in recovery after hip replacement? A: Consistent participation in physical therapy is crucial for stabilizing and strengthening your new hip joint. It’s important to attend all scheduled therapy sessions and perform recommended exercises at home, as this consistency maximizes functional gains and supports a smoother recovery.
Paying It Forward
Age In Place School is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com. We also participate in other affiliate programs which compensate us for referring traffic.
Dr. Robert Donaldson
Dr. Donaldson is dually licensed; physical therapy in 1975 and doctor of chiropractic in 1995. He held credentials of Orthopedic Clinical Specialist in physical therapy for 20 years, QME in California, and taught at USC. He owns and operates an orthopedic physical therapy practice. See "About Me" page.
Recent Posts
Who Should Not Have Knee Replacement Surgery & Reasons to Avoid Knee Replacement
In my forty years as an orthopedic physical therapist, I've guided countless patients through the decision-making process for total knee replacement surgery. While it's a life-changing procedure for...
Knee Replacement Surgery Alternatives: Explore Your Options for Alternative to Total Knee Replacement
For those suffering from debilitating knee pain, the prospect of total knee replacement surgery can be both a beacon of hope and a source of uncertainty. With advances in medical science, however,...

A Guide to Your Hip Replacement Recovery Journey
by empirical360 | Feb 1, 2021 | Hip Pain , Outpatient Total hip and Knee Replacement
Hip replacement surgery can become a patient’s best option to reduce pain related to osteoarthritis and other age-related conditions if pain is seriously disrupting quality of life and conservative treatments are no longer effective. It’s really important to understand that successful joint replacements require commitment on the part of the patient, and hip replacement recovery is an essential part of this. An orthopedic surgeon can successfully replace the damaged joint with an artificial joint, but once the incision is closed, so much is up to the patient.
The OJRCA team is passionate about delivering patient-centered care, and we believe that patient education is a critical part of that mission. We’ve created the following guide to help patients considering hip replacement procedures understand the recovery journey and make the plans that can help them achieve a positive outcome.
The Day of Your Minimally Invasive Hip Replacement Procedure
By using muscle and tendon-sparing techniques, our experienced and highly skilled orthopedic surgeons are able to perform hip replacement surgery on an outpatient basis. One of the biggest advantages to this approach for hip replacement recovery is a smaller incision and limited disruption of surrounding soft tissue. This means the incision can heal quicker and patients can get up and on their feet much sooner, which is essential for recovery and rehabilitation after joint replacements.
Patients at OJRCA will be given detailed pre- and post-operative instructions to prepare them for the day of the hip replacement procedure and the immediate recovery period. After the procedure is performed, patients will be brought to the recovery area.
After vitals have been taken and clearance given by medical professionals, patients will typically get up with physical therapy and then be able to return home the day of the procedure. Physical therapy should begin as soon as possible, typically the next day. The sooner the better. Patients will be given pain medication and instructions for proper usage. It is critical to follow the dosage guidelines. While patients should never take more than the minimum effective dosage, it is still important to stay on top of pain while in recovery.
Hip Replacement Recovery — Days One to Two
You will be given instructions for safely resuming basic activities as well as how to stay safe in your home during the recovery period. Examples of how to stay safe during hip replacement recovery include:
- Using handrails on steps and any other location
- Wearing flat shoes with slip-proof soles
- Avoiding slippery surfaces, such as wet or waxed floors.
- Keeping floors free of items that obstruct movement
- Removing throw rugs or small objects, or making them slip proof
- Be cautious of pets or other animals that could get in your way.
- Avoiding ice or snow, if necessary
Another important element to watch for in the first several days after surgery is blood clots. Always follow your orthopedic surgeon’s instructions carefully to limit your risk of blood clots, which can occur during the early period of your recovery. Indicators of blood clots as a result of hip replacement surgery include:
- Increased pain in the lower leg and calf.
- Tenderness and visible redness in the leg or thigh.
- Increased inflammation of the calf, ankle and foot.
It is also possible for post-surgical blood-clots to travel into the lungs and disrupt respiration. Indicators that this has occurred include, shortness of breath, onset of chest pain. If you notice any of these signs, it is important to immediately get in touch with your surgical provider or your primary care physician.
The First Week After Hip Replacement and Infection Prevention
Yet another key safety concern in the hip replacement recovery period is infection of the surgical site or implant. While implant infection is a very low risk factor, it can occur in an extremely small percentage of cases and every patient should watch for them. The most important actions that can help to lower the risk of infection after total joint replacement include:
- Follow guidelines for skin washing with antiseptic soap the days preceding surgery as instructed
- Leaving the dressing in place as it is placed in the operating room under sterile conditions and is a special dressing with a silver compound that helps prevent infection.
Patients should continue physical therapy and follow guidelines for resuming regular activities. During this time or slightly after, you can expect a post-operative appointment to check on the incision site and remove material from the wound, such as staples, if necessary.
Hip Replacement Recovery — the first week
You may be able to resume activities and can begin to transition from a walker to a cane after the first day or so. Your doctor may also clear you to start driving again, so long as you are not taking any pain medication.
Do not resume any vigorous activities without the express consent of your physician. In general, if you still require a walker or cane, there are still likely mobility problems that would make these activities overly risky.
The Importance of Physical Therapy
Physical therapy is absolutely critical to ensure a successful hip replacement recovery. Not only do the hips need rehabilitation after surgery to regain range of motion and function, but chronic hip pain sufferers typically deal with years of muscle atrophy and immobility. Working with a physical therapist helps to overcome these obstacles as well as learn how to properly function with your new artificial joint.
Typical physical therapy methods include:
- Therapeutic exercises to strengthen the hip and improve range of motion
- Manual therapy to activate the hip joints and improve blood flow
- Therapeutic massage to relieve tense muscles
While it is important to start physical therapy early in the recovery process, patients should expect to commit to therapy during the duration of hip replacement recovery to promote the highest degree of hip health and function.
Resuming Activities and Committing to a Healthy Lifestyle
Most people are usually able to return to normal activities within 2 weeks, but full recovery may take longer. Long-term relief very often relies on living a healthy lifestyle that reduces the risk of hip inflammation and the stress we place on the hip every day. Common steps include:
- Eating a nutritious diet with anti-inflammatory foods
- Managing your weight to reduce pressure on the hip joints
- Getting regular exercise to strengthen the body and improve cardiovascular health
- Avoiding tobacco products and excessive alcohol consumption
- Practicing good sleep hygiene and getting a good night’s sleep
Reach out to OJRCA to Learn About Your Treatment Options and the Hip Replacement Recovery Journey Have you been living with the highly disrupting symptoms of arthritis of the hip and other degenerative conditions? While conservative treatment options help many people on their recovery journey, many others find themselves dealing with pain and limited mobility after fully exploring nonsurgical treatment. To learn more about the benefits of outpatient total hip replacement surgery by our expert surgical team, contact us today .
Recent Posts
- Understanding Synovial Tissue Damage Treatment
- What is Articular Cartilage Damage? Causes and Treatment
- How to Approach Treatment for Torn Ligaments
- Torn Meniscus? Three Steps to Relief
- What to Know About Treating Hip Fractures
- Finding Joint Pain Relief for Rheumatoid Arthritis
- How to Find the Right Orthopedic Surgeon in Tampa for You
- Understanding the Outpatient Hip Replacement Advantage
- February 2021
- January 2021
- October 2020
- September 2020
- Outpatient Total hip and Knee Replacement
- Uncategorized
Get in touch with us
- Phone Number
- Email Address
3030 N Rocky Point Dr, Tampa, FL 33607
(813) 281-0567
Let's get connected
Get in Touch

Get maximum pain relief with same-day, minimally invasive surgery.
3030 N. Rocky Point Drive West
Tampa, FL 33607
(813)281-0567
[email protected]
Privacy Policy
- Patient Care & Health Information
- Tests & Procedures
- Hip replacement
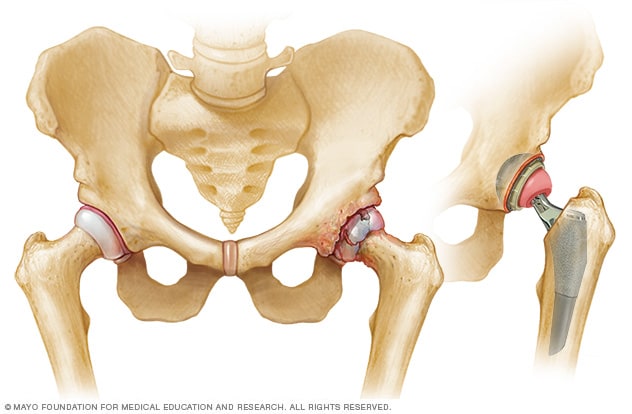
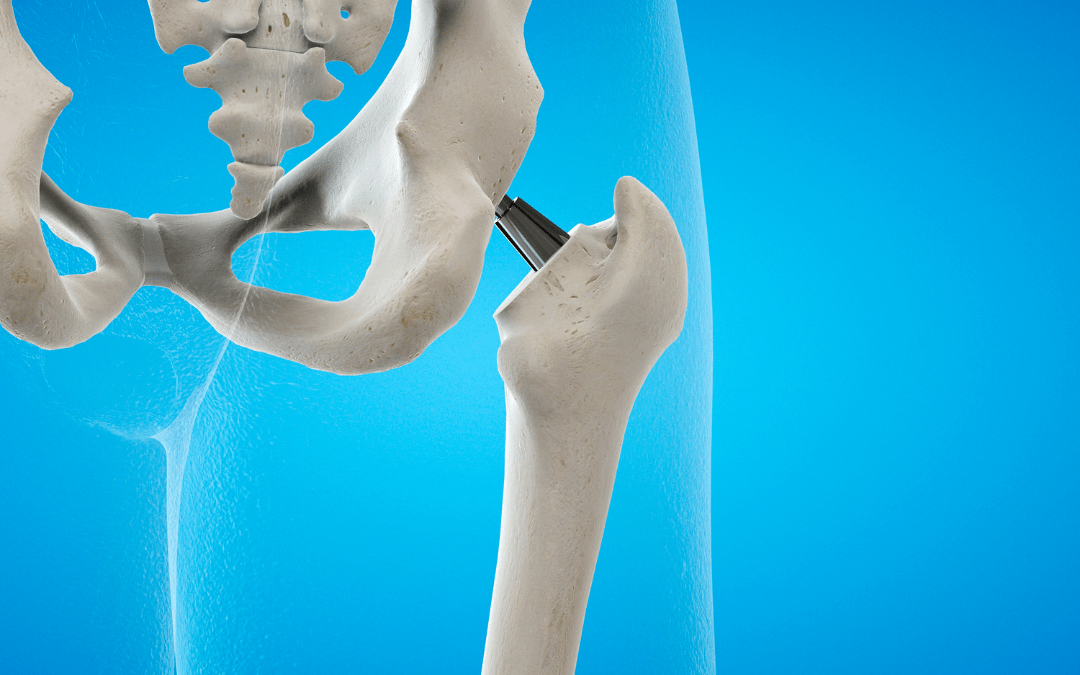
- Artificial hip
Hip prostheses are designed to mimic the ball-and-socket action of your hip joint. During hip replacement surgery, your surgeon removes the diseased or damaged parts of your hip joint and inserts the artificial joint.
During hip replacement, a surgeon removes the damaged sections of the hip joint and replaces them with parts usually constructed of metal, ceramic and very hard plastic. This artificial joint (prosthesis) helps reduce pain and improve function.
Also called total hip arthroplasty, hip replacement surgery might be an option if hip pain interferes with daily activities and nonsurgical treatments haven't helped or are no longer effective. Arthritis damage is the most common reason to need hip replacement.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- A Book: Mayo Clinic Guide to Arthritis
- Assisted Walking and Mobility Options at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Conditions that can damage the hip joint, sometimes making hip replacement surgery necessary, include:
- Osteoarthritis. Commonly known as wear-and-tear arthritis, osteoarthritis damages the slick cartilage that covers the ends of bones and helps joints move smoothly.
- Rheumatoid arthritis. Caused by an overactive immune system, rheumatoid arthritis produces a type of inflammation that can erode cartilage and occasionally underlying bone, resulting in damaged and deformed joints.
- Osteonecrosis. If there isn't enough blood supplied to the ball portion of the hip joint, such as might result from a dislocation or fracture, the bone might collapse and deform.
Hip replacement may be an option if hip pain:
- Persists, despite pain medication
- Worsens with walking, even with a cane or walker
- Interferes with sleep
- Affects the ability to walk up or down stairs
- Makes it difficult to rise from a seated position
Risks associated with hip replacement surgery can include:
- Blood clots. Clots can form in the leg veins after surgery. This can be dangerous because a piece of a clot can break off and travel to the lung, heart or, rarely, the brain. Blood-thinning medications can reduce this risk.
- Infection. Infections can occur at the site of the incision and in the deeper tissue near the new hip. Most infections are treated with antibiotics, but a major infection near the new hip might require surgery to remove and replace the artificial parts.
- Fracture. During surgery, healthy portions of the hip joint might fracture. Sometimes the fractures are small enough to heal on their own, but larger fractures might need to be stabilized with wires, screws, and possibly a metal plate or bone grafts.
- Dislocation. Certain positions can cause the ball of the new joint to come out of the socket, particularly in the first few months after surgery. If the hip dislocates, a brace can help keep the hip in the correct position. If the hip keeps dislocating, surgery may be needed to stabilize it.
- Change in leg length. Surgeons take steps to avoid the problem, but occasionally a new hip makes one leg longer or shorter than the other. Sometimes this is caused by a contracture of muscles around the hip. In these cases, progressively strengthening and stretching those muscles might help. Small differences in leg length usually aren't noticeable after a few months.
- Loosening. Although this complication is rare with newer implants, the new joint might not become solidly fixed to the bone or might loosen over time, causing pain in the hip. Surgery might be needed to fix the problem.
- Nerve damage. Rarely, nerves in the area where the implant is placed can be injured. Nerve damage can cause numbness, weakness and pain.
Need for second hip replacement
The artificial hip parts might wear out eventually, especially for people who have hip replacement surgery when they're relatively young and active. If this happens, you might need a second hip replacement. However, new materials are making implants last longer.
How you prepare
Before the operation, you'll have an exam with the orthopedic surgeon. The surgeon may:
- Ask about your medical history and current medications
- Examine your hip, paying attention to the range of motion in your joint and the strength of the surrounding muscles
- Order blood tests and an X-ray. An MRI is rarely needed
During this appointment, ask any questions you have about the procedure. Be sure to find out which medications you should avoid or continue to take in the week before surgery.
Because tobacco use can interfere with healing, it's best to stop using tobacco products. If you need help to quit, talk to your doctor.
What you can expect
When you check in for your surgery, you'll be asked to remove your clothes and put on a hospital gown. You'll be given either a spinal block, which numbs the lower half of your body, or a general anesthetic, which puts you into a sleep-like state.
Your surgeon might also inject a numbing medicine around nerves or in and around the joint to help block pain after your surgery.
During the procedure
The surgical procedure can be completed within two hours. To perform a hip replacement, the surgeon:
- Makes an incision over the hip, through the layers of tissue
- Removes diseased and damaged bone and cartilage, leaving healthy bone intact
- Implants the replacement socket into the pelvic bone
- Inserts a metal stem into the top of the thighbone, which is then topped with a replacement ball
After the procedure
After surgery, you'll be moved to a recovery area for a few hours while your anesthesia wears off. Medical staff will monitor your blood pressure, pulse, alertness, pain or comfort level, and your need for medications.
You'll be asked to breathe deeply, cough or blow into a device to help keep fluid out of your lungs. How long you stay after surgery depends on your individual needs. Many people can go home that same day.
More information
- Outpatient joint replacement: Is it a safe option?
Blood clot prevention
After hip replacement surgery, you'll temporarily be at increased risk of blood clots in your legs. Possible measures to prevent this complication include:
- Moving early. You'll be encouraged to sit up and walk with crutches or a walker soon after surgery.
- Applying pressure. Both during and after surgery, you might wear elastic compression stockings or inflatable air sleeves on your lower legs. The air sleeves squeeze and release your legs. That helps keep blood from pooling in the leg veins, reducing the chance that clots will form.
- Blood-thinning medications. Your surgeon might prescribe an injected or oral blood thinner after surgery. Depending on how soon you walk, how active you are and your overall risk of blood clots, you might need blood thinners for several weeks after surgery.
Physical therapy
Daily activity and exercise can help you regain the use of your joint and muscles. A physical therapist can recommend strengthening and mobility exercises and can help you learn how to use a walking aid, such as a walker, a cane or crutches. As therapy progresses, you'll gradually increase the amount of weight you put on your leg until you're able to walk without assistance.
Home recovery
Before you leave the hospital, you and your caregivers will get tips on caring for your new hip. For a smooth transition:
- Arrange to have a friend or relative prepare some meals in advance
- Place everyday items at waist level, so you won't have to bend down or reach up
- Consider getting a raised toilet seat and a shower chair for your recovery at home
- Put your phone, tissues, TV remote, medicine and books near the area where you'll be spending most of your time during recovery
Full recovery from a hip replacement varies from person to person, but most people are doing well three months after the surgery. Improvements typically continue during the first year after surgery.
The new hip joint can reduce pain and increase the hip's range of motion. But don't expect to do everything you could do before the hip became painful.
High-impact activities, such as running or playing basketball, might be too stressful on the artificial joint. But in time, most people can participate in lower-impact activities — such as swimming, golfing and bicycle riding.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Hip replacement care at Mayo Clinic
- Hip replacement. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/hip-replacement-surgery/advanced. Accessed Nov. 2, 2021.
- Erens GA, et al. Total hip arthroplasty. https://www.uptodate.com/contents/search. Accessed Nov. 2, 2021.
- Total hip replacement. American Academy of Orthopaedic Surgeons. https://orthoinfo.aaos.org/en/treatment/total-hip-replacement. Accessed Nov. 2, 2021.
- Goldman L, et al., eds. Surgical treatment of joint diseases. In: Goldman-Cecil Medicine. 26th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Nov. 2, 2021.
- Erens GA, et al. Complications of total hip arthroplasty. https://www.uptodate.com/contents/search. Accessed Nov. 2, 2021.
- Azar FM, et al. Arthroplasty of the hip. In: Campbell's Operative Orthopaedics. 14th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Nov. 2, 2021.
- Office of Patient Education. Total hip replacement surgery. Mayo Clinic; 2018.
- Sierra RJ (expert opinion). Mayo Clinic. Dec. 8, 2021.
- Jensen NA. Allscripts EPSi. Mayo Clinic. Dec. 10, 2021.
- 3D Printer Helps Hip
- Avascular necrosis (osteonecrosis)
- Bone metastasis
- Hip dysplasia
- Hip fracture
- Hip Surgery Overview
- Hockey Coach Gets Hip
- Osteoarthritis
- Outpatient joint replacement
- Rheumatoid arthritis
- Stem Cells Get Hip
- Two types of hip implants
- Walker tips
News from Mayo Clinic
- Mayo Clinic expert: Warm climates offer mobility options for snowbirds after surgery Jan. 29, 2024, 10:07 p.m. CDT
- Mayo Clinic Minute: What to know about aging and joint replacements Oct. 31, 2023, 03:49 p.m. CDT
- Mayo Clinic expert: Joint replacement surgery, arthritis are not inevitable Sept. 27, 2023, 01:25 p.m. CDT
- Mayo Clinic in Florida awarded top national certification for advanced total hip, knee replacement Oct. 28, 2022, 03:00 p.m. CDT
- Mayo Clinic Q and A: Managing osteoarthritis for hips and knees Sept. 29, 2022, 12:32 p.m. CDT
- Expert alert: Outpatient joint replacement surgery benefits patients May 11, 2022, 03:00 p.m. CDT
- Expert Alert: Mayo Clinic expert shares tips for good outcomes after hip, knee replacement surgery April 26, 2022, 03:30 p.m. CDT
- Sharing Mayo Clinic: Back on the bandstand April 03, 2022, 11:00 a.m. CDT
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
Prices | Medical form | About Us | Patient blog | News | Find a doctor | KCM Academy | KCM Family | Contact us
- Allurion Program
- Obesity is a disease
- Causes and effects of obesity
- Guide: 10 steps for losing weight
- Our Bariatric Surgeons and Specialists Team
- Aftercare program
- Patient stories
- Bariatric diet
- BMI Calculator
- Gastric Sleeve (SG)
- Gastric Bypass (RYGB)
- Mini Gastric Bypass (OAGB, MGB)
- Revisional surgery
- Gastric Band Removal
- SASI Bypass
- Endoscopic sleeve gastroplasty (ESG)
- Weight Loss Balloon Orbera
- ALLURION Weight Loss Program
- Bariatric and Metabolic Clinic
- Dietetics and Nutrition Clinic
- Clinical Psychology Clinic
- Diabetology Clinic
- Cardiology Clinic
- Physiotherapy Clinic
- POLAND (EU) vs TURKEY
- Breast Implant & Enlargement
- Breast lift
- Breast reduction
- Preventive mastectomy
- Breast reconstruction
- Plastic surgery of the nipple and areola
- Gynecomastia surgery
- Nose surgery
- Ear surgery
- Eyelid surgery
- Eyebrow lifting
- Face and neck lifting
- Cheek and chin implants
- Tummy Tuck (Abdominoplasty)
- Tummy tuck with the Fleur de Lis
- Thigh Plastic Surgery | Thighplasty | Thigh Lift Surgery
- Arm Lift Surgery | Shoulder Plastic Surgery | Brachoplasty
- Buttock implants
- Buttock Augmentation
- Body Plastic Surgery | Belt Lipectomy | Body Lift Surgery
- Bra Line Back Lift Surgery
- Labiaplasty
- N.I.L. liposuction – Stomach
- N.I.L. liposuction – Hips
- N.I.L. liposuction – Thighs
- N.I.L. liposuction – Arms
- N.I.L. liposuction – Knees
- N.I.L. liposuction – Calves
- N.I.L. liposuction – Back
- N.I.L. liposuction – Chin
- Endoscopic spine surgery (ESS)
- Vertebroplasty
- Thermal radiofrequency denervation
- Coblation – nucleotomy-discectomy, cervical episode
- SED-YESS lumbar endoscope
- Dynamic stabilisation with Medtronic DIAM flexible implant
- Gel implant of the spine – DISCOgel nucleoplasty
- Diagnostic Block
- Knee arthroscopy
- Shoulder arthroscopy
- Arthroscopy of the ankle joint
- ACL / Cruciate ligament reconstruction
- Hip joint replacement
- Knee joint replacement
- Ankle joint and foot
- Bunion surgery
- Carpal tunnel surgery (CTS)
- Tarsal tunnel release
- Stem cells and plasma
- Uterine fibroids operations
- Laparoscopic surgery of the uterus, ovaries and fallopian tubes
- Laparoscopic tubal ligation reversal
- Laparoscopic endometriosis surgery
- Fallopian tube microsurgery in infertility
- Infertility diagnosis
- Vaginal gynecological operations
- Aesthetic gynecology
- Endoscopic surgery of the urinary tract
- Endoscopic prostate surgery
- Prostate laser surgery
- Laser removal of urinary stones
- Laparoscopic kidney surgery
- Laparoscopic prostate surgery
- Urinary incontinence operations
- Operations and prostheses of penile
- Operations of the scrotum and testicles
- Endoscopic bladder surgery
- Cystoscopy under anesthesia
- Prostate biopsy
- Vasectomy Reversal Surgery (Microsurgery)
- Penile Curvature Surgery
- Varicocele surgery
- Endoscopic vaporization of the prostate-diathermy Olympus (TURIS-P)
- General dentistry
- Children’s dentistry
- Root canal treatment – microscopic endodontics
- Dental implants
- Orthodontics
- Dental surgery
- Aesthetic dentistry – teeth whitening
- Weight Loss Surgery
- Plastic Surgery
- Spine Surgery
- Orthopedics
- Laparoscopic Gallbladder removal
- Laparoscopic Abdominal hernia repair
- Laparoscopic Inguinal hernia repair
- Laparoscopic Adrenal gland repair
- Laparoscopic small or large bowel surgery
- Laparoscopic surgery for intestinal tumors
- Laparoscopic surgery for adrenal tumors
- Mastectomy with breast reconstruction
- Partial thyroid resection
- Total thyroid resection
- FESS sinus surgery
- Nose and septal surgery
- Snoring treatment RAVOR
- Laryngeal microsurgery
- Removal of the Pharyngeal Tonsil
- Salivary gland operations
- Plastic of protruding ears
- Sleep polygraphic examination
- Implantable contact lens (ICL)
- Cataract surgery
- Intravitreal injections in AMD
- Laser therapy
- Hernia operations
- Phimosis plastic surgery
- Cryptorchid surgery
- Excision of skin lesions
- Plastic surgery of the frenulum
- Rehabilitation center
- Orthopedic rehabilitation
- Neurological rehabilitation
- Sports rehabilitation
- Spinal rehabilitation
- Magnetic Resonance OMEGA
- Computer Tomograph OMEGA
- RTG / X-ray
- Colonoscopy vs Gastroscopy – The key differences
- USG / Doppler
- Breast USG with BI-RADS description
- Cardiological diagnosis
- Imaging diagnostics of the eye
- Urodynamics
- Program Allurion
- Patient blog
- Mini Gastric Bypass (OAGB. MGB)
- Allurion Gastric Balloon – Weight loss without surgery
- Obesity Treatment Centre
- Fleur de Lis Tummy Tuck
- Prosthetics
- Plastic & Cosmetic Surgery
- Laparoscopic small or large intestine bowel surgery
- Rehabilitation Center
- Sports rehabilitations
- Specialist clinics
Hip Replacement Recovery: Timeline, Tips and Information
- Patient Blog
- Hip Replacement Recovery: Timeline, Tips…
Sep 20 2023

Hip replacement, also known as arthroplasty, is a surgical procedure wherein the worn-out or damaged sections of the hip joint are replaced with artificial implants. These artificial parts can be made from a variety of materials, such as metal, plastic, or ceramic, and are designed to replicate the natural motion of the hip joint.
While the surgery offers many the chance to live without hip pain, understanding the hip replacement recovery timeline and what to expect post-operation is essential. Let’s delve deeper into the details to make your total hip replacement recovery journey smoother.
What To Expect After Hip Replacement Surgery
After your surgery, you’ll wake up in a recovery room and be monitored for any immediate post-operative complications. Pain management is a priority, and you’ll be given medications to alleviate discomfort.
Once you’re stable, physiotherapy typically begins the day after the surgery, with a focus on ensuring you can safely move in and out of bed. Breathing exercises might be recommended to clear your lungs.
At KCM Clinic, our dedicated team of specialists ensures that every patient receives individualised care. We emphasise the importance of early mobility, as it plays a crucial role in preventing postoperative complications like blood clots.
Hip Replacement Recovery Timeline
Initial 48 hours.
This is the immediate post-operative phase. Pain management, wound care, and beginning mobility are primary focuses. You may be encouraged to stand or walk with assistance.
First Few Weeks
Gradually, your mobility will increase. You will transition from walking with a walker or crutches to a cane and eventually walk independently.
Six To Twelve Weeks
By this time, most patients resume their daily activities with modifications. However, high-impact exercises and strenuous activities are still discouraged.
Three To Six Months
This period marks significant improvements. Most patients can start engaging in more vigorous daily activities, but it is recommended to always consult your orthopaedic surgeon before attempting any new exercises.
After Six Months
By this stage, many patients are fully integrated into their daily routines without significant pain or limitations. Regular check-ups with your doctor are however essential to monitor your progress.
At KCM Clinic, we use a comprehensive approach to ensure that the hip replacement recovery time is optimised. Our professionals are always ready to guide you through every step, ensuring a safe and speedy recovery.
Hip Replacement Recovery Week By Week
Week 1: In the initial week, managing pain and swelling is the focus. Gentle range-of-motion exercises will be introduced. Avoid overexerting yourself.
Week 2: By the end of the second week, you’ll likely transition to using a cane. Your physical therapy will intensify, aiming to improve strength and flexibility.
Weeks 3 & 4: You might start light household chores and short outdoor walks. Hip stiffness should decrease, and your sleep patterns may begin to normalise.
Weeks 5 & 6: By now, many individuals feel more comfortable and confident. You might start driving, but it is recommended to always consult your surgeon before doing so.
Weeks 7 & 8: Strength continues to return. More exercises may be added, and you might be able to return to work, depending on the nature of your job.
Weeks 9 & 10: You should notice a significant improvement in your movement and flexibility. However, avoid any high-impact activities.
Weeks 11 & 12: During this time, many patients are largely able to perform all their daily activities, albeit with some precautions.
At KCM Clinic, we emphasise the importance of patience during your hip replacement recovery. Each individual’s recovery time for hip replacement can vary. Our team is dedicated to ensuring that your total hip replacement recovery week by week is a success story.
Complications To Watch Out For After Hip Replacement Surgery
After undergoing hip replacement, most people anticipate a smooth recovery. However, it’s vital to be vigilant and watch out for potential complications to ensure your hip replacement recovery is successful.
- Infection: Signs include increased redness or swelling at the surgical site, drainage, fever, and chills.
- Blood clots: Symptoms might encompass swelling and pain in the legs, especially the calf.
- Dislocation: If the new joint moves out of place, you might experience severe pain and inability to move the hip.
- Difference in leg length: One leg might feel longer than the other after surgery.
- Wear and loosening: Over time, the artificial hip joint may wear out or loosen.
At KCM Clinic, patient safety is our top priority. Our expert team constantly monitors post-operative patients for any signs of complications. We believe that early detection and timely intervention are crucial for a successful hip replacement recovery.
Pain After Hip Replacement Surgery
Pain is a natural part of the healing process after any surgery, including hip replacement. Most patients will experience some pain after the procedure, but it’s usually manageable with medications. The pain typically decreases over time and can be alleviated by:
- following your physical therapy regimen
- applying cold packs to the affected area
- elevating your leg to reduce swelling
- using over-the-counter pain relievers as directed
- following your surgeon’s advice on movement restrictions
At KCM Clinic, we emphasise the importance of pain management in ensuring a swift and effective total hip replacement recovery week by week. Our medical staff works closely with each patient to tailor pain management strategies, ensuring comfort and facilitating the hip replacement recovery timeline.
Recovery in Older Vs. Younger People
Age can influence the recovery time for hip replacement. Here’s what to expect:
Younger Individuals
They might have a more aggressive hip replacement recovery timeline due to better overall health and muscle tone. They often resume activities faster and may push the boundaries of their new hip sooner. However, they should be cautious and avoid overexertion, which could compromise the new joint.
Older Individuals
The recovery might be more gradual. Elderly patients may require additional assistance and a longer duration of physical therapy. The focus should be on safety to prevent falls and subsequent injuries.
Regardless of age, the key is to stay active within the recommended limits. Physical therapy is vital in both groups to restore strength and flexibility and to optimise the hip replacement recovery time.
At KCM Clinic, we recognise that each individual is unique. Age, health status, and other factors contribute to the varied recovery time for hip replacement. We are dedicated to providing personalised care, ensuring that every patient, young or old, navigates the hip replacement recovery process with the utmost support and expertise.
Schedule a free consultation with our coordinator
I hereby agree to the Privacy Policy and the utilization of the data provided by filling out the form.
Hip Replacement Recovery FAQs
- How long does it take to walk normally after hip surgery?
The hip replacement recovery timeline varies, but typically, most patients begin walking with assistance within days, and by 6-12 weeks, most people can walk without using any aid. At KCM Clinic, we emphasise early mobility to ensure an efficient hip replacement recovery time.
- How long are you on bed rest after a hip replacement?
After a hip replacement surgery, bed rest is usually minimal to promote early mobility and reduce complications. Therefore, physiotherapy is usually started within 24-48 hours to ensure safe movement.
- What are permanent restrictions after hip replacement?
Permanent restrictions post-hip replacement typically involve high-impact activities and certain extreme motions that strain the joint. However, it is essential to consult your surgeon for a detailed list, as individual recommendations may differ.
- What can you never do again after a hip replacement?
Following a hip replacement, high-impact sports, deep squatting, or extreme hip flexion might be discouraged. However, every patient’s total hip replacement recovery is unique, and so restrictions can vary. It’s always best to consult your orthopaedic surgeon for personalised guidance.
- https://www.spirehealthcare.com/health-hub/specialties/bones-and-joints/hip-replacement-recovery-timeline-tips-and-information/
- https://www.webmd.com/osteoarthritis/ss/slideshow-hip-surgery-recovery-timeline
- https://www.healthline.com/health/hip-replacement-recovery
- https://www.medicalnewstoday.com/articles/hip-replacement-2

Author: Krzysztof Czerkasow
A graduate of the Faculty of Medicine at the Wrocław Medical University (Poland). He received his medical degree in 1976. He successively completed the first and second levels of specialty training in trauma and orthopedic surgery in 1980 and 1983. He gained experience in English hospitals. At William Harvey Hospital in Ashford, UK, he reached the rank of consultant

Privacy Overview

Revitalize Your Steps: A Comprehensive Guide to Physical Therapy Post-Hip Replacement
by Dr. Veronica Jow | Jan 19, 2024 | Physical Therapy
Hip replacements are common, especially among active adults and seniors. This surgical procedure, aimed at relieving pain and improving mobility, involves replacing a damaged hip joint with a prosthetic implant. However, the journey to full recovery doesn’t end in the operating room. Physical therapy is a vital part of this journey, ensuring that you make the most out of your new hip and return to your daily activities safely and effectively.
At Avid Sports Medicine in San Francisco, we understand that each patient’s journey is unique. That’s why we emphasize personalized care and evidence-based practices in our physical therapy programs. Whether you’re an athlete, a weekend warrior, or someone looking to enjoy pain-free movements, our guide is designed to provide you with valuable insights and practical tips to navigate the post-operative phase with confidence.
Understanding Hip Replacement
Embarking on a hip replacement journey can be a significant decision, and we’re here to help you understand every aspect of this process. Hip replacement surgery, also known as hip arthroplasty, is a procedure where a damaged or worn-out hip joint is replaced with an artificial implant. This surgery is a common solution for those suffering from hip pain and mobility issues, often due to arthritis or injury.
Why Choose Hip Replacement?
The primary goal of hip replacement is to alleviate pain and enhance your quality of life. When non-surgical treatments like physical therapy, medications, or lifestyle changes no longer provide relief, hip replacement surgery becomes a viable option. It’s designed to restore mobility and enable you to return to your everyday activities without the hindrance of hip pain.
The Procedure Explained
In a typical hip replacement surgery, the surgeon removes the damaged cartilage and bone from your hip and replaces it with artificial components. These components include a socket (made of durable plastic, ceramic, or metal), which is implanted into your pelvic bone, and a ball component, which replaces the rounded top of your thigh bone (femur). This ball-and-socket mechanism mimics the movement of a natural hip joint.
Types of Hip Replacements
There are different types of hip replacement surgeries, and the choice depends on various factors like your age, health, and lifestyle. The most common types are:
- Total Hip Replacement: Both the ball and socket of the hip joint are replaced. This is the most common type and is highly effective for those suffering from severe hip deterioration.
- Partial Hip Replacement: Only the ball part of the joint is replaced. This is often recommended for older patients with hip fractures.
- Minimally Invasive Hip Replacement: A variation of the total hip replacement, but involves smaller incisions and less muscle disturbance, leading to potentially quicker recovery times.
- Hip Resurfacing: A bone-preserving alternative to total hip replacement, suitable for younger, more active patients.
Recovery and Physical Therapy
Recovery from hip replacement surgery varies from person to person, but physical therapy is a crucial component. A well-planned physical therapy regimen, tailored to your individual needs, can significantly impact the speed and success of your recovery. Physical therapy starts soon after surgery – often within the first day. It focuses on improving hip strength, flexibility, and overall mobility, ensuring that you can return to your daily activities safely and effectively.
The Role of Physical Therapy in Recovery
After a hip replacement surgery, the journey to full recovery truly begins, and physical therapy plays a starring role in this process. At Avid Sports Medicine, we believe that a well-structured physical therapy program is crucial for a successful recovery. Here’s how physical therapy can make a difference in your post-surgery life.
Accelerating Recovery Post-Surgery
Physical therapy starts almost immediately after hip replacement surgery – sometimes as soon as the same day or the next. Early movement is key to preventing complications such as blood clots and to promote healing. The initial exercises are gentle and aimed at gradually increasing your hip mobility.
Customized Physical Therapy Plans
Every individual’s recovery journey is unique. That’s why we develop personalized physical therapy plans. These plans take into consideration your specific surgical procedure, health history, and personal recovery goals. Tailoring your physical therapy ensures that you are on the most efficient path to regaining strength and mobility.
Building Strength and Mobility
A significant focus of physical therapy after hip replacement is to strengthen the muscles around the new hip joint and improve flexibility. This is crucial for regaining your ability to perform daily activities such as walking, climbing stairs, and eventually returning to more strenuous activities like sports or hiking.
Reducing Pain and Swelling
Physical therapy techniques also play a vital role in pain management and reducing swelling post-surgery. Through various exercises, stretching routines, and sometimes modalities like ice or heat, our therapists at Avid Sports Medicine help you manage discomfort and accelerate your healing process.
Preventing Post-Surgical Complications
A critical aspect of physical therapy is to help prevent complications that can arise after hip surgery. This includes educating patients on how to move correctly, positioning techniques to prevent dislocation of the new hip joint, and exercises to maintain blood circulation.
Restoring Confidence in Movement
Beyond the physical benefits, physical therapy is instrumental in restoring your confidence in your body’s abilities. Our therapists support you every step of the way, encouraging you to push your limits safely and regain your independence.
Continual Assessment and Adjustment
Your physical therapy journey is dynamic, with ongoing assessments to track your progress. As you improve, your therapist will adjust your exercises to continuously challenge and strengthen your hip. This ongoing customization ensures that you are always working towards optimal recovery.
Initial Phase of Physical Therapy
Embarking on the initial phase of physical therapy after your hip replacement surgery is a crucial step in your recovery journey. At Avid Sports Medicine, we understand the importance of starting off on the right foot. This early stage of physical therapy is all about laying a strong foundation for a successful recovery. Here’s what you need to know about the initial phase of your physical therapy.
Starting with the Basics
The initial phase of physical therapy typically begins within the first 24 to 48 hours post-surgery. This early intervention is vital to kickstart your healing process. The goals here are straightforward – to promote blood circulation, prevent blood clots, and begin gentle movements to aid in your hip recovery.
Gentle Exercises and Movements
During these first days, your physical therapy will consist of light exercises. These might include ankle pumps, gentle leg lifts, and careful walking with assistance. The idea is to engage your muscles without straining your new hip joint. At Avid Sports Medicine, our therapists guide you through each movement, ensuring that you perform them correctly and safely.
Pain Management Strategies
Managing pain and discomfort is a significant part of the initial phase of physical therapy. We employ various techniques, such as ice therapy, gentle stretching, and careful movements, to help manage pain and reduce inflammation. It’s important to communicate with your therapist about your pain levels, so they can adjust your therapy plan accordingly.
Building Confidence in Movement
This early phase is also about building your confidence in moving again. It’s normal to feel a bit anxious about moving your new hip, but gentle, guided exercises will help you overcome this. Our therapists are experts in helping patients regain trust in their body’s ability to move without pain.
Education on Safe Movements
An essential component of your early physical therapy is education. Our therapists will teach you how to move safely to protect your new hip. This includes instructions on how to sit, stand, and lie down correctly, as well as how to safely perform everyday activities.
Setting the Stage for Advanced Therapy
The initial phase is just the beginning. As you progress, your physical therapy sessions will gradually become more challenging. This phase sets the stage for more advanced exercises and activities that will further strengthen your hip and improve your mobility.
Regular Monitoring and Feedback
Throughout your initial phase of physical therapy, regular monitoring and feedback from our therapists at Avid Sports Medicine are crucial. This allows us to track your progress and make necessary adjustments to your therapy plan, ensuring that you’re always moving forward in your recovery.
Advanced Physical Therapy Techniques
As you move forward in your recovery journey post-hip replacement surgery, it’s time to embrace the advanced phase of physical therapy. At Avid Sports Medicine, we’re dedicated to guiding you through this crucial stage with advanced techniques designed to restore your strength, improve flexibility, and enhance your overall mobility.
Building Strength and Endurance
In this advanced phase, the focus shifts to building the strength and endurance of your hip muscles and surrounding areas. You’ll engage in exercises that are more challenging than those in the initial phase. These may include leg presses, squats, and exercises using resistance bands. The aim is to gradually increase the resistance and intensity of your workouts, ensuring continuous improvement in muscle strength and joint stability.
Enhancing Mobility and Flexibility
Enhanced mobility and flexibility are key to a successful recovery. Our therapists will introduce a range of motion exercises and stretching routines targeting not just your hip but also the lower back, knees, and ankles. These exercises are crucial for regaining a full range of motion in your hip and for promoting overall body coordination and balance.
Balance and Gait Training
A significant aspect of advanced physical therapy is balance and gait training. This involves exercises that help improve your ability to stand, walk, and move around safely and confidently. Techniques such as walking on different surfaces, stair climbing, and using balance equipment are incorporated to restore your natural walking pattern and prevent falls.
Consistency and Regular Assessment
Consistency is key in this phase of your recovery. Regular physical therapy sessions, combined with exercises at home, are vital for achieving the best results. At Avid Sports Medicine, we continually assess your progress, adjusting your therapy plan as needed to ensure that you are always on track towards full recovery.
Incorporating Functional Movements
As you progress, we integrate functional movements into your therapy sessions. These are movements that mimic your daily activities, like bending to pick something up or reaching overhead. The goal is to prepare you to return to your everyday life, including work and leisure activities, without discomfort or limitations.
Use of Advanced Physical Therapy Equipment
In this stage, we may also utilize advanced physical therapy equipment. This can include treadmills, stationary bikes, and other machinery designed to aid in recovery. These tools help fine-tune your strength, endurance, and mobility, offering a comprehensive approach to your rehabilitation.
Emphasis on Patient Education
An informed patient is an empowered patient. Throughout your advanced physical therapy, we place a strong emphasis on education. Understanding the mechanics of your new hip, the do’s and don’ts, and how to manage any discomfort or unusual sensations ensures that you remain proactive in your recovery.
Long-Term Recovery and Maintenance
After progressing through the initial and advanced stages of physical therapy following your hip replacement surgery, you’ve reached an important milestone – long-term recovery and maintenance. At Avid Sports Medicine in San Francisco, we’re committed to helping you maintain and enhance the gains you’ve made, ensuring a healthy and active lifestyle. Let’s delve into the strategies and practices essential for long-term success.
Sustaining Strength and Mobility
Long-term recovery focuses on maintaining and further improving the strength and mobility you’ve worked hard to achieve. Regular engagement in low-impact exercises like walking, swimming, or cycling is beneficial. These activities not only keep your muscles strong but also ensure that your hip joint remains flexible and functional.
Incorporating Lifestyle Changes
Your journey doesn’t end with physical therapy. Incorporating certain lifestyle changes can significantly impact the longevity of your hip replacement. This includes maintaining a healthy weight, engaging in regular physical activity, and adopting a balanced diet. These changes not only support your hip health but also contribute to overall well-being.
Ongoing Exercise Regimen
An ongoing exercise regimen tailored to your needs is crucial. This might include a mix of strength training, flexibility exercises, and balance activities. Remember, the goal is to keep your muscles strong and your joints limber to prevent stiffness and maintain mobility.
Monitoring Progress and Health
Regular check-ins with your healthcare provider and physical therapist are important. These appointments are opportunities to assess your hip’s condition, address any concerns, and make adjustments to your exercise routine if necessary. It’s also a time to discuss any new activities or sports you’re considering.
Knowing When to Seek Medical Advice
Awareness of your body and understanding when to seek medical advice is essential. If you experience increased pain, swelling, or any unusual symptoms in your hip, it’s important to contact your healthcare provider. Early intervention can prevent complications and ensure the longevity of your hip replacement.
Continuous Learning and Adaptation
The field of physical therapy and hip care is always evolving. Staying informed about new exercises, techniques, and lifestyle recommendations can provide additional benefits to your long-term hip health. At Avid Sports Medicine, we encourage ongoing education and adaptation to new, evidence-based practices.
Community and Support
Finally, remember that you’re not alone in this journey. Engaging with a community of individuals who have undergone similar experiences can be incredibly supportive. Whether it’s through support groups, online forums, or community events, sharing experiences and tips can be both enlightening and encouraging.
Potential Challenges and Solutions
Recovering from hip replacement surgery is a journey that comes with its own set of challenges. At Avid Sports Medicine, we understand that being prepared for these challenges and knowing how to effectively address them can make a significant difference in your recovery. Here, we’ll explore some common hurdles you might face and provide practical solutions to overcome them.
Challenge 1: Managing Post-Surgery Pain
Solution: Pain management is a key aspect of recovery. It’s important to follow your pain medication schedule as prescribed by your doctor. Additionally, incorporating gentle exercises and applying heat or cold therapy can help alleviate discomfort. If pain persists or worsens, it’s crucial to consult with your healthcare provider.
Challenge 2: Limited Mobility in the Early Stages
Solution: Initially, you may find your mobility is quite restricted. Regular physical therapy sessions are essential to gradually improve your range of motion. Use assistive devices like walkers or canes as recommended by your therapist. Remember, it’s a gradual process, and patience is key.
Challenge 3: Fear of Moving the New Hip Joint
Solution: It’s common to feel apprehensive about moving your new hip joint. Working closely with your physical therapist can help build confidence in your hip’s capabilities. Start with low-impact exercises and gradually increase intensity as you become more comfortable.
Challenge 4: Swelling Around the Hip Area
Solution: Swelling is a normal part of the healing process. To reduce swelling, elevate your legs when sitting and apply ice packs as instructed by your therapist. Keep moving within your comfort level, as activity helps reduce swelling.
Challenge 5: Difficulty Returning to Normal Activities
Solution: Returning to your normal routine takes time. Incorporate the exercises and techniques learned during your physical therapy sessions into your daily routine. Set realistic goals and celebrate small victories along the way.
Challenge 6: Long-term Maintenance of Hip Health
Solution: Maintaining the health of your new hip joint is a lifelong commitment. Continue with a regular exercise regimen, maintain a healthy weight, and follow up with your healthcare provider for regular check-ups. Stay informed about new exercises or lifestyle changes that can benefit your hip health.
Challenge 7: Emotional and Mental Health Concerns
Solution: It’s important to acknowledge the emotional and mental aspects of recovery. If you’re feeling down, anxious, or frustrated, don’t hesitate to talk about it with your healthcare team, a counselor, or support groups. Remember, mental health is just as important as physical health in your recovery journey.
Your Path to Recovery Starts Here
Recovering from hip replacement surgery is not just about physical healing; it’s about reclaiming your mobility and enjoying a better quality of life. Whether you’re taking your first steps in recovery or are looking to enhance your long-term hip health, Avid Sports Medicine is here to guide you.
Free Consultation Call : Take the First Step Today
We invite you to take the first step towards a successful recovery by booking a free consultation call with us. This call is an opportunity to discuss your specific needs, ask questions, and learn how our tailored physical therapy programs can aid in your recovery. Our team of experienced therapists is dedicated to helping you achieve your goals, whether it’s returning to daily activities, sports, or simply enjoying a pain-free life.
Your Journey, Our Commitment
At Avid Sports Medicine, your journey is our commitment. We believe in providing not just expert care but also a supportive environment where you can confidently work towards regaining your strength and independence. Let us be part of your journey to a new and improved quality of life.
To schedule your free consultation, visit our website or contact us directly. We’re here to help you step confidently into your new chapter of mobility and wellness. Remember, your path to recovery and a more active life starts with Avid Sports Medicine in San Francisco.
Recent Blog Posts
- Will Physical Therapy Help A Torn Rotator Cuff
- Will Physical Therapy Help Spinal Stenosis?
- Physical Therapy After Hip Replacement
- Physical Therapy For Plantar Fasciitis
- The Benefits of Physical Therapy
- Hip Surgery & Replacement
- SMART Total Hip Replacement
- Direct Anterior Approach (DAA) Hip Replacement
- Knee Surgery & Replacement
- Robotic Knee Replacement
- Shoulder Surgery & Replacement
- Elbow Surgery & Treatment
- Hand and Wrist Surgery & Treatment
- Foot and Ankle Surgery & Treatment
- Spine Care & Spinal Surgery
- Regenerative Medicine
- Sports Medicine
- Medical Tourism
- Auto Accident Recovery
- Workers’ Compensation
- Vladimir Alexander, M.D.
- John Constantino, D.P.M.
- Jonathan Dattilo, M.D.
- Adam Kopiec, M.D.
- Andrew Mundy, M.D.
- Charles Nalley, M.D.
- Thomas E. Odmark, M.D.
- Daniel Penello, M.D.
- Adam Perler, D.P.M.
- Jennifer Swaringen, M.D.
- Scott Vizzi, M.D.
- Ali Zahrai, M.D.
- Physician Assistants
- Physical Therapists
- Patient Portal
- Patient Forms
- Pay My Bill
- Insurance Information
- Preparing for Surgery
- The Alexander Outpatient Advantage
- Patient Stories
- Palm Harbor
- St. Petersburg
- Career Opportunities
- Schedule an Appointment
How to Stretch Safely After a Hip Replacement
A guide to safe stretching after hip replacement surgery.
Hip replacement surgery offers improved mobility and relief from chronic pain for many individuals. However, the journey to recovery doesn’t end in the operating room; it continues with postoperative care and rehabilitation exercises like stretching.
If you’ve recently undergone a hip replacement or are supporting a loved one through their recovery process, you may be wondering how to safely incorporate stretching into your postoperative routine. Use our expert guide for advice and insights to help you safely navigate the path to a more flexible and pain-free future.
Benefits of Stretching After a Hip Replacement Surgery
It is generally safe to engage in stretching exercises after a hip replacement. Stretching after hip replacement surgery offers numerous benefits. It helps to promote flexibility , improve joint function, reduce stiffness, and enhance overall mobility. Additionally, targeted stretches can aid in muscle strength and balance, which can contribute to a smoother recovery process, prevent postoperative complications, and facilitate a quicker return to daily activities.
How Soon Can I Start Stretching After a Hip Replacement for Maximum Benefits?
You can start gentle, supervised stretches immediately after your hip replacement. However, it’s crucial to follow your surgeon’s and physical therapist’s guidance. Initially, focus on simple movements and gradually progress to more extensive stretches as your healing progresses.
Recommendations for Stretching Safely After a Hip Replacement
To stretch safely after a hip replacement, follow the regime and guidance laid out by your physical therapist. Start with gentle, controlled movements. Prioritize proper technique, avoid overstretching, and progress gradually. Above all, listen to your body, and if you experience pain or discomfort, consult your healthcare team for personalized advice.
How Often Should I Stretch?
In the early stages of recovery, aim for gentle stretches 3-4 days per week, gradually increasing frequency as your hip heals. As you progress, consult your surgeon or a physical therapist to determine an optimal stretching frequency based on your individual progress and specific rehabilitation needs. Generally, you only need to stretch during physical therapy or first thing in the morning if you are feeling stiff after sleeping. However, stretches can be done everyday or several times a day if your muscles are feeling tight.
How Long Should I Hold Each Stretch?
Hold each stretch for 15-30 seconds, allowing the muscles to lengthen and improve flexibility. Avoid bouncing or forcing the stretch. Gradually increase the duration as your comfort level improves. As you improve, you can build up to multiple repetitions. Always prioritize quality over quantity, and consult your physical therapist for personalized recommendations based on your recovery progress.
How Do I Know If I’m Stretching Too Much?
Pain or soreness while stretching is your body’s attempt to tell you to slow down. Therapy after a hip replacement should not involve pushing through pain. Remember you just had surgery, and pushing through discomfort is often more likely to set you back than it is to facilitate progression in your recovery.
What Stretches are Safe After a Hip Replacement?
Any stretching is safe after a hip replacement. However, gentle movements to improve flexibility and strength are recommended. Begin with knee-to-chest stretches, ankle pumps, and heel slides. As you progress, incorporate hip flexor and quadriceps stretches. Always adhere to your surgeon’s recommendations and avoid overstretching or sudden, intense movements.
Try the following stretches to allow your body to naturally and safely progress in motion. Remember to perform these stretches in a controlled manner, avoiding any jerky or forceful movements. Always listen to your body, and if you experience pain or discomfort, consult your healthcare team before continuing or modifying your stretching routine.
Knee-to-Chest Stretches
Begin by lying on your back with both legs extended. Slowly bring one knee toward your chest, holding it with both hands for 15-30 seconds. Repeat with the other leg. This stretch helps increase flexibility in the hip and lower back.
Ankle Pumps
While lying on your back or sitting with your legs extended, gently move your ankles up and down, mimicking a pumping motion. This simple exercise promotes blood circulation and helps prevent stiffness in the ankles.
Heel Slides
While lying on your back, bend one knee and slide the heel along the surface toward your buttocks. Hold for a few seconds, then straighten the leg back out. This movement aids in improving the range of motion in your hip.
Hip Flexor Stretch
Kneel on one knee with the other foot in front, forming a 90-degree angle. Gently push your hips forward, feeling a stretch in the front of the hip of the kneeling leg. Hold for 15-30 seconds and switch legs. This stretch targets the hip flexors.
Quadriceps Stretch
While standing, hold onto a stable surface for support. Bend one knee, bringing your foot toward your buttocks, and grasp your ankle with your hand. Hold for 15-30 seconds and switch legs. This stretch focuses on the quadriceps and helps maintain muscle flexibility.
What Movements or Exercises Should Be Avoided After a Hip Replacement?
It is generally recommended that you avoid high-impact activities and exercises that involve excessive twisting or bending at the hip, such as deep squats or certain yoga poses, after your hip replacement. Steer clear of sudden, forceful movements and activities that may put excessive strain on the hip joint.
Hip Precautions for Stretching
Depending on the type of hip replacement you had, your surgeon may advise you to avoid certain positions or activities, known as hip precautions . The following list are some hip precautions to observe while stretching, but consult your surgeon for a comprehensive list tailored to your specific case.
- Avoid Deep Hip Bends: Refrain from deep bends or stretches, including deep squats, that might exceed the recommended hip flexion angle of 90 degrees.
- Skip Cross-Legged Stretches: Steer clear of stretches that involve crossing your legs as this can place stress on the hip joint.
- Use Supportive Props: Make use of supportive props, such as pillows or cushions, to assist in maintaining proper alignment during stretching exercises.
- Don’t Twist: Avoid stretches that involve excessive twisting of the hips. You do not want to strain the healing hip joint.
Are there Lifelong Restrictions After a Hip Replacement?
The biggest restriction after hip replacement surgery is to avoid falling. Falling can cause damage to the prosthesis or surrounding bone. Aside from that risk, there are no other permanent restrictions once you have recovered from your hip replacement. You’ll be able to resume an active lifestyle, including activities like playing golf or tennis. Some patients, with guidance from their surgeon, are even able to resume higher impact activities like running, skiing, or surfing.
What Should I Do if I Experience Pain While Stretching?
If you experience pain while stretching after a hip replacement, stop the activity immediately. Use your pain as a guide. Mild discomfort may improve with stretching, but more significant pain is your body’s warning that you are still recovering from an operation. If pain persists, consult your healthcare team. Pain may indicate overstretching or potential issues requiring professional evaluation and adjustment to your rehabilitation plan.
Hip Replacement Stretching and Recovery FAQs
When should i start physical therapy after a hip replacement.
Most hip replacement patients have a physical therapy session on the day of surgery, approximately 2 hours after their surgery concludes. This session focuses on safe ambulation with a walker. Formal physical therapy will begin 2-3 days after surgery and continues for 4-6 weeks.
How Long Does it Take For Stiffness to Go Away After a Hip Replacement?
Hip replacement surgery is designed to replace the worn out bone and cartilage with a prosthetic interface and that allows for increased motion. As a result, many patients notice immediate improvement in their stiffness and range of motion after surgery. In general, swelling from surgery subsides over the first 2-4 weeks, which also helps increase overall mobility.
Are Yoga Poses Safe After a Hip Replacement?
Yes. Many yoga poses are safe after a hip replacement, but It is advised that you wait 4 weeks before resuming yoga practice. You want to ensure that the swelling in your hip has subsided before attempting more strenuous yoga exercises. Consider starting with gentle stretches and implement modifications to support flexibility without straining your hip joint.
Can I Sit with My Legs Crossed After a Hip Replacement?
Avoid sitting with your legs crossed immediately after hip replacement surgery. The cross-legged position can strain the healing joint and hinder your recovery process. As your stiffness resolves and your postoperative pain subsides, you will be able to sit with your legs crossed.
Can I Swim After a Hip Replacement?
Yes. Swimming is often a beneficial exercise after a hip replacement. It provides low-impact, gentle resistance, promoting joint mobility and overall fitness. However, wait at least 4 weeks after your hip replacement before swimming in order to give your surgical incision the appropriate time to heal.
Can I Sleep on My Side After a Hip Replacement?
Yes. It is safe to sleep on your side after a hip replacement, but you may not want to do this immediately due to the pain. Some types of hip replacements also have an incision located on the outside of your hip that may be uncomfortable until the wound has healed. As your pain eases, you may lay on your hip without fear of damaging the prosthesis.
Can I Sit in a Recliner After a Hip Replacement?
Yes. It is safe to sit in a recliner after a hip replacement, especially if it provides comfort and support during your recovery. It is recommended that you ensure the recliner is at an appropriate height to minimize strain on the hip joint. Follow your surgeon’s advice, and use additional cushions or supports if needed for optimal comfort and alignment.
Recover Safely From Hip Replacement Surgery at Alexander Orthopaedic Associates
Safely recover from your hip replacement surgery or have your hip pain evaluated at Alexander Orthopaedic Associates. Our team is dedicated to your well-being, providing personalized recommendations, safe stretching protocols, and ongoing support. Trust in our experience to guide you through a successful and comfortable hip surgery, replacement, treatment, and recovery and schedule your appointment today.

Hip replacement recovery guide: week-by-week
For those suffering from persistent hip pain, hip replacement surgery can significantly improve mobility and quality of life. It is considered by consultants to be a major surgery, so if hip surgery is on the cards for you, it’s crucial to follow your healthcare professional’s post-surgery advice. This can help to ensure you make a full and fast recovery. This guide is designed to help you navigate your hip replacement recovery and help ensure the best outcome after your surgery.

Private hip replacement surgery at a glance:
- Surgery within 4-6 weeks
- Costs just £10,720
- Available at a range of our UK locations
- Finance options available
Call us on 0333 321 1961
How long is the recovery from hip replacement?
The recovery period after hip replacement surgery varies depending on the following factors:
- your health
- the type of hip surgery you need
- how closely you follow your rehabilitation programme.
By following your physiotherapy plan, you can expect to resume regular activities within two to three months of surgery. The time it takes to fully benefit from your new hip depends on how closely you follow your recovery plan. The average expected time can be up to a year, however, this will depend on the rehabilitation work you do on the muscles around the hip. Making sure these are strong will help ensure the hip returns to a good range of motion.
Hip surgery recovery times for elderly patients
Older patients are more likely to experience slower healing and reduced mobility compared to younger patients. This can make recovery slower but the overall health and mobility of the patient will play a big part.
Recovery from minimally invasive hip replacement surgery
Minimally invasive hip replacement is when the surgeon makes one or more shorter incisions over the hip. Recovery from minimally invasive hip replacement surgery is generally quicker and less intense compared to traditional open surgery.
This technique may not be suitable for all patients.
Hip replacement recovery timeline
We’ve looked at how long recovery can take, now it’s time to explore in further detail what recovery might look like on a more detailed basis.
One-to-three days after a hip replacement
The initial recovery phase typically takes place in hospital. The average hospital stay following hip replacement ranges from one to three days. During this time, pain management, monitoring, and physiotherapy are provided to help you regain strength and mobility.
If you have a hip replacement at a Practice Plus Group hospital, once the operation is over, our physiotherapists will begin working closely with you. This happens within hours of joint replacement surgery and often means you’ll be able to return home as soon as possible. Early and gentle movement can also reduce the risk of complications after surgery such as blood clots.
One-to-six weeks after surgery
Once you return home, the first few weeks are crucial for healing and adjusting to your new hip. Pain and discomfort should gradually decrease during this period. Physiotherapy will improve your range of motion, help you regain strength, and encourage regular movement.
Six-to-twelve weeks after a hip replacement
During this phase, you should experience a significant reduction in pain while your mobility improves. Physiotherapy continues to focus on increasing strength, balance and flexibility. Most patients will be able to gradually resume light activities. They should also be able to return to work if their job is not physically demanding.
Three-to-six months after a hip replacement
At this stage, pain and swelling further decrease while mobility significantly improves. Physiotherapy continues to focus on enhancing strength, endurance, and stability. Activities such as walking, swimming and low-impact exercises become more manageable.
Six months to one year after a hip replacement
By this stage, most people experience significant improvements in mobility and reduced pain
While individual experiences may vary, many people will be able to resume normal activities. These include higher-impact exercises and sports. Physiotherapy may still be ongoing at this point. The focus will likely be on maintaining strength, flexibility, and optimal joint function.
It’s important to gradually reintroduce daily activities such as driving, work, and household chores as advised by your surgeon. Follow their guidelines regarding timelines and limitations.
Please note that, even though you might be able to return to higher-impact sports, these activities could speed up wear and tear of the implant.
Patient testimonial
“My hip pain had got to such a degree that it was waking me at night. From my first appointment at Practice Plus Group, it was an excellent experience.” Val Stones, hip replacement patient at Practice Plus Group Hospital, Shepton Mallet

Hip replacement recovery tips
Timelines and plans aside, the following tips can give you the best chance of a smooth hip surgery recovery:
- Book time off work : to encourage speedy recovery, make sure you book enough time off work following your surgery
- Prepare your home : your living space should be changed to ensure a safe and comfortable recovery. Arrange necessary equipment (such as a raised toilet seat, grab bars, and a stable chair with armrests) to make everyday living easier
- Hip pain management : follow your surgeon’s prescribed pain management plan. This may include medication, ice packs or heat therapy
- Physiotherapy : be sure to attend all your sessions. This will help you regain mobility and strength in your hip. Work closely with your physiotherapist to learn proper exercises and techniques to facilitate a smooth recovery
- Walking aids : use assistive devices like crutches or a walking stick as recommended by your surgeon and physiotherapist. Gradually transition to using them less as your strength improves
- Incision care : follow your surgeon’s instructions regarding incision care to minimise the risk of infection. Keep the incision clean and dry and avoid any activities that could irritate or disrupt the healing process
- Gradual weight-bearing : your surgeon will provide guidelines on when and how much weight you can put on your new hip. Initially, you may need to use assistive devices and gradually transition to full weight-bearing based on your surgeon’s instructions
- Follow post-operative guidelines : adhere to your surgeon’s post-operative guidelines regarding activity restrictions, medication usage and wound care. Report any unusual symptoms or concerns to your healthcare provider
- Gradual increase in activity : begin with gentle exercises and gradually increase your activity level as advised by your physiotherapist. Follow a structured rehabilitation program to regain flexibility, strength, and range of motion in your hip
- Nutrition and hydration : maintain a balanced diet rich in nutrients and stay well-hydrated to support the healing process. Consult with your healthcare provider for dietary recommendations tailored to you
- Rest and sleep : rest and sleep will help with the healing process. Practise good sleep hygiene by maintaining a comfortable sleep environment and following a regular night time routine
- Exercise and physical activity : when safe to do so, try regular low-impact exercises, such as swimming or cycling. This will help you maintain overall fitness and hip strength. Ask your healthcare provider for exercise recommendations
- Follow-up appointments : attend all follow-up appointments with your surgeon to monitor your progress, assess your healing, and address any concerns or complications.
Best exercises for hip replacement recovery
Walking, stationary cycling, and swimming are great low-impact forms of exercise that can help your recovery. It’s also important to follow your physio plan to gain strength. Your physio may recommend exercises such as:
- heel raises
- heel slides
- ankle circles
- single leg stand
Remember to consult your healthcare provider or physiotherapist before returning to sport and exercise after a hip replacement !
Pain in your hip?
If you’re experiencing hip pain, try our hip suitability quiz. It will give you an idea of whether you’d benefit from booking a consultation with one of our hip specialists.
Our enhanced recovery programme for hip replacement patients
At Practice Plus Group Hospitals, we’re passionate about giving patients a positive experience with personalised care every step of the way.
We practise the Enhanced Recovery Pathway (ERP). This is a modern, evidence-based approach that helps people speed up their recovery following major surgery. With this support you will be mobile enough to go home one or two days after your self-pay hip operation , some people are able to return home on the day of surgery.
It’s important to remember that the recovery process after hip replacement surgery is unique to each patient. Follow the guidance provided by your surgeon and healthcare team and listen to your body’s needs throughout the recovery journey. By following these guidelines and committing to your rehabilitation program, you can optimise your recovery and enjoy the benefits of improved hip function and mobility.
Hip operation recovery FAQs
Not quite found the information you’re looking for? Our dedicated hip replacement recovery FAQs can help.
Most patients can resume regular activities within two to three months. It can take up to a year to fully benefit from your new hip. This depends on how closely you follow your recovery plan.
While there’s no guaranteed “fastest” way to recover, you can maximise the chance of a complication-free recovery by reading the guidelines and tips on this page. Always follow the instructions and recommendations of your healthcare provider for optimal post-surgery results.
Hip replacement recovery can involve varying levels of pain and discomfort. However, advances in surgical techniques, anaesthesia, and pain management have significantly improved the overall experience for many patients. Be sure to follow the pain management instructions given to you by your surgeon and talk to your health provider if you are struggling to manage the pain.
One of the most frequent complications after hip replacement surgery is infection. That’s why it’s important to keep the incision area clean and dry. Minimise the risk of infection by following your surgeon’s instructions on wound care and medication.
Practice Plus Group hospitals have high levels of cleanliness and infection control. We also boast a 100% clean record for hospital-acquired infections.
Generally, you should expect to start walking (with the help of walking aids) within a few hours of your surgery. Typically, many patients can start walking unaided within four to six weeks of surgery. However, it’s important to note that individual experiences may differ.
Sitting on a sofa after hip replacement surgery is usually possible within the first few days of the procedure.
After hip replacement surgery, there are certain activities and movements that you should approach with caution. There are others you should look to avoid altogether to protect your new hip joint and ensure a successful recovery.
Consult your surgeon or physio before attempting these activities:
- high-impact activities (i.e. jumping)
- crossing your legs
- twisting at the hip
- squatting deeply
- high-risk sports (i.e. skiing)
You may be able to get back behind the wheel around six weeks post-operation. Always check with your doctor before driving again.
Returning to work will depend on the type of work you do. If your work is desk-based, you might be able to return as soon as six weeks after your operation. More physical roles could take a little longer.

Acknowledgements
- Share via Facebook
- Share via Twitter
- Share via Linkedin
- Select to copy URL Copied
Related resources

Benefits and risks of hip replacement

Gardening after a hip replacement

Hip replacement surgery in Derbyshire: a patient guide

Guide to hip replacement waiting times

What to Expect 2 Weeks After a Hip Replacement: Key Milestones and Tips

Undergoing a hip replacement can be a life-changing event for many individuals, leading to improved mobility and reduced pain. Within the first two weeks after the procedure, patients typically experience significant recovery progress. It is crucial to clearly understand what to expect during this initial stage of healing to prepare both physically and emotionally.

It is important to follow the guidance of the physical therapist and gradually progress to more challenging exercises tailored to the individual’s recovery and specific needs.
Using a Walker
During the first two weeks after hip replacement surgery, patients commonly use a walker to assist with mobility and stability. The walker helps to maintain a proper posture, reduce the amount of weight put on the newly operated hip, and prevent falls. Here are some tips on how to use a walker safely:
- Adjust the height of the walker, ensuring the handles are at wrist level when the arms are hanging down.
- Move the walker forward, keeping it close to the body while walking.
- Step with the surgical leg first, making sure the entire foot is flat on the ground before transferring weight onto it.
- Follow with the non-surgical leg, stepping slightly past the surgical leg.
During these initial stages of recovery, it is essential to maintain a consistent balance between exercising the hip and protecting the joint from injury. Patients should seek advice from healthcare professionals and follow their recommendations closely. By doing so, they can expect to gradually regain strength, range of motion, and overall function in their hip joint within the first few weeks after surgery.
Daily Activities 2 Weeks After a Hip Replacement
How far should you be walking.
Two weeks after a hip replacement surgery, you should be experiencing increased confidence and independence in walking. At this stage, you may still need a walking aid such as a cane, walker, or crutches, but you should be able to gradually increase the distance covered each day. Remember to continue doing the exercises prescribed by your physical therapist to help with flexibility and muscle tone 1 .
Showering and Personal Care
Two weeks post-operation, you should be able to manage most of your personal care activities, such as washing, showering, and dressing independently. However, you might still experience some pain and stiffness in your hip, so it’s important to be patient and not overexert yourself 2 .
We do recommend getting and using a shower chair during the first 2 weeks after a hip replacement. This makes sure that you don’t break hip surgical precautions while showering and gives you a break from standing during the first few days of recovery.
We recommend the Dr. Kays Adjustable Shower chair because it’s sturdy, lightweight, and adjustable.

Returning to Work
When it comes to returning to work, the timeline may vary depending on the nature of your job. If you have a desk job with minimal activity, you might be able to return to work after about two weeks. For jobs requiring heavy lifting or being tough on the hips, it is recommended to take around six weeks off to recover 3 .
As for driving, the decision to return should be based on your comfort level and mobility. It’s crucial to discuss your driving abilities with your doctor and physical therapist before getting behind the wheel. Make sure you can safely operate the vehicle and reach all necessary controls without causing pain or discomfort 4 .
- Activities After Total Hip Replacement – OrthoInfo – AAOS ↩
- Week Two – After Hip Replacement Surgery – totalhips.com ↩
- Hip Replacement Recovery Q&A | Johns Hopkins Medicine ↩
- Hip Replacement Recovery: Timeline and Tips for Best Outcome – Healthline ↩
Potential Complications After a Hip Replacement
Blood clots.
One potential complication after hip replacement surgery is the increased risk of developing blood clots in the legs. To prevent this complication, it is important for patients to start moving as soon as possible after the surgery. They will be encouraged to sit up and walk with the help of crutches or a walker soon after the procedure 1 . Other methods to prevent blood clots include:
- Taking prescribed blood-thinning medication
- Wearing compression stockings
- Performing ankle pump exercises
Nerve Damage
Another potential complication is nerve damage, which may occur during the surgery. This risk can manifest in several ways, such as:
- Numbness around the incision site
- Difficulty moving the affected leg
- Persistent pain
While nerve damage is a rare occurrence, it is essential for patients to be aware of this risk and report any unusual symptoms to their healthcare team. Monitoring the recovery and following the prescribed rehabilitation exercises can help in minimizing the risk of nerve damage during the healing process 2 .
In conclusion, being informed about potential complications such as blood clots and nerve damage can help patients take necessary precautions and work closely with their healthcare team during the recovery process.
- https://www.mayoclinic.org/tests-procedures/hip-replacement/about/pac-20385042 ↩
- https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/hip-replacement-recovery-qa ↩
Timeline of Recovery
Short-term milestones.
During the first two weeks after a hip replacement, patients can expect to see some key short-term milestones in their recovery. Initially, patients will work with a physical therapist to regain strength and mobility in the affected area [1] . Some recovery milestones within this period include:
- Standing and walking with assistance, typically within the first 24-48 hours after surgery
- Transitioning to walking with crutches or a walker
- Gradually increasing mobility and range of motion
- Managing pain and swelling through medication and ice
- Decreasing the use of narcotic pain medication
- Sleep longer before waking up each night
It’s important to note that individual recovery times can vary depending on factors such as age, preexisting health conditions, and level of activity prior to surgery [2] .
Full Recovery After a Hip Replacement
While short-term milestones are crucial for a successful recovery, achieving a full recovery usually takes longer. Many patients experience significant improvements around three months after surgery, but it’s not uncommon for the full recovery process to take up to a year or more [3] .
During this time, patients should continue attending physical therapy sessions and perform exercises at home to promote healing and increase mobility. Regular walking and gradually resuming daily activities are essential for a successful outcome, as well as maintaining a healthy lifestyle and monitoring the healing process with medical professionals [4] .
In summary, the timeline of recovery after a hip replacement includes short-term milestones, such as regaining mobility and managing pain, as well as ongoing efforts to achieve full recovery over a longer period of time. Each patient’s recovery process will be unique, and a clear communication line with healthcare providers is necessary for a successful outcome.
Patients can expect gradual improvements in the two weeks following a hip replacement surgery as their body adjusts to the new joint. Mobility and independence will steadily increase, and pain levels should decrease over time as they engage in physical therapy and follow their doctor’s advice. To get a clear idea of the recovery process, it’s helpful to break it down into the key aspects.
Physical Therapy
During the first two weeks, patients should engage in regular physical therapy sessions. This will help them regain strength, balance, and flexibility, thereby making day-to-day tasks easier to perform. They might start with simple exercises, such as ankle pumps or leg slides, before progressing to more challenging activities like walking with support. It’s essential to follow the therapist’s recommendations and be patient with the process, as full recovery may take several weeks or even months.
Pain Management
Pain levels should gradually decrease as the body heals. Initially, some discomfort may occur, but it should subside over time, reaching a low level within 12 weeks after surgery. If pain persists or intensifies, patients should consult their doctor, as this could be a sign of infection or other complications, as mentioned by Johns Hopkins Medicine .
Mobility and Independence
According to Medical News Today, patients are expected to move about more easily and without aid within the first two weeks. Those who previously required a cane or walker might now find themselves walking short distances with little to no assistance. By the end of the second week, many patients will have been discharged from the hospital and can perform most of their normal activities, as highlighted by Healthline .
As time progresses, the patient’s ability to perform daily tasks will continue to improve. Maintaining open communication with the healthcare team and engaging in physical therapy is crucial to ensure optimal recovery outcomes during this period. A proactive and committed approach to healing will likely result in a smoother and more rewarding hip replacement experience.
Related Posts

How to Sleep With Hip Bursitis: The Definitive Guide

Hip Labral Tear Pain with Sitting: What to Know

5 Reasons for Lateral Hip Pain: Expert Insights and Solutions

The Complete Guide to Using a Massage Gun for Hip Labral Tears

How to Do the Side Lying Clamshell Exercise (With Perfect Form)

Glute Minimus Tear: Non-Surgical Treatment Options Explained

Top 5 Stretches to Help Heal Your Gluteus Minimus Tear
1 thought on “what to expect 2 weeks after a hip replacement: key milestones and tips”.
Pingback: When Can You Walk After a Hip Replacement? - The Hip PT
Comments are closed.
ScienceSphere.blog
Mastering Mobility: How To Get Back In The Driver’s Seat After Hip Replacement

Hip replacement surgery is a common procedure that aims to alleviate pain and improve mobility in individuals with hip joint problems. This surgical intervention involves replacing the damaged or diseased hip joint with an artificial joint, known as a prosthesis. The recovery process after hip replacement surgery is crucial for regaining mobility and returning to an active lifestyle.
Table of Contents
Brief explanation of hip replacement surgery
Hip replacement surgery, also known as total hip arthroplasty, is a surgical procedure performed to replace a damaged or diseased hip joint with an artificial joint. The hip joint is a ball-and-socket joint that allows for smooth movement and stability. However, conditions such as osteoarthritis, rheumatoid arthritis, or hip fractures can cause severe pain and limit mobility, necessitating the need for hip replacement surgery.
During the procedure, the damaged parts of the hip joint are removed and replaced with a prosthetic implant made of metal, plastic, or ceramic materials. This artificial joint mimics the natural movement of the hip, allowing for improved mobility and reduced pain.
Importance of regaining mobility after surgery
Regaining mobility after hip replacement surgery is crucial for several reasons. Firstly, it allows individuals to perform daily activities independently, such as walking, climbing stairs, and getting in and out of chairs. Restoring mobility also enhances overall quality of life, as it enables individuals to engage in recreational activities, exercise, and social interactions.
Moreover, regaining mobility helps prevent complications associated with immobility, such as blood clots, muscle weakness, and joint stiffness. Physical activity promotes blood circulation, strengthens muscles, and improves joint flexibility, reducing the risk of post-surgery complications.
Furthermore, restoring mobility after hip replacement surgery can have a positive impact on mental well-being. Being able to move freely and engage in activities that were previously challenging or impossible can boost self-confidence, independence, and overall happiness.
In the following sections, we will explore the journey of regaining mobility after hip replacement surgery, including preparing for the recovery process, exercises for hip rehabilitation, overcoming challenges, returning to driving, maintaining long-term mobility, and concluding with key takeaways for readers.
Preparing for the Journey
After undergoing hip replacement surgery, it is crucial to prepare yourself for the journey of recovery. This phase is essential for regaining mobility and ensuring a successful outcome. By understanding the recovery process, setting realistic expectations, and making necessary preparations, you can make your post-surgery experience more comfortable and safe.
Understanding the Recovery Process
Before embarking on your recovery journey, it is important to have a clear understanding of the process. Hip replacement surgery involves the removal of damaged or diseased parts of the hip joint and replacing them with artificial components. The recovery period typically lasts several weeks to months, during which you will gradually regain strength and mobility.
During the initial days after surgery, you may experience pain, swelling, and limited mobility. However, as time progresses, these symptoms will gradually improve. It is important to follow your surgeon’s instructions and attend regular physical therapy sessions to aid in your recovery.
Setting Realistic Expectations
While hip replacement surgery can significantly improve your quality of life, it is important to set realistic expectations. Understand that the recovery process takes time and patience. You may not be able to resume all activities immediately after surgery, and it is important to listen to your body and not push yourself too hard.
Consult with your surgeon and physical therapist to understand the limitations and restrictions during the recovery period. They will provide you with guidelines on weight-bearing, activity levels, and precautions to take to ensure a smooth recovery.

Preparing Your Home for Post-Surgery Comfort and Safety
Before returning home after surgery, it is crucial to prepare your living space for post-surgery comfort and safety. Consider the following steps:
Clear pathways: Remove any obstacles or clutter that may hinder your mobility. Ensure that there are clear pathways throughout your home, especially in areas where you will be spending most of your time.
Install safety equipment: Install grab bars in the bathroom, near the toilet, and in the shower to provide support and stability. Consider using a raised toilet seat and a shower chair to make these activities easier and safer.
Create a comfortable resting area: Set up a comfortable and accessible resting area with pillows, blankets, and a recliner if necessary. This will allow you to rest and elevate your leg comfortably.
Arrange for assistance: If possible, arrange for a family member or friend to stay with you during the initial days after surgery. They can assist you with daily activities and provide emotional support.
By making these preparations, you can create a safe and comfortable environment that promotes a smooth recovery process.
Preparing for the journey of hip replacement surgery involves understanding the recovery process, setting realistic expectations, and making necessary preparations in your home. By following these steps, you can ensure a more comfortable and successful recovery, ultimately regaining your mobility and improving your quality of life.
Taking the First Steps
After undergoing hip replacement surgery, taking the first steps towards recovery can be both exciting and challenging. It is crucial to approach this phase with patience and a well-structured plan. In this section, we will explore the key aspects of taking the first steps towards regaining mobility after hip replacement surgery.
Working with a Physical Therapist
One of the most important steps in the recovery process is working with a physical therapist . They will guide you through a personalized rehabilitation program designed to improve your strength, flexibility, and overall mobility. The therapist will assess your condition and create a plan tailored to your specific needs.
During the initial stages, the focus will be on gentle exercises and movements to gradually increase your range of motion. These exercises may include ankle pumps, heel slides, and gentle leg lifts. As you progress, the therapist will introduce more challenging exercises to strengthen the muscles around your hip joint.
Utilizing Assistive Devices for Mobility
In the early stages of recovery, you may need to rely on assistive devices to aid your mobility. These devices can provide support and stability while reducing the strain on your hip joint. Common assistive devices include crutches, walkers, and canes.
It is important to use these devices correctly and follow the guidance of your physical therapist. They will teach you the proper techniques for walking, standing, and sitting to ensure optimal recovery. As your strength and balance improve, you will gradually reduce your reliance on these devices.
Gradually Increasing Activity Levels
As you progress in your recovery, it is essential to gradually increase your activity levels. Start with simple tasks such as walking short distances or performing light household chores. Listen to your body and avoid overexertion or pushing yourself too hard.
Your physical therapist will provide guidance on when to progress to more challenging activities. They will help you set realistic goals and monitor your progress. Remember, the key is to gradually increase your activity levels to avoid setbacks or injuries.
It is important to note that everyone’s recovery timeline is different. Some individuals may progress faster, while others may take longer. Patience is crucial during this phase, as it can take several weeks or even months to regain full mobility.
By following the guidance of your physical therapist and gradually increasing your activity levels, you will be on the right path towards regaining your mobility after hip replacement surgery.
Taking the first steps towards regaining mobility after hip replacement surgery is a crucial phase in the recovery process. Working with a physical therapist, utilizing assistive devices, and gradually increasing activity levels are key components of this phase. Remember to be patient with yourself and follow the guidance of your healthcare team. With time and dedication, you will be able to regain your mobility and enjoy a better quality of life.
Exercises for Hip Rehabilitation
After undergoing hip replacement surgery, rehabilitation exercises play a crucial role in restoring mobility and strengthening the hip joint . These exercises are designed to improve range of motion, increase muscle strength, and enhance balance and stability. By following a structured exercise program, patients can expedite their recovery process and regain their independence. In this section, we will explore the various exercises that are commonly recommended for hip rehabilitation.
Range of motion exercises
Range of motion exercises are aimed at improving the flexibility and mobility of the hip joint. These exercises help to prevent stiffness and promote smooth movement. Some common range of motion exercises include:
Ankle pumps : While lying down, flex and extend your ankles, moving them up and down. This exercise helps to improve blood circulation and prevent blood clots.
Knee lifts : While lying down, bend your knees and lift your feet off the bed. Hold for a few seconds and then lower your feet back down. This exercise helps to strengthen the hip flexor muscles.
Hip abductions : While lying down, slide your leg out to the side, away from your body. Hold for a few seconds and then bring your leg back to the starting position. This exercise helps to improve the range of motion of the hip joint.
Strengthening exercises
Strengthening exercises are essential for rebuilding the muscles around the hip joint. These exercises help to improve stability and support the new hip implant. Some effective strengthening exercises include:
Hip extensions : Stand behind a chair and hold onto it for support. Slowly lift your operated leg straight back, keeping your knee straight. Hold for a few seconds and then lower your leg back down. Repeat this exercise several times.
Hip abductions : Stand behind a chair and hold onto it for support. Lift your operated leg out to the side, away from your body. Hold for a few seconds and then lower your leg back down. Repeat this exercise several times.
Squats : Stand with your feet shoulder-width apart. Slowly lower your body into a sitting position, as if you were sitting back into a chair. Hold for a few seconds and then stand back up. Repeat this exercise several times.
Balance and stability exercises
Balance and stability exercises are crucial for preventing falls and improving overall mobility. These exercises help to enhance coordination and proprioception. Some effective balance and stability exercises include:
Single-leg stands : Stand near a wall or a sturdy chair for support. Lift one leg off the ground and balance on the other leg for as long as you can. Repeat with the other leg. As you progress, try to balance without any support.
Heel-to-toe walk : Place one foot in front of the other, touching the heel of the front foot to the toe of the back foot. Take small steps and maintain your balance as you walk forward. Repeat this exercise several times.
Tai Chi : Consider joining a Tai Chi class, as it is a gentle form of exercise that focuses on balance, flexibility, and relaxation. Tai Chi can help improve overall stability and reduce the risk of falls.
It is important to note that these exercises should be performed under the guidance of a physical therapist or a healthcare professional. They will provide you with specific instructions and ensure that you are performing the exercises correctly and safely.
By incorporating these exercises into your daily routine, you can significantly improve your hip mobility and regain your independence after hip replacement surgery. Remember to start slowly and gradually increase the intensity and duration of the exercises as advised by your healthcare provider. Stay consistent and committed to your rehabilitation program, and you will soon experience the benefits of improved hip function and overall well-being.
Overcoming Challenges
After undergoing hip replacement surgery, it is common to face various challenges during the recovery process. However, with the right mindset and strategies, these challenges can be overcome. In this section, we will discuss some of the common challenges faced by individuals after hip replacement surgery and provide tips on how to overcome them.
Managing pain and discomfort
Pain and discomfort are to be expected after hip replacement surgery. However, it is important to effectively manage them to ensure a smooth recovery. Here are some strategies to help you manage pain and discomfort:
Medication : Your surgeon will prescribe pain medication to help manage post-surgery pain. It is important to take the medication as prescribed and communicate any concerns or side effects to your healthcare provider.
Ice and heat therapy : Applying ice packs or using heat therapy can help reduce pain and inflammation. Consult with your physical therapist or surgeon to determine which therapy is suitable for you.
Physical therapy : Engaging in regular physical therapy sessions can help alleviate pain and discomfort. Your physical therapist will guide you through exercises and techniques to improve mobility and reduce pain.
Dealing with fatigue and frustration
Fatigue is a common challenge faced by individuals recovering from hip replacement surgery. It is important to listen to your body and give yourself time to rest and recover. Here are some tips to help you deal with fatigue:
Pace yourself : Avoid overexertion and take breaks when needed. Gradually increase your activity levels as advised by your healthcare provider.
Get enough sleep : Adequate rest is crucial for your body to heal. Ensure you are getting enough sleep each night and consider taking short naps during the day if needed.
Stay positive : It is normal to feel frustrated during the recovery process. However, maintaining a positive mindset can help you overcome challenges more effectively. Surround yourself with supportive loved ones and engage in activities that bring you joy.
Seeking support from loved ones and support groups
Recovering from hip replacement surgery can be a challenging journey, both physically and emotionally. It is important to seek support from your loved ones and consider joining support groups. Here’s why:
Emotional support : Your loved ones can provide emotional support and encouragement throughout your recovery. Lean on them when you need a listening ear or a helping hand.
Shared experiences : Joining support groups or online communities can connect you with individuals who have undergone similar surgeries. Sharing experiences and advice can provide valuable insights and motivation.
Professional guidance : Your healthcare team, including your surgeon and physical therapist, are there to support you. Don’t hesitate to reach out to them with any concerns or questions you may have.
Remember, overcoming challenges is a part of the recovery process. By effectively managing pain and discomfort, dealing with fatigue and frustration, and seeking support from loved ones and support groups, you can navigate through these challenges and regain your mobility after hip replacement surgery.
In the next section, we will discuss the process of returning to driving after hip replacement surgery and provide tips for a safe and comfortable driving experience.
Returning to Driving After Hip Replacement Surgery
After undergoing hip replacement surgery, one of the milestones on the road to recovery is returning to driving. However, it is important to approach this step with caution and follow the guidelines provided by your surgeon. In this section, we will discuss the guidelines for driving after hip replacement surgery, provide tips for a safe and comfortable driving experience, and offer advice on gradually building confidence behind the wheel.
Understanding the Guidelines for Driving After Hip Replacement
The timeline for when you can resume driving after hip replacement surgery varies from person to person. It is crucial to consult with your surgeon and follow their specific recommendations. In general, most surgeons advise waiting at least 4 to 6 weeks before getting behind the wheel again. This waiting period allows your body to heal and regain strength, ensuring that you can safely operate a vehicle.
During the initial weeks after surgery, it is common to experience pain, stiffness, and limited mobility. These factors can affect your ability to drive safely. It is essential to prioritize your recovery and avoid rushing back into driving before you are physically ready.
Tips for a Safe and Comfortable Driving Experience
When you are ready to resume driving, there are several tips you can follow to ensure a safe and comfortable experience:
Adjust your seat : Position your seat in a way that allows you to maintain proper posture and support for your hip. Use cushions or pillows if needed to provide additional comfort and reduce pressure on the surgical site.
Use a seatbelt cushion : To minimize discomfort and pressure on your hip, consider using a seatbelt cushion or pad. This can provide extra padding and support, making your drive more comfortable.
Take breaks : Long periods of sitting can cause stiffness and discomfort. Plan your trips with regular breaks to stretch your legs and relieve any tension in your hip. This will help prevent fatigue and improve circulation.
Avoid sudden movements : Be mindful of your movements while driving. Avoid sudden braking, accelerating, or making sharp turns, as these actions can put strain on your hip joint. Drive defensively and anticipate potential hazards to minimize the risk of sudden movements.
Use assistive devices : If you have difficulty operating the pedals or turning the steering wheel, consider using assistive devices such as pedal extenders or steering wheel knobs. These tools can provide additional support and make driving easier.
Gradually Building Confidence Behind the Wheel
Returning to driving after hip replacement surgery can be a nerve-wracking experience. It is normal to feel anxious or uncertain about your ability to drive safely. To build confidence, start with short trips to familiar places, such as the grocery store or a friend’s house. Gradually increase the duration and complexity of your drives as you become more comfortable.
If you feel overwhelmed or experience pain while driving, it is important to listen to your body and take a break. Do not push yourself beyond your limits. Remember, recovery takes time, and it is better to take things slow and steady rather than risk reinjury or discomfort.
Returning to driving after hip replacement surgery is an important milestone in your recovery journey. By following the guidelines provided by your surgeon, taking necessary precautions, and gradually building confidence behind the wheel, you can ensure a safe and comfortable driving experience. Remember to prioritize your recovery and consult with your healthcare team if you have any concerns or questions. Take control of your mobility journey and enjoy the freedom of driving once again.
Maintaining Long-Term Mobility
After undergoing hip replacement surgery, it is crucial to focus on maintaining long-term mobility. This section will discuss the importance of incorporating regular exercise into your daily routine, following a healthy diet for joint health, and scheduling regular check-ups with your surgeon and physical therapist.
Incorporating regular exercise into daily routine
Regular exercise is essential for maintaining the mobility and strength of your hip joint. It helps to improve flexibility, reduce stiffness, and increase overall joint function. Here are some exercises that can be beneficial for long-term mobility:
Low-impact aerobic exercises : Engaging in activities such as walking, swimming, or cycling can help improve cardiovascular health without putting excessive strain on your hip joint.
Strength training exercises : Incorporating strength training exercises into your routine can help build muscle strength and support your hip joint. Focus on exercises that target the muscles around your hip, such as squats, lunges, and leg lifts.
Stretching exercises : Stretching exercises can help improve flexibility and range of motion in your hip joint. Include exercises like hip flexor stretches, hamstring stretches, and hip rotations in your routine.
Remember to start slowly and gradually increase the intensity and duration of your exercises. It is important to listen to your body and avoid overexertion or pushing through pain.
Following a healthy diet for joint health
Maintaining a healthy diet is crucial for overall joint health and can contribute to long-term mobility after hip replacement surgery. Here are some dietary tips to consider:
Include anti-inflammatory foods : Incorporate foods that have anti-inflammatory properties, such as fatty fish (salmon, mackerel), nuts, seeds, and leafy green vegetables. These foods can help reduce inflammation in your joints.
Ensure adequate intake of vitamins and minerals : Consume foods rich in vitamins C, D, and E, as well as calcium and magnesium. These nutrients are essential for maintaining healthy bones and joints.
Stay hydrated : Drink plenty of water throughout the day to keep your joints lubricated and maintain optimal joint function.
Maintain a healthy weight : Excess weight can put additional stress on your hip joint. Aim to maintain a healthy weight through a balanced diet and regular exercise.
Regular check-ups with the surgeon and physical therapist
Regular check-ups with your surgeon and physical therapist are essential for monitoring your progress and addressing any concerns or issues that may arise. These professionals can provide guidance on exercises, monitor your joint health, and make any necessary adjustments to your rehabilitation plan.
During these check-ups, discuss any changes in your mobility, pain levels, or overall well-being. Your surgeon and physical therapist can provide valuable insights and recommendations to ensure that you are on the right track towards maintaining long-term mobility.
In conclusion, maintaining long-term mobility after hip replacement surgery requires a proactive approach. By incorporating regular exercise into your daily routine, following a healthy diet for joint health, and scheduling regular check-ups with your healthcare professionals, you can ensure that your hip joint remains strong and functional for years to come. Take control of your mobility journey and enjoy an active and fulfilling life post-surgery.
Unveiling The Shelf Life: How Long Does Citric Acid Last?
Unveiling The True Value: How Much Is Jcoin Worth In Today’s Market?
Rebooting Your Booze: How To Reset Alcohol Content
Quick And Easy: Mastering The Art Of Thawing Tuna
Unveiling The Dynamic Interplay: How Physical And Human Systems Shape A Place
Unlocking The Power: How Long Does It Take For Royal Honey To Activate?
Mastering Residency: A Guide On How To Study Effectively
Mastering The Art Of Die Cast Mold Making: A Step-By-Step Guide
Unveiling The Energy Consumption Of Water Coolers: How Much Electricity Do They Really Use?
Mastering Virtual Reality: Unlocking The Secrets To Altering Your Height
Leave a Comment Cancel reply
Save my name, email, and website in this browser for the next time I comment.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Blom AW, Artz N, Beswick AD, et al. Improving patients’ experience and outcome of total joint replacement: the RESTORE programme. Southampton (UK): NIHR Journals Library; 2016 Aug. (Programme Grants for Applied Research, No. 4.12.)

Improving patients’ experience and outcome of total joint replacement: the RESTORE programme.
Chapter 4 understanding patient’s experiences of total hip and knee replacement: a qualitative study.
Parts of this chapter have been reproduced with permission from Johnson EC, Horwood J, Gooberman-Hill R. Patients’ journeys through total joint replacement: patterns of medication use. Musculoskeletal Care 2014; 12 :92–102 229 © 2013 John Wiley & Sons, Ltd; and reproduced with permission from Johnson and colleagues. 230
We aimed to characterise and explore the patient pathway through total hip or knee replacement surgery in current routine NHS care.
In a qualitative study, 34 patients receiving joint replacement were interviewed before surgery, 2–4 weeks, 6 and 12 months after surgery. Interviews elicited patients’ experiences of preparing for, undergoing and recovering from surgery. Analyses used a thematic approach or interpretive phenomenological analysis.
Patients noted that delays to joint replacement in the NHS are common, which has implications for well-being. Patients’ experiences of time differ from the linear conceptualisation of time required to plan NHS services.
Undergoing surgery can increase feelings of vulnerability and alter a patient’s trust in their own body, the influence of interactions with others on confidence levels, and fears concerning the potential for causing harm to their new prosthesis. Patients rely extensively on, and value, both informal and formal support networks over the perioperative period. Transformation from a person living with osteoarthritis to a person recovering from a surgical intervention can lead to alterations in the assistance people receive from others.
When patients are not offered the support of health and social professionals, patients may feel distress and abandonment. Patient expectations for joint replacement surgery are complex and can be driven by previous personal experience, experiences of others and information provided by the hospital.
Conclusions
Our findings suggest important ways in which the provision and delivery of care and education for people undergoing joint replacement in routine NHS care can be refined and improved.
Qualitative work has provided insight into the experience and impact of living with osteoarthritis including treatment options and surgery. 5 , 24 – 27 In relation to surgery, studies have explored pathways to surgery; 4 , 29 decision-making about joint replacement; 231 and patient satisfaction and outcome. 28 , 30 However, little research has explored how patients experience their journeys through joint replacement from pre-operative care to postoperative recovery. Our qualitative research addresses this gap in evidence by focusing on experiences of pre-operative circumstances and preparation, views about the hospital stay and the operation, as well as exploring longer-term recovery, rehabilitation and outcome in the year after surgery.
The research aimed to provide robust patient-centred evidence that could inform future design and delivery of health care for people undergoing joint replacement. We used an inductive approach to the work and the areas of literature that we draw on are those that became most relevant as data collection and analysis progressed. These were related to the wait for surgery, the experience of delay, confidence and expectations as well as the experience of time in the lead up to surgery.
- Understanding the patient experience: total hip replacement
Waiting for hip replacement surgery
Within the NHS, waiting times for medical interventions are a recognised element of current health care, 232 as patients passing through the system are provided with appointment dates for consultations and treatments by a system increasingly predicated on a discourse of patient choice. 233 – 235 A continual drive to reduce waiting times for intervention, to monitor and measure the passage of time, highlights the salience and relevance of a consideration of the temporal landscape within current health-care processes. The issue of waiting times is important given that a growing body of research highlights the detrimental impact that waiting for elective surgery can have. For example, patients awaiting hip surgery have previously reported experiencing significant increases in pain and physical disability, 236 high levels of psychological distress 237 and an overall deterioration in HRQoL. 238 Our exploration of patients’ experience of time aimed to provide in-depth understanding of the impact and implications of waiting for surgery in current NHS care.
The role of confidence during the journey through hip replacement
Confidence, which is concerned with a person’s judgement about their own, or others’, abilities and vulnerability, 239 which can be defined as capable of being physically or emotionally wounded ( www.merriam-webster.com/dictionary/vulnerable ) 240 are both concepts evident in the literature concerning the experience of older age. For example falls, which are common in this population, 241 , 242 can result in reduced confidence and an enduring fear of falling. This can lead to people choosing to disengage from usual activities. 243 As osteoarthritis is associated with ageing, affecting 10% of people > 5 years of age in the UK, 1 confidence and vulnerability may have particular relevance to the experiences of patients undergoing joint replacement. A subtheme ‘building confidence’ arose in a recent study, 32 involving interviews with patients after they had undergone THR. This encompassed patients’ experiences of feeling fearful of falling and damaging their new hip and also related to confidence and use of walking aids after surgery. This builds on earlier work by Grant and colleagues 244 which reported that with increasing confidence, patients who had undergone THR 4–6 months previously talked of slowly relinquishing their reliance on mobility aids. A metasynthesis of older adults’ lived experiences of discharge from hospital after undergoing orthopaedic intervention reports that patients’ confidence can be influenced by their perception of the expertise of staff and consistency of information received around the perioperative period. 245 This small body of work provides some initial understanding regarding the influence and relationship of elements of the orthopaedic surgical experience on patients’ confidence level and vulnerability. Our exploration of patients’ experiences aimed to build on and extend these insights by providing an in-depth understanding of the ways in which their confidence was affected by, and affected, their journey through hip replacement surgery.
The experience of support during the journey through knee replacement
Living with osteoarthritis and undergoing surgery brings about pain and functional limitations. We know from existing literature that at times of disability, informal care has a large part to play 246 and recent work highlights the importance of informal support for people living with osteoarthritis. This shows that assistance from family and friends with everyday activities (such as help around the home) is valued 140 and has positive implications for mental and physical health. 247 , 248 People with osteoarthritis also engage with more formal support, including contact with health professionals and social services. 249 However, patients may have little contact with health-care professionals after discharge from surgery, at which time family are particularly important in provision of support, including personal care. 32 , 250 The value of this support is well documented 32 , 244 but can cause mixed reactions including gratitude and frustration towards family and concern about placing burden on others. 245 , 250 , 251 Importantly, previous research has not considered how patients’ relationships with others may change as they move from living with pain and limitations associated with osteoarthritis, through to postoperative recovery and to functional independence. Therefore, we conducted research to explore how undergoing and recovering from knee replacement surgery affects patients’ experiences and use of support networks.
An exploration of patients’ hopes and expectations for hip and knee replacement surgery
A large body of quantitative work has investigated patients’ expectations for recovery from elective orthopaedic surgery. 32 , 145 , 165 , 252 – 254 This evidence has highlighted the importance of considering the role and function of expectations around the perioperative period. For example, we have learned that patients’ pre-operative expectations for joint replacement are both important in their decision to have surgery 252 and can help to predict outcomes. 253 We also know that realisation of patients’ pre-operative expectations after hip and knee replacement surgery are significant in influencing their reported outcomes and satisfaction. 145 , 165 , 254 This body of work has not provided detailed understanding of expectations for recovery from joint replacement from the patient perspective. A recent qualitative study, 32 attempted to address this gap through an examination of the experiences of patients undergoing THR. The authors report that participants held high expectations of what having surgery ‘would do for them’ and suggest the value of patients having the opportunity to discuss their expectations of joint replacement in order to limit ‘false optimism’. This work illustrates the importance of using qualitative methods in order to gain novel insights into expectations of joint replacement surgery. However, McHugh and Luker 32 report only on the expectations of hip replacement patients and interviews were undertaken 6–8 months after surgery, a time-point when participants’ recovery may have still been incomplete. Therefore, we were interested in gaining an in-depth understanding of patients’ expectations for recovery from both hip and knee replacement surgery, with a focus on the fulfilment of these expectations 12 months after surgery. We hoped to gain insight both into the processes by which patients’ expectations were formed and the reasons why their expectations were, or were not, met.
- Methods for qualitative studies
Sampling and recruitment
Patients who were listed to undergo either total hip or knee replacement surgery in the Avon Orthopaedic Centre (AOC) were eligible to take part in the qualitative study. Between February 2011 and August 2012, study invitation packs were posted to 179 patients (111 hips and 68 knees). Of those who returned a reply slip to the research team expressing their agreement to be contacted about the study ( n = 52), we purposively identified a sample of men and women who were a range of ages. These comprised 29 patients undergoing hip replacement and 10 undergoing knee replacement. The programme’s qualitative researcher contacted individuals in this sample to discuss the study in more detail and for any concerns to be addressed.
Of the 29 hip patients contacted, 24 agreed to meet with the researcher to take part in an initial interview. The remaining five were no longer eligible to take part (e.g. they had been recruited into an alternative study that precluded their inclusion, their operation date had been brought forward). All knee patients who were contacted agreed to meet with the researcher. These sample sizes ensured that data from the hip sample was at saturation point, such that no new themes were emerging from analysis by the end of data collection at the first data collection point. 255 The sample size for the knee cohort was determined as appropriate for the conduct of fine-grained interpretive phenomenological analysis. 256
Data collection
In-depth semistructured interviews were conducted with all participants after they had been placed on the surgical list for joint replacement surgery. We also aimed to interview participants 2–4 weeks, 6 and 12 months post surgery. All participants provided their written, informed consent to take part immediately prior to the initial interview. As the study was longitudinal, the researcher also sought participants’ verbal agreement to ongoing participation before each follow-up interview.
Initial interviews, which lasted between 65 and 135 minutes, took place at participants’ preferred location: either in their own homes ( n = 29) or on University premises ( n = 5). Follow-up interviews, which lasted from 20 to 90 minutes, largely took place over the telephone, other than when a participant requested a face-to-face interview in their own home ( n = 6) or on University premises ( n = 1). In addition, participants whose surgery was delayed by > 3 months from their original admission date ( n = 3) were asked if they were willing to take part in an additional interview focusing specifically on their experience of delay. Two participants (one hip patient and one knee patient) agreed to this additional contact.
Interviews were carried out with 21 of the 24 hip patients and 8 of the 10 knee patients at the three follow-up points. Five participants did not take part in postoperative interviews: three because they chose not to have surgery, one because their medical circumstances precluded a follow-up interview, and one because the date of the surgery moved beyond the time constraints of this study.
The data collection time points and numbers of participants for hip and knee patients are shown in Tables 10 and 11 .
Understanding the patient experience: data collection time points for hip patients
Understanding the patient experience: data collection time points for knee patients
Interview procedure
Interview questions were framed by topic guides specific to each time point. They were informed by existing literature and developed through discussion with patient representatives. Core questions aimed to elicit participants’ experiences of preparing for, undergoing and recovering from surgery and additional probes were used to facilitate elaboration and to achieve depth. Pre-surgery interviews addressed pain and functional limitations, expectations, existing knowledge about surgery and its outcomes, and preferences for pre-operative management. Post-surgery interviews addressed pain, function, views on the care that patients have received as well as their future plans and hopes for/of rehabilitation and recovery. At the 6- and 12-month interviews, participants were asked to talk about their experiences of long-term recovery and adaptation. These interviews also revisited topics that arose from earlier interviews, including ongoing and missing support needs. Interviews exploring delay to surgery addressed participants’ views about delay and their experiences of support. Interviews were conducted by qualitative methodologists with social and behavioural science backgrounds and it was made clear to participants that the researchers were not clinical staff.
Interviews were audio-recorded, transcribed and anonymised, with the exception of two interviews which were recorded in note form owing to audio-recording equipment failure. Ethical approval was provided by NHS South West 1 REC (10/H0203/44).
- Data analysis
Initially, we analysed data from all time points of patients undergoing hip replacement separately from the data from patients undergoing knee replacement. We used different analytic approaches with each data set. Once the analysis of the two data sets was completed, we brought the hip and knee data together and conducted analysis on the pre-operative and 12-month data together.
Hips: inductive thematic analysis
We used inductive thematic analysis for the data set of interviews with patients undergoing hip replacement. This was chosen as a means of exploring change over time as well as comparing and contrasting experiences in a relatively large data set which comprised 88 interviews by the time of completion. Analysis was iterative with data collection, with use of software to enable data organisation. Anonymised transcripts of audio-recordings and notes from interviews with patients undergoing hip replacement were imported into the qualitative data management software package ATLAS.ti ® 6 (ATLAS.ti software; ATLAS.ti, Berlin, Germany). Initial analysis of transcripts began shortly after data collection started and was ongoing and iterative. Analysis informed further data collection such that early findings were used to refine the topic guides and identify questions to ask in future interviews. Transcripts from each participant were combined and treated as one single data set and were analysed using inductive thematic analysis. 257 A member of the research team first identified thematic codes which were grounded in the data. Next, through identifying connections between the codes, the research team clustered them into superordinate themes. To enhance analysis and enable team discussion and interpretation, double coding was conducted on a sample of four interview transcripts at each time point (total double coding on 16 interview transcripts). The double coding was conducted independently by members of the team who also had social and behavioural science backgrounds. The double-coding process was used as a means to stimulate close reading of the transcripts by the qualitative research team, who met regularly to discuss the codes and who worked to achieve a consensus about coding. Consensus, as agreement, was arrived at through discussion. To improve understanding of the whole data set, those aspects of data that appeared to contradict general experiences were identified and explored. The data from all patients, including those who did not have THR, were included in the analysis because their experiences of preparing for and waiting for surgery provide valuable insights.
Knees: interpretative phenomenological analysis
We used interpretative phenomenological analysis (IPA) to analyse data from knee replacement patients. This was chosen as a way to explore participants’ personal lived experiences and how they make sense of them in detail and depth with an emphasis on the detail of cases in a group of participants likely to be undergoing similar experiences. 256 , 258 IPA is an idiographic approach, focusing on the particular rather than the universal and starts with the detailed examination of case studies, which then tentatively progresses to more general statements about groups of individuals. 259 Taking this approach we were able to describe patients’ lived experiences and their process of preparing for, undergoing and recovering from surgery (i.e. how their experiences unfolded). The process of analysis was guided by a series of principles gleaned from the reflections of Smith and colleagues within research methods publications, e.g. Smith and Eatough 258 and Smith and Osborn. 260
Hips and knees: inductive thematic analysis
After identifying salient themes relating to expectations in the hip replacement data and having conducted IPA with the knee replacement patient data, we were interested in also exploring these issues for knee patients. Therefore, we imported knee transcripts into ATLAS.ti and undertook thematic analysis on this data set, employing the procedures previously described to investigate these issues further. This enabled us to explore patients’ hopes and expectations of surgery across the longitudinal qualitative data set as a whole.
As described in Methods for qualitative studies , 24 hip replacement patients and 10 knee replacement patients took part in the longitudinal qualitative study. Of the hip patients, 13 were men and 11 were women, with ages ranging from 52 to 82 years ( Table 12 ). Of the knee replacement patients, six were men and four were women, with ages ranging from 61 to 78 years ( Table 13 ).
Understanding the patient experience: participant demographics for hip patients
Understanding the patient experience: participant demographics for knee patients
Within the hip data set we explored each participant’s journey from his or her initial referral to secondary care through to his or her final surgery date. As shown in Table 14 , accounts revealed that participants took one of five main routes from referral to surgery.
Understanding the patient experience: pathways to surgery
The experience of waiting for surgery after entering secondary care and impact of delay and cancellation emerged from our analysis as salient issues for participants. We present a summary of experiences from two angles: (1) the psychosocial impact of waiting and (2) the conceptualisation and experience of ‘time’ during this period.
The psychosocial impact of waiting to undergo hip replacement
Two overarching themes relating to the psychosocial impact of waiting for THR were identified: emotional reactions and impact, and wider impact on social support networks ( Box 1 ). The impact of waiting was influenced by the time that patients had spent waiting for surgery and their journeys through health care before surgery. These aspects of waiting for hip replacement are described in turn.
Quotations to illustrate the psychosocial impact of waiting to undergo hip replacement Yes, and can you recall how you felt on that morning, when you got that phone call saying, where are you?
Psychological impact
Whether or not they experienced delay, participants all described emotional reactions to the experience of waiting.
Participants on pathways B, C and E who experienced postponement of their surgery date experienced a range of emotional reactions. Frustration and disappointment were frequently reported; however, some participants expressed understanding and acceptance of postponement. They tried to rationalise the news and described their gratitude when delay was a matter of weeks rather than months. The wait for surgery can also have more detrimental emotional consequences, for instance leading to a feeling of helplessness and utter desperation. Participants talked of feeling as if they were ‘left to linger’ in the secondary care system and forced to ‘live in limbo’.
Participants on pathway A without any delay or changes to their surgery date also described some disappointment at the length of time that they had had to wait for their operation. They recalled their dissatisfaction that their operations were not scheduled as soon as they had hoped and the disruption to their lives caused by this. The impact of delay on physical well-being and functioning also had some psychological effects. Mr Rayner’s experience provides a useful example. He experienced recurrent postponement of his operation owing to investigative but inconclusive tests for additional health problems. While waiting for THR he then experienced a rapid deterioration in his general health and functional well-being, and expressed ‘frustration’ at the situation.
Wider impact
Accounts illustrated how cancellation of operations could have wider impact, particularly affecting support networks. Participants explained how their friends and family also had to cope with and manage the participants’ own deteriorating health as well as share in their disappointment about a delay to the surgery date. Participants described how family and friends put their lives on hold and had to cope with the detrimental impact of ‘living in limbo’. Cancellation and delay also had a more practical impact as friends and family had to renegotiate their own plans to remain supportive during the perioperative period.
Consequences of preceding pathway on current experience
Participants’ views of their wait for surgery and the detrimental impact of the waiting period were influenced by their experience of time already spent living with pain and discomfort. Many participants described complex and sometimes slow journeys through health care from initial onset of their problems through to eventual referral to secondary care.
Two key factors were central in accounts of patients’ journeys through care. First, participants reported that they had initially delayed seeking advice and support from primary care practitioners. Reasons cited for this included a fear of the undesirable inevitable (i.e. surgery); other priorities (e.g. caring for a sick spouse); and choosing to ‘put up’ with pain and discomfort. Second, many participants reported the sense that referral from primary to secondary care had been delayed. Explanations provided for this delay included receiving an incorrect diagnosis; that their GP saw them as ‘too young’ to undergo THR; and that their GP strongly advocated alternative strategies (e.g. weight loss, use of pain relief). Participants’ accounts highlighted the interaction between frustration with management in primary care and subsequent impatience with the time spent waiting in secondary care.
Conceptualisation of time
Two overarching themes relating to conceptualisation of time were identified: unavoidable changes to use and passage of time in the lead-up to surgery, and time in the context of health care.
Unavoidable changes to use and passage of time in the lead-up to surgery
The progression of time from onset of osteoarthritis towards THR was marked by the experience of pain and patients made unavoidable changes to their use of time ( Box 2 ).
Unavoidable changes to use and passage of time in the lead up to surgery The left hip, um the pain has been there for years, but not severe. I’ve felt it for years. Then when the right hip was done, yeah, it was definitely there then, that was (more...)
Participants’ accounts highlighted how they had been living with pain for long periods of time and many had experienced deterioration and acceleration of their problems in the lead-up to surgery. As well as describing the long periods for which they had lived with pain, participants also described the experience of pain in terms of time. They described fleeting spasms (a ‘horrible twang’) that lasted seconds as well as constant, unrelenting pain or ‘throbbing ache’. Living a life in continuous pain with no respite appeared to provide the sense that time was drawn out during the lead-up to, and wait for, surgery.
Participants described making unavoidable and considerable changes to the way in which they spent their time because of pain and functional difficulties. When waiting for their operation, participants described withdrawal from their everyday activities and no longer actively engaging with life. For example, participants talked of inability to walk or stand for long because doing so resulted in ‘unbearable pain’. Many talked of giving up pastimes that had previously provided much pleasure, such as golf and gardening. Most of those who had been working had stopped doing so. Participants found themselves progressively unable to fill and enjoy their time as they once had done and, instead, described how they often found themselves ‘sitting down and doing nothing’ in their homes rather than actively engaging with life and ‘doing’. They talked about feelings of ‘lost time’ and a sense that time had slowed. The sense was in part due to the long process before diagnosis and then referral to secondary care. For some, such as Mr Horton, this was seen as a failure to diagnose the problem and working ‘along the wrong lines’.
In addition, the accounts of some participants indicated that day and night became conflated in the lead-up to surgery. While they would have previously been awake in the daytime, some reported resting and sleeping during the day to seek relief from the exhaustion of living in pain and due to side effects of pain medication. Participants also described pain onset or increasing intensity at night, which regularly woke them up or kept them awake. Unable to sleep well at night and sleeping during the day, participants experienced time slowing down as they waited for surgery and expressed distress, isolation and upset.
Time in the context of health care
Participants reported that their journeys through health care to arrive at surgery were lengthy, partly because they did not necessarily seek help for joint problems, but also because of slow processes of referral from primary to secondary care ( Box 3 ). Such delays earlier in their journey through health care could influence the experience and impact of the wait for surgery once within the secondary care system.
Time in the context of health care I think the doctors [GPs] could have assessed the problem quicker no doubt . . . initially the first doctor I saw didn’t think I needed a hip operation. Four months after another doctor decided (more...)
Once in the secondary care system and before admission to hospital for surgery, participants’ time was also increasingly filled with activities relating to surgery. These included trips to hospital for pre-operative education, assessments and consultations, and tasks relating to psychological and physical preparation. These activities focused participants’ attention on, and heightened their awareness of, the upcoming date in their calendar and also meant that they had to arrange their other commitments and activities.
Participants also described how time in the lead-up to surgery did not always pass at a regular, steady pace. They felt that the date of their planned admission to hospital could appear closer or further away. Some participants felt that the date was approaching too quickly and this evoked anxiety and nervousness. Others were eager and impatient to have surgery and expectations about how long their wait would be were influenced by discussions with health-care professionals in secondary care. However, some were also unsure about how long they would have to wait and thought that the timing of their operation was not static, but would be changed. Participants described uncertainty and, in relation to their experience of time, how they had to put their lives on hold when waiting for surgery.
Participants also experienced changes to their admission date and this could be due to hospital factors, ill health or the option of a date change by choosing to change surgeon. However, the impact of these factors was sometimes complicated; for instance, one participant accepted the offer to change her surgeon because it would mean that she did not have as long to wait for her operation. The new date for her operation was then postponed because her glycaemic control for type 2 diabetes was not deemed adequate for surgery. A referral ‘back’ to primary care aimed to ensure support to achieve better glycaemic control, which was then followed by a wait to re-enter the secondary care system and to learn her surgery date.
Within the longitudinal hip data set, we also explored how participants experienced confidence and vulnerability during their journeys through joint replacement surgery. Six themes were identified: participants’ changing trust in their bodies; feelings of vulnerability in relation to a surgical procedure; use and function of aids to be better safe than sorry; damage limitation and obeying the rules; awareness and fear of dislocation; and the influence of interactions with others on confidence.
Participants’ changing trust in their bodies
Participants’ accounts highlighted how their faith and trust in their body changed over the perioperative period ( Box 4 ). During pre-operative interviews, participants described lack of confidence in their hip joints, describing their hips as ‘worn’, ‘damaged’ and no longer ‘strong’. Many had experienced the sense of their leg giving way beneath them, which meant that they felt that their bodies were letting them down and, as a result, participants spoke of feeling fearful of falling, ‘unsteady’ and ‘unsafe’; all of which impacted their daily lives. Before surgery, participants also spoke of feeling ‘frightened’ when using stairs without a rail and avoided certain movements to avoid putting too much pressure on their affected joint. Some participants also spoke of a sense of vulnerability in public areas, believing that they were unable to react quickly or effectively to situations (such as a physical attack).
Participants’ changing trust in their bodies I can still walk about which I’m glad that I can walk but as for sort of relying on it to uh, for movement, no I haven’t got a lot of confidence in it.
After surgery, many participants described how they had quickly attained new or increased confidence in their body and prosthesis. They talked of feeling more physically capable and of how their leg no longer threatened to give way. Freedom from this, together with ability to engage in physical tasks that were previously difficult, enhanced trust and confidence in their bodies’ capabilities. Some participants spoke of their absolute confidence in their new hip joint and a belief that it would outlast them. However, at 12 months after their surgery, some participants said that they remained troubled by lack of confidence and faith in their body and the prosthesis. These participants described becoming more nervous of slipping over and falling since having surgery. They also spoke of a sense that the leg for which the hip joint was replaced felt weaker after surgery and uncertainty about the ability of their bodies. This had detrimental impact on their QoL.
Feelings of vulnerability in relation to a surgical procedure
Participants also articulated feelings of vulnerability in relation to the operation itself ( Box 5 ). These feelings included concern about the body’s ability to withstand surgery and apprehension about the potential for surgery to go wrong (e.g. in relation to potential detrimental side effects of anaesthetic). Participants described concern about leaving hospital to return home, seeing hospital as a safe environment. Feelings of vulnerability were heighted for those participants who were concerned about returning home if they felt that there would be no one there to look after or support them. Some participants were also concerned about the potential for the failure of the prosthesis and the presence in their bodies of the materials from which the prosthesis was made.
Feelings of vulnerability in relation to a surgical procedure I shouldn’t say this, but it worried me, I got myself in a – because they say that, you know, you’ve got to be in pretty good nick for operations, and it did worry me (more...)
Use and function of aids: better safe than sorry
Participants spoke about their use of, and the benefits of, walking aids over the perioperative period ( Box 6 ). Before surgery, many used walking aids on a regular basis. They were used to maintain and boost confidence, offer reassurance, prevent falls and offer support in situations that evoked vulnerability. Use of aids peaked in the early weeks after surgery. At the 2- to 4-week postoperative interview, many participants continued to use walking aids, saying that this reduced the risk of harm to their new joint; this was in spite of feeling that they should be able to manage now without this ‘safety net’.
Use and function of aids: better safe than sorry . . . but sometimes when I’ve been out walking; it feels as though the joint is going to give way . . . And of course you get excruciating pain when that happens (more...)
At the time of the 6-month interview, most participants were no longer using walking aids; however, this was not universal. Some spoke of occasional use, for instance, when extra security was needed but others continued to use a walking stick regularly when outside, saying that aids were ‘just like a comfort blanket’ that provided reassurance.
Damage limitation and obeying the rules
After surgery, participants avoided and restricted movements and activities that could cause potential damage to their new joint ( Box 7 ). They spoke of not wanting to ‘push their luck’ or to ‘push the joint to the limit, you know, before it’s settled’. They were nervous and described a need to remain respectful of their prosthesis and of the need to follow the postoperative restrictions and ‘rule book’. They talked of their ‘fear’ of ‘overdoing it’ and were careful and aware of their movements (e.g. standing for too long, twisting). Accounts suggested that these concerns and behaviours were driven both by a fear of harming their new joint and of not wanting to ‘undo any good that’s been done’. Some participants explained that after the initial postoperative weeks had passed they became more adventurous in the activities and movements that they engaged in. However, others remained apprehensive of particular activities (e.g. lifting, higher impact sports, dancing and gardening) and were careful when performing certain movements (e.g. bending to put tights on). This was related to a concern of not wanting to damage their new joint by placing strain on it.
Damage limitation and obeying the rules I was dead scared to disobey any of the rules, I followed them religiously.
Awareness and fear of dislocation
Before surgery, participants were mindful of the need to ‘look after’ their new joint to avoid dislocation. Concerns about dislocation peaked in the weeks after surgery ( Box 8 ). At this time participants experienced occasions when they felt that their hip was about to dislocate and spoke of their apprehension. Awareness of the potential for dislocation was informed by the verbal information and written literature provided by the hospital. This was heightened by knowledge of other people’s experiences and previous personal experience. For some participants, concerns about potential dislocation became an enduring fear, continuing to influence their behaviour and activities in the long term.
Awareness and fear of dislocation This is the only thing I’m having trouble with getting used to, is that I know, once I’ve had it done, I mustn’t do that . . . Once they’ve done it, um I don’t want (more...)
The influence of interactions with others on confidence
Although interactions with others and knowledge about dislocation could reduce confidence, participants also described how their confidence could be increased through encounters ( Box 9 ). For instance, some described how conversations with surgeons before surgery boosted their confidence in care and treatment that they would receive. Some spoke of the importance of education and information in order to feel informed about the operation and recovery. Health professionals also continued to bolster participants’ confidence in the weeks and months after surgery. In addition, observing the experiences of others who had had positive experiences of joint replacement enhanced confidence.
The influence of interactions with others on confidence So actually going into the place, um again [name of Surgeon] said, ‘I’m going to come round to see you before I – you get wheeled off’, or whatever. And so, you know, (more...)
Understanding the patient experience: total knee replacement
We were also interested in exploring how undergoing and recovering from knee replacement surgery alters patients’ experiences and use of their support networks. Using IPA 259 we examined patients’ experience of knee replacement at all time points and identified three superordinate themes relating to the experience of support: (1) relationships with health professionals over the knee replacement journey; (2) implications for informal relationships and support networks; and (3) providing support to others.
Relationships with health professionals over the knee replacement journey
‘i’ve got faith in him’: trust and confidence in the surgical team.
Participants who were undergoing knee replacement expressed considerable ‘trust’ and ‘faith’ in surgical teams. This seemed to relate to their experience of living with osteoarthritis, in which participants dealt with increasing pain and impaired mobility. By the time that they had reached secondary care, many felt that they had no choice but to rely on medical opinion and expertise, and that surgery was inevitable. This was rooted in previous positive encounters in consultations as well as experiences (their own and others) of successful outcomes after other types of surgery.
Contact with secondary care team
After having their operation, participants’ contact with secondary care health professionals shifted from the surgical team to a team of nurses, physiotherapists and auxiliaries. Relationships with health professionals also changed; participants wanted to receive support and guidance rather than the total control that they had wanted from surgical teams. After returning home, all participants had some contact, although often infrequent, with secondary care professionals – predominantly consultants and sometimes physiotherapists. They were ‘keen’ to receive follow-up appointments and ‘eager’ to obtain clinical opinion about aspects of the recovery process, for instance when they should stop using walking aids or return to leisure activities. These interactions bolstered confidence and offered reassurance.
‘You were sort of cut adrift’: unmet support needs during the recovery process
Participants also spoke of unmet support needs during the recovery process. For example, many felt that input from physiotherapists was received too late in the recovery process and that earlier involvement would have helped to reduce feelings of abandonment, enhanced motivation to exercise and facilitated earlier recovery. Postoperative aftercare in the community was also described as lacking. After discharge from hospital one participant, a widow, was not offered the support of a district nurse. Instead she described struggling with her own care, such as changing her surgical stockings, and had to implement her own support by paying for help. This participant felt that more formal support would have provided reassurance and reduced her feelings of isolation.
Differing perceptions of expertise: primary versus secondary care health professionals
Although confidence in secondary care health professionals was consistently high, participants trust in and willingness to seek support from primary health-care professionals was more mixed. Perceptions of support on offer and that received from primary care during the postoperative period was influenced by experience of care received before surgery. For example, some participants expressed dissatisfaction with primary care before surgery, describing their sense that care and advice had been inconsistent. When patients felt that primary care had not been helpful before their surgery, they were less likely to seek support actively from primary care on return home from hospital ( Box 10 ).
Quotations to illustrate relationships with health professionals over the knee replacement journey He [has] done my brother’s leg, both legs, about 6 years before me, and he’s had – you know, brilliant. I asked for him. And he’s (more...)
Implications for informal relationships and support networks
Changes in level and type of assistance.
There were changes in level and type of assistance provided and received at different points in the journey through knee replacement. Before surgery, participants described the importance of help provided by family and friends for everyday activities (such as fetching groceries and household chores). Immediately after surgery, the need for this kind of support sharply increased, with support needed for many more daily tasks, such as carrying a drink. Undergoing surgery also led to changes in participants’ roles in their relationships and family units. For example, one participant described how, when recovering from surgery, he was looked after by his children who were ‘running errands and things’ and felt that his wife treated him ‘like a baby’. These changes sometimes evoked negative emotions, including despondency and helplessness. However, as recovery from surgery progressed, the need for support and associated sense of helplessness reduced.
‘She’s always there you know when I want her’: the assumption that family will help
For participants who were married, help often came from spouses. Married participants ( n = 7) who all lived with their spouses initially turned to their spouses for assistance during the journey through knee replacement. After surgery, in addition to spouses taking on increased responsibility for tasks relating to everyday living and functioning, they also assumed additional caring responsibilities, including help with personal care (e.g. helping to bathe). Some also played a role in medical aspects of the recovery process. For example, Mr Armstrong’s wife administered postoperative anticlotting injections and Mr Clark’s wife, a retired nurse, removed his stiches. Although many participants appeared comfortable in accepting that their spouse was occupying this novel role, others felt ‘awkward’ and embarrassed at asking spouses to undertake duties that they felt should be provided by paid professionals.
Use of extended informal support networks
Participants looked outside their immediate household to other family members (e.g. children, grandchildren, siblings) and friends to meet their postoperative support needs when they could not be fulfilled by a spouse. For example, several participants were the only driver in a household and this meant that friends and family were asked to drive on their behalf while postoperative restrictions were still in place (patients are currently told not to drive for 6–8 weeks after knee replacement). Participants who did not live with spouses asked friends and family for help, particularly in the early postoperative period.
‘I’m lucky’: willingness to accept help
Participants expressed mixed emotions about the help they received from their friends and family around the time of surgery. Several viewed such support as ‘helpful’ and ‘invaluable’ and felt fortunate to be ‘spoilt’ by friends and family who ‘rallied’ around them. Although surgery was often seen as a way of maintaining independence the time around surgery was a period when help and support from others was a necessity. Many participants craved their return to self-sufficiency and most participants did eventually regain the independence that they had sought ( Box 11 ).
Quotations to illustrate implications for informal relationships and support networks Well my wife has been working like a trooper you know [since discharged from hospital]. I mean, trouble is she won’t let me do stuff. . . . going (more...)
Providing support to others
Although not a shared experience, a striking feature in the accounts of some participants was the impact that knee replacement had on the support they provided to others and how caring responsibilities influenced their journey through joint replacement ( Box 12 ). For example, Mrs Biggs, a widow and sole provider of support for her mother and brother-in-law, was particularly articulate about the reliance of others on her and the impact of surgery on this. Owing to her caring responsibilities, and despite limitations and pain imposed on her by osteoarthritis, she strived to maintain her role and not let others down. Undergoing surgery meant that Mrs Biggs temporarily passed her normal caring responsibilities onto her sister. Keenness and determination to decrease ‘burden on others’ as soon as possible and to return to her original role supporting others served to drive and motivate Mrs Biggs in her recovery from the operation. Successful knee replacement also meant that some participants felt able to assume a new role offering support to others, which they felt would have been impossible before their surgery.
Quotations to illustrate providing support to others are you where you thought you’d be six months ago in terms of recovery?
Combined hip and knee data sets
We were interested in learning more about participants’ expectations for recovery from hip and knee replacement surgery and how their expectations were met. We present here the findings of our analysis from the pre-operative and 12-month data sets.
Hopes and expectations relating to long-term pain after joint replacement
All participants hoped that hip or knee replacement would reduce their pain ( Box 13 ). For most, this was a key motivating factor for their decision to have the operation. Some participants described awareness that long-term pain was a potential issue after surgery. However, some thought this might be mild while many hoped to achieve complete freedom from pain in their operated joint in the year after surgery. Expectations relating to pain were based on previous personal experience of undergoing joint replacement surgery, knowledge of others’ experiences – both successful and unsuccessful – and information resources provided by the hospital. Most participants also described a hope that they would be able to stop use of pain relief and anti-inflammatory medication in the year after surgery. However, some also thought that they would have to continue using medication to manage pain in other parts of their body. Participants also described their hopes for the positive benefits of reduced pain in the longer term after surgery, for instance improved mood and enhanced sleep quality.
Hopes and expectations relating to long-term pain after joint replacement Having the hip replacement, the motivation is to get rid of the pain.
Expectations relating to postoperative function
Before surgery participants described living with restrictions on movement and mobility, reliance on walking aids and inability to ‘do a lot physically nowadays’ ( Box 14 ). They anticipated that joint replacement would confer better function and bring about a future in which they would be able to ‘get around easier’, walk further and with a ‘normal stride’, navigate stairs and steps with more confidence and ease, and achieve independence from walking aids. They also spoke of hoping to once again be able to kneel down, bend down and reach their toes and have the capability to return to riding a bike again.
Expectations relating to postoperative function And if we did speak in a year’s time, how do you think that life will have changed?
As a result of these changed functional abilities, participants anticipated that they would, in the year following surgery, be able to become more active and enhance their general level of health and fitness. However, several participants also acknowledged that there would continue to be some restrictions on their physical capabilities. For example, they spoke of how they would have to continue to avoid lifting heavy objects even in the long term and would also be unable to return to playing high-impact sports. They also believed that although walks to the local shops would become a future reality, hill trekking and climbing mountains would not. In addition, expectations relating to postoperative function were tempered by a sense that they may not achieve the level of function that they had before the onset of the problems with their hip or knee joint. This was informed by the sense that they continued to age and that some lived with problems in other parts of their body.
Like their expectations for pain, hopes for postoperative function were informed and shaped by their own and others’ experiences of undergoing similar medical interventions, in addition to information received around the time of surgery.
Expectations for changed engagement in social, work and life activities
Participants described expectations for participation in social and work activities after hip or knee replacement ( Box 15 ). These expectations were related to anticipation of reduced pain and increased function and were particularly driven by observations of how well others had recovered from similar operations. For example, participants hoped to return to work and looked forward to attending social clubs again, meeting friends for lunch and other valued activities including golf, bowls, bell ringing and ballroom dancing. They also hoped to be able to take holidays once more, have day trips out and travel to see friends and family, both within the UK and abroad. Participants had to stop or limit these kinds of activities before surgery because of difficulties relating to their osteoarthritis.
Expectations for changed engagement in social, work and life activities Well when it started I thought that uh, it would be an advantage for me playing golf. Because as I say my mate who I play golf with for a long time, uh, he had both his knees done (more...)
Participants’ accounts also showed how they hoped that joint replacement would provide them with the chance to engage with life once again: ‘to be able to get out again’, to ‘go out and enjoy themselves’, ‘get on with their life’ and to ‘get back their quality of life’. For some, this also meant taking up new hobbies and interests such as joining a walking club and starting voluntary work. Many participants talked of their hope to be able to participate in these activities by certain points in time, for instance Christmas or their birthday. However, a few participants did not put time markers on when, and if, their goals would be achieved, talking of ‘just having to wait and see’ and ‘just depending on how I get on’.
Fulfilment of expectations relating to pain
Twelve months after surgery, 15 participants described complete relief from pain in their operated joint ( Box 16 ). This group talked of being ‘absolutely over the moon’ with this outcome and of how they now ‘felt a hundred times better’. The operation had surpassed their expectations and they revealed how it was a ‘wonderful’ relief to be free of long-term pain. They described how it was ‘lovely’ to ‘move around without pain’; for example, how they were now able to bend down and walk without experiencing a ‘terrible pain’. As a result, as hoped, those in this group who were not living with pain in other parts of their body had halted their use of pain relief. However, 12 participants said that although they were free from the pre-operative intensity of pain arising from the grating of ‘bone on bone’, they continued to experience discomfort, soreness, tenderness, a dull ache or twinges in the area of their operated joint. They attributed this pain to a variety of causes. For example, some said that the discomfort was caused by their muscles tightening, while others thought that their recovery from surgery was not yet complete. Participants with ongoing problems were also able to identify triggers that intensified these sensations, such as exercise, ‘stretching themselves too much’, moving from sitting to standing, or standing in the same position for too long. Although living with ongoing discomfort, most members still said that they were ‘grateful’ for the treatment that they had. In keeping with attitudes to pain relief medication before surgery, participants in this group did not see pain to be ‘bad enough’ to warrant taking pain relief medication; however, two knee replacement participants described continued experience of a more ‘severe pain’ and they expressed frustration and unhappiness with this outcome. Again, as they did during the pre-operative interview, participants reflected on how previous experiences of joint replacement – their own and others’, in addition to information received around the time of surgery, played an important role in their expectations relating to pain after surgery.
Fulfilment of expectations relating to pain No pain at all . . . no painkillers . . . I was on eight paracetamol a day I think it was, on the maximum and you couldn’t sleep at night because you could be comfortable (more...)
Fulfilment of expectations relating to postoperative function
Participants spoke of how a reduction in the pain experience meant that at 12 months post operation they were able to move their body around with less difficulty and to walk further than they could before having joint replacement surgery ( Box 17 ). They were also able to ride a bicycle, more confidently navigate steps and stairs and had experienced the anticipated independence from walking aids. However, this was not a universal outcome, with walking aids still used by some participants when they walked for any distance as they continued to offer reassurance, as they had done before surgery. Participants also talked of ways in which they continued to experience a lack of freedom and restrictions on the way in which they were able to move their body. For example, some highlighted how they were unable to run or experienced difficulties when bending down to the floor to, for example, pick up objects. Accounts also showed how participants continued to experience difficulties in walking up hills, how their walking pace had slowed and that they were unable to cope with longer walks, as they had hoped. Many of those who had undergone knee replacement surgery spoke of how they were now unable to kneel down. Nonetheless, these restrictions on movement, for most, did not seem to interfere with satisfaction with recovery and were perceived as ‘no major hindrance’. A perception among participants that general ageing also played a significant role in limiting the overall potential for movement and mobility can perhaps help to explain this view.
Fulfilment of expectations relating to postoperative function Are there any things you’re doing now that you could not do before the operation?
Fulfilment of expectations relating to engagement in social, work and life activities: ‘I’ve got my life back’
Participants talked of the ways in which their lives had positively changed since undergoing joint replacement surgery ( Box 18 ). They described how they were now ‘more active’ and how life had become ‘more enjoyable’ as a result of having the operation. They spoke of having ‘a new lease of life’, of ‘making up for lost time’ and of how they were able to actively engage with more activities in each day now. As hoped, they had returned to many of the activities that they undertook prior to the onset of the difficulties with their hip or knee joint – a return to employment, social clubs, gardening, playing skittles, improved intimate relationships with partners and had already enjoyed holidays and trips to see family and friends. Planning for, and engaging in, these activities provided them with a psychological ‘lift’ and they talked of feeling ‘more positive’ and ‘optimistic’ about the future. However, for some participants, their pre-operative expectations to engage in particular social activities (e.g. taking holidays and games of golf) once they had recovered from their joint replacement surgery, were tempered, or had to be put on hold, because of other health conditions. In addition, a few participants who did not talk of additional health conditions also revealed that they continued to hold themselves back from undertaking the hobbies and activities that they had previously enjoyed and had hoped to return to (e.g. ballroom dancing). This was attributed to a lack of confidence in their new joint and concerns relating to falling.
Fulfilment of expectations relating to engagement in social, work and life activities: ‘I’ve got my life back’ I actually played nine holes um about a fortnight, three weeks ago, on a Sunday. We had a nice, sunny Sunday. Um, yeah, (more...)
Through employing a qualitative, longitudinal design, we have achieved a detailed understanding of a range of issues concerning the experience and impact of hip and knee replacement. Specifically, we have gained a comprehensive understanding of patients’ routes from referral to hip replacement surgery and have learned about the impact of waiting for surgery. This includes focus on patients’ psychosocial well-being and their conceptualisation of time. We have gained an understanding of how confidence influences, and is influenced by, experiences of undergoing and recovering from hip replacement surgery. We have also generated novel perspectives on the trajectories of support used by patients over the journey through knee replacement. We have also achieved an in-depth understanding of the nature of patients expectations for hip and knee replacement surgery, how these expectations are formed and the ways in which they are accomplished (or not) 12 months after surgery. All of these insights have been made possible by the study designs, which is one of the first to explore patients’ experiences of joint replacement in such detail from the pre- to 12-month postoperative period. Furthermore, a key strength of our work is the inductive nature of the approach, which ensured that the issues that we have addressed in this chapter are of particular salience and relevance to participants.
We have identified that delays to surgery are a common occurrence for patients in the NHS awaiting orthopaedic intervention. These changes to the date of surgery made by the system and patients’ changing perceptions while waiting for health care both have implications for patients’ well-being and this finding helps to explain views about health care. Our findings suggest that patients’ experiences of time in the lead up to surgery are complex and multidimensional and clearly differ from the linear conceptualisation of time that is required to plan NHS services. We have gained detailed and useful insights into how undergoing surgery can increase feelings of vulnerability and alter a patient’s trust in their own body, and the influence of interactions with others on confidence levels and the fears that patients have concerning the potential of causing harm to their new prosthesis. The research also highlights some of the strategies that patients engage in to limit this. We have learned that patients rely extensively on, and value, both informal and formal support networks over the perioperative period and that transformation from a person living with osteoarthritis to a person recovering from a surgical intervention can lead to alterations in the assistance participants received from others, including the source, type and level of assistance. However, when patients are not offered the support of health and social professionals over the perioperative period, for example to aid recovery, negative consequences can ensue (e.g. distress and feelings of abandonment). We have highlighted the complexity of patients’ expectations for joint replacement surgery and how these expectations can be driven by previous personal experience of undergoing joint replacement surgery, knowledge of others’ experiences – both successful and unsuccessful – and information resources provided by the hospital around the perioperative period. These insights will be useful in helping health-care professionals in educating, supporting and managing patients expectations to ensure that patients form realistic and achievable expectations for outcomes relating to pain, function and engagement with work, social and life activities.
Use of in-depth interviews facilitated a detailed exploration of participants’ experience of undergoing and recovering from joint replacement surgery. Follow-up interviews allowed for clarification of any issues raised in earlier interviews. They also facilitated the development of a closer researcher–participant rapport, which encouraged the disclosure of personal accounts, helping to generate novel insights and richer data. The use of topic guides allowed consistent exploration of salient issues across participants but also the opportunity for additional probing and reflection in order to facilitate examination of prominent and unanticipated issues. To ensure analytic rigour, analysis was conducted by a team of experienced qualitative methodologists with backgrounds in social and behavioural sciences. The analysis process included double coding, discussion and agreement to arrive at the final list of themes. Furthermore, we engaged in several other validation strategies: discussion of findings with patient representatives, reflexivity and seeking out and paying attention to negative cases. We do not claim that the experiences of the participants were representative of everyone awaiting hip and knee replacement surgery; however, the rigour of analysis helps to improve the credibility of findings. In addition, although the research was carried out with patients undergoing surgery at a single orthopaedic centre, men and women were included and the sample sizes were designed to accord with robust approaches. In the thematic approach used in the hips data set, we were confident that data saturation had been achieved. In the knees data set, use of IPA provided us with the opportunity to achieve depth in analysis and the data set size is within the norms of IPA methodology. The inclusion of patients from only one orthopaedic centre has the potential to affect transferability of findings, but the orthopaedic centre serves a diverse population in the region and it is likely that the results will resonate with the experiences of patients from other areas of the UK.
We took care in the design of the study to consider data collection approaches. Qualitative researchers have traditionally chosen to meet face to face with participants when carrying out in-depth interviews. However, research in the area now indicates that the mode of interview may have little impact on the number, character and depth of data generated during an interview. 261 However, we designed the study such that initial interviews took place in person to build rapport and consider it likely that this enabled the generation of even richer data during subsequent interviews that were conducted by telephone. The study had excellent retention; interviews were carried out with 21 out of the 24 hip patients and 8 out of the 10 knee patients at the three follow-up points.
Our findings suggest important ways in which the provision and delivery of care and education to people undergoing joint replacement in routine NHS care could be refined and improved. For example, patients can experience a range of emotional reactions if they experience delay and cancellation of their surgery date. Even without a delay, the wait for surgery alone can have detrimental physical and emotional consequences and cause wider psychosocial disruption. It is important that health professionals recognise these consequences, affirm patients’ experiences, identify those at increased risk and work towards minimising delay and cancellation of operation dates when possible. In addition, findings demonstrate the value of recognising the fluid and dynamic nature of time and broader temporal issues embedded in the perceptions, interpretations and experiences of patients in the lead up to joint replacement. Findings also highlight how patients appear to value the offer of postoperative physiotherapy shortly after surgery as well as longer-term follow-up in secondary care. The latter may be of particular value for those patients who experience complications after surgery or who are particularly troubled by a lack of confidence and faith in their prosthesis.
The findings of our analysis suggest the importance of future directions for work that concerns patients’ experiences of undergoing joint replacement surgery. For example, for some participants, concerns about potential dislocation became an enduring fear, something that influenced their behaviour and activities 1 year after surgery. This suggests the need to investigate the influence and impact of these concerns in the longer term and learn more about how best to support this group of patients. In addition, findings suggest the value of future work to address the specific impact of age, sex and cohabitation status on patients’ use of support networks around the perioperative period.
Included under terms of UK Non-commercial Government License .
- Cite this Page Blom AW, Artz N, Beswick AD, et al. Improving patients’ experience and outcome of total joint replacement: the RESTORE programme. Southampton (UK): NIHR Journals Library; 2016 Aug. (Programme Grants for Applied Research, No. 4.12.) Chapter 4, Understanding patient’s experiences of total hip and knee replacement: a qualitative study.
- PDF version of this title (87M)
In this Page
Other titles in this collection.
- Programme Grants for Applied Research
Recent Activity
- Understanding patient’s experiences of total hip and knee replacement: a qualita... Understanding patient’s experiences of total hip and knee replacement: a qualitative study - Improving patients’ experience and outcome of total joint replacement: the RESTORE programme
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Questions? Call us at 647-797-7616 | Hassle Free Returns | Learn More
Item added to your cart
Getting dressed after your hip replacement: a comprehensive guide.
Undergoing a hip replacement is a significant life event, one that can dramatically enhance your quality of life and mobility. However, the journey to full recovery is not without its challenges, and one seemingly simple task that can become surprisingly difficult is getting dressed. In this comprehensive guide, we'll explore the various aspects of dressing after your hip replacement, including clothing choices, adaptive options, and practical tips to make the process as smooth as possible.
The Importance of Safe Dressing Post Hip Replacement
Hip replacement surgery is often recommended to alleviate pain and restore mobility in individuals suffering from hip joint problems. While the surgery is highly effective, the recovery period demands careful attention to avoid complications and discomfort. Safe and efficient dressing plays a pivotal role in this phase of your recuperation. Here's why it matters:
Minimizing Strain: During the initial recovery period, it's essential to reduce strain on the newly replaced hip joint. Any sudden or excessive movements can lead to discomfort or complications.
Regaining Independence: The ability to dress independently is a significant milestone in your recovery journey. It can boost your confidence and overall well-being.
Adaptive Solutions: With advancements in medical technology and clothing design, there are adaptive solutions available that can significantly simplify the dressing process and enhance your overall comfort.
In this blog post, we'll break down the dressing process into simple steps, discuss the significance of clothing choices, and explore adaptive clothing options to assist you in making this daily task a breeze.
Dressing After Hip Replacement: The Basics
Before we dive into the step-by-step dressing guide, let's start with some basic considerations for dressing after your hip replacement:
1. Choose the Right Clothing:
Your choice of clothing is pivotal in ensuring a smooth dressing process. Opt for garments that are easy to put on and take off. Consider loose-fitting clothing that doesn't require excessive bending or stretching.
2. Front-Closure Clothing:

3. Adaptive Clothing:

4. High-Waisted Options:
Opt for high-waisted clothing that provides coverage for your surgical site, offering extra support and reducing irritation or pressure on the incision area.
5. Stretchy Fabrics:
Choose clothing made from soft, stretchy materials that are easy to manipulate without causing discomfort. Stretchy fabrics accommodate any swelling or changes in your body shape during recovery.
Now that we've covered the basics, let's move on to the step-by-step guide for dressing after your hip replacement.
Step-by-Step Guide to Dressing After Hip Replacement
Here is a comprehensive, step-by-step guide to help you get dressed after your hip replacement surgery:
1. Prepare Your Dressing Area:
Start by arranging your clothing, adaptive tools (if needed), and a stable, comfortable place to sit. Ensure that you have everything within arm's reach to minimize unnecessary movements.
2. Sit Down:
Begin by sitting on a sturdy chair or your bed. Use a cushion or pillow if necessary to elevate your surgical leg slightly. This position helps maintain the correct hip angle for comfort.
3. Put on Underwear and Pants:
Start by sliding your operated leg into your underwear and pants. Go for front-closure options or adaptive clothing that simplifies this process. Take your time to avoid sudden movements and strain.
4. Use Adaptive Tools:
If you have adaptive clothing with magnetic or easy-release fasteners, now is the time to take advantage of these features. They can significantly simplify the dressing process.
5. Dress Your Non-Operated Leg:
Once your operated leg is comfortably dressed, proceed to dress your non-operated leg. Again, front-closure or adaptive clothing can be a significant help in this step.
6. Put on Your Top:
When it comes to putting on tops, consider adaptive options with front closures. These can be a real time-saver and can help you dress independently.
7. Make Necessary Adjustments:
Take a moment to ensure your clothing fits comfortably and does not bunch up or constrict. Make any adjustments to achieve a snug but comfortable fit.
By following this step-by-step guide and selecting appropriate clothing, you can make the process of getting dressed after hip replacement surgery much smoother and more comfortable. Regaining your independence and confidence is essential for a successful recovery.
The Benefits of Adaptive Clothing
Adaptive clothing has emerged as a significant asset for individuals recovering from hip replacement surgery or those with limited mobility. Here are some key benefits of adaptive clothing:
1. Independence:
Adaptive clothing empowers individuals to dress independently, boosting their sense of self-sufficiency and confidence.
2. Comfort:
These garments are designed with comfort in mind, reducing irritation and pressure on surgical sites or sensitive areas.
3. Convenience:
The innovative closures and designs in adaptive clothing save time and energy during the dressing process.
4. Stylish Options:
Adaptive clothing has come a long way in terms of style and fashion. You can find adaptive options that suit your personal taste and preferences.
Finding Adaptive Clothing
Adaptive clothing is becoming more widely available, both in physical stores and online. To find adaptive clothing that suits your needs, consider the following:
1. Medical Supply Stores:
Many medical supply stores offer a range of adaptive clothing options for individuals with mobility challenges. These stores often have staff who can assist you in finding the right garments.
2. Online Retailers:
Numerous online retailers specialize in adaptive clothing including JuneAdaptive.com . You can browse through a wide selection of styles and sizes and read reviews from other customers to help you make informed choices.
3. Specialty Brands:
Several clothing brands are dedicated to designing adaptive clothing. These brands focus on combining fashion with functionality, creating a broad range of stylish options.
4. Consult Your Healthcare Provider:
Don't hesitate to consult your orthopedic surgeon or physical therapist for recommendations on where to find suitable adaptive clothing. They may have valuable insights or local resources to share.
Final Thoughts
Dressing with ease after hip replacement is not only possible but also essential for a smooth recovery. Selecting the right clothing, including adaptive options, can significantly improve your comfort and independence. Remember to consult with your healthcare provider for personalized guidance and recommendations, and don't hesitate to explore the world of adaptive clothing to find solutions that suit your unique needs. Your journey to improved mobility and well-being begins with the little things, like getting dressed effortlessly and confidently.
Leave a comment
Please note, comments need to be approved before they are published.
Let customers speak for us
My mother has severe edema and cannot wear shoes. I have modified various kinds of slippers for her but they didn't really work either. I found your 'Unisex Wide Easy-On Fleece Bootie Slippers' on the internet and took a chance by ordering them. They are perfect!!! Mom loves them; They are really warm and comfortable, and she finally has something to wear on her feet.

Bought these for my mother who suffers from arch and heel issues. She has loved these and feels truly supported in them.

Practical and very warm. I ordered 1 size up and it fit perfectly

Great product. Easy to put on and take off. Very comfortable. Will use these even after my husband’s recovery. Great for someone in a wheelchair and has a colostomy and catheter.

Very comfortable. easy to put on and take off. Especially good for wheel chair use. Nice color.

Love the dual zipper, great traction.
I had these items shipped straight to my Aunt she is in 24hour care and I am told that this is an excellent item for her and that she really likes it

This sweater was purchased in cream colour for my mom who uses a wheelchair. It is a great heavier weight sweater for cooler days. After laundering, it is lovely and soft.
My mother absolutely LOVED this shacket and has gotten countless compliments.

The wide fit is great for my mothers swollen feet
These are the most comfortable pjs for my dad I’ve bought. Any other are too bulky and not as soft. He really likes them and keeps them on most days. I only bought one pair to check them out and need to buy more.

Very happy with the product especially since our electric was off for almost 24 hours so no heat in the house and very low outside temperatures, Needless to say, it was my son's favorite Christmas gift and he wore it all day on Christmas until our electric came back on and our heat warmed the houRead more about review stating Men's magnetic closure sherpa shacket with detachable hoodse again. Thank you!

nice fabric ,good fit ,my mom loves them

This style with the open toe has been helpful in preventing the regrowth of toe calluses.

I bought the clothes for my Sister-in-law and she just loved them. Also the staff at her care center were very appreciate as it makes dressing her so much easier. Looking forward to my next purchase.
Our Customers Favourites
- Men's Pants with Side Zipper 11 reviews Men's Pants with Side Zipper Regular price $49.98 CAD Regular price Sale price $49.98 CAD Unit price / per
- Ankle Anti-Slip Socks (3 pairs) 15 reviews Ankle Anti-Slip Socks (3 pairs) Regular price $30.98 CAD Regular price Sale price $30.98 CAD Unit price / per
- Mens Short Sleeve Shirt with Magnetic Buttons 21 reviews Mens Short Sleeve Shirt with Magnetic Buttons Regular price $74.98 CAD Regular price Sale price $74.98 CAD Unit price / per
- Men's Cotton Pants with Elastic Waist 2 reviews Men's Cotton Pants with Elastic Waist Regular price $54.98 CAD Regular price Sale price $54.98 CAD Unit price / per
- Choosing a selection results in a full page refresh.
Can You Jog After Hip Replacement? A Comprehensive Guide
Can you jog after hip replacement surgery? It’s a question that many patients with an active lifestyle often ask. In this comprehensive guide, we will delve into the recovery process following traditional total hip replacements and explore how one can gradually return to activities like jogging.
We’ll take you through the journey of recovery post-surgery, discussing timelines and techniques for regaining muscle strength in your hips. You’ll hear inspiring stories of runners who’ve successfully returned to pain-free running even after having their left hip replaced.
The role of physical therapy in rehabilitation cannot be overstated; hence, we will also highlight its importance during the post-operative period. Furthermore, we discuss life beyond major surgeries like total hip replacements and how pacing oneself while planning future sporting events is crucial.
Lastly, we consider other options besides complete joint replacements such as hip resurfacing. Are they viable alternatives? What are the risks associated with high impact activities on late-stage osteoarthritis patients? Can you indeed jog after a hip replacement? Read on to find out more.
The Journey of Recovery After Hip Replacement
Recovering from hip replacement surgery is a unique journey for each person. Regaining strength and suppleness in the hip muscles is an integral part of recuperation after a hip replacement, so that one can get back to their usual activities – such as running.
Understanding the Timeline for Post-Surgery Recovery

The typical recovery period after hip replacement surgery ranges between 3-6 months. Recovery duration may differ depending on elements such as age, state of health, and observance to physical therapy sessions. The first few weeks are generally focused on managing pain and swelling while gradually increasing mobility with walking aids like crutches or walkers.
Around six weeks post-surgery, most people can walk without support and start driving again. By three months, they’re usually able to perform light activities such as swimming or cycling. High impact exercises like running should only be reintroduced around six months after surgery when the hip joint has fully healed.
Techniques for Regaining Muscle Strength in Hips
To regain muscle strength in your hips after surgery, it’s crucial to adhere strictly to the rehabilitation plan set by your physiotherapist. This typically includes strengthening exercises targeting key muscle groups supporting the hip joint: gluteus maximus (your buttock), quadriceps (front thigh), and hamstrings (back thigh).
- Gentle stretching: Start with gentle stretches under supervision before progressing towards more challenging ones once comfortable.
- Bridges: Lying flat on your back and lifting your pelvis off the ground helps strengthen both glutes and hamstrings simultaneously.
- Squats: Assisted squats initially using chair/wall support can help build up quad strength over time leading eventually into unassisted full squats.
Remember, everyone heals at their own pace, so it’s important not to rush through these stages, risking potential injury. Always consult with healthcare professionals regarding appropriate timelines based upon personal progress during regular check-ups, ensuring a safe and effective rehabilitation process post-surgery.
Patience is key here. You’ll need plenty of it along this journey, but rest assured all hard work will pay off, allowing resumption of favorite high impact sports, including jogging, sooner than later.
Recovering from hip replacement surgery takes time and patience, with a typical recovery period of 3-6 months. To regain muscle strength in the hips, it’s important to follow a rehabilitation plan set by your physiotherapist that includes exercises like gentle stretching, bridges, and squats. High impact exercises like jogging should only be reintroduced around six months after surgery when the hip joint has fully healed.
Inspiring Stories of Runners Post-Hip Replacement Surgery
Hip replacement surgery is a major procedure that requires significant recovery time and can limit mobility. But with determination, physical therapy, and the right mindset, it’s possible to regain pre-surgery stamina levels – even for avid runners.
Determination Can Help Regain Pre-Surgery Stamina Levels
Take Tom as an example. He was always on his feet – running marathons or just jogging around the neighborhood park. But when arthritis developed due to injuries, he had to undergo total hip replacement surgery.
Tom persevered to overcome his injury and resumed running, ultimately achieving a triumphant marathon finish post-total hip replacement surgery. With consistent effort in physical therapy sessions, he managed to get back on track and regain his pre-surgery stamina levels.
Successful Marathon Participation Post-Total Hip Replacement Surgery
There are countless inspiring stories out there like Missy Gosney and Sam Szura who underwent similar surgeries yet didn’t let their passion fade away.
- Missy Gosney: A dedicated runner who faced severe hip problems due to hereditary factors leading eventually towards a complete joint replacement surgery at 49 years old. Despite this setback, she made an amazing comeback by participating in half-marathons post-recovery. source
- Sam Szura: She suffered from debilitating osteoarthritis which resulted in two total hip replacements within six months apart at age 52. Her strong willpower led her towards completing multiple full marathons after these procedures without any discomfort or complications. source
Their incredible journeys show us how life doesn’t stop after such major surgeries if you have the right attitude and dedication towards your goals along with appropriate care routines & balanced exercises regimes under professional guidance.
All these examples prove that undergoing a major surgical procedure like total hip replacement does not mean giving up high impact activities such as jogging/running forever. Instead, it opens doors towards exploring new ways of maintaining active lifestyles while taking necessary precautions & modifications according to individual needs post-surgical rehabilitation period under medical supervision.
The article discusses inspiring stories of runners who have undergone hip replacement surgery and managed to regain their pre-surgery stamina levels through determination, physical therapy, and the right mindset. Examples include Tom, Missy Gosney, and Sam Szura who all showed that undergoing a major surgical procedure like total hip replacement does not mean giving up high impact activities such as jogging/running forever but rather opens doors towards exploring new ways of maintaining active lifestyles while taking necessary precautions & modifications according to individual needs post-surgical rehabilitation period under medical supervision.
The Role of Physical Therapy in Post-Surgical Rehabilitation
After undergoing a major surgery like total hip replacement, physical therapy is essential for regaining strength and mobility in order to return to your active lifestyle. Physical therapy is a must for regaining the strength and flexibility in your new joint after surgery, so you can return to your regular activities.
Why Regular Physical Therapy Sessions are Important
Physical therapy sessions are crucial during rehabilitation for several reasons. First, they help reduce pain and swelling post-surgery. Therapists may assist in increasing blood flow, which can hasten healing and reduce the possibility of issues like clots.
But that’s not all. Physical therapists guide patients through exercises designed to restore range of motion and strengthen muscles around the new joint. This is essential because strong muscles provide better support for your artificial hip, reducing strain on it when you engage in high impact activities like jogging or running.
Case Study – TCS New York City Marathon Participant
Let’s take a look at John Doe (name changed), who participated in the TCS New York City Marathon six months after his total hip replacement surgery. Doe was determined not to let this setback deter him from achieving his goal.
Doe started attending regular physical therapy sessions soon after his operation where he worked tirelessly under professional guidance to regain muscle strength around his hips while maintaining flexibility. His therapist gradually introduced low-impact cardiovascular exercises into his regimen before slowly transitioning him back into jogging over time.
This methodical approach paid off tremendously as Doe successfully completed the marathon without any discomfort or setbacks. The key takeaway here is that with determination combined with appropriate care routines including regular physiotherapy sessions, even significant procedures like total hip replacements need not put an end to one’s passion for running.
Physical therapy is essential for post-surgical rehabilitation after a total hip replacement. It helps reduce pain and swelling, improves blood circulation, restores range of motion and strengthens muscles around the new joint. With determination and appropriate care routines including regular physiotherapy sessions, even significant procedures like total hip replacements need not put an end to one’s passion for running.
Life Beyond Major Surgeries Like Total Hip Replacement
As a runner who’s undergone total hip replacement surgery, you might wonder if you can still participate in marathons. The answer is yes. With proper care and exercise, many have resumed their love for running post-surgery.
Pacing Yourself for Sporting Events
Returning to sports after major surgeries like total hip replacements requires pacing yourself. Gradually reintroduce jogging or running while listening to your body’s signals. Start with low-impact exercises like swimming or cycling before transitioning to more strenuous activities. Set realistic goals and remember that patience is crucial.
Exercise Regimes & Care Routines
A balanced exercise regime is crucial for maintaining an active lifestyle post-surgery. Incorporate strength training and flexibility exercises to improve muscle tone and stability. The American Academy of Orthopaedic Surgeons (AAOS) recommends specific exercises for joint replacement recovery.
- Strength Training: Leg presses, squats, and lunges strengthen muscles supporting the hips.
- Mobility Exercises: Walking or stationary biking improves range-of-motion.
- Flexibility Workouts: Stretching routines aid movement and prevent stiffness.
Adopt appropriate care routines, including following dietary recommendations for bone health and regular check-ups to monitor progress since surgery.
The journey beyond major surgeries isn’t easy, but it’s possible. Countless stories showcase how people have bounced back stronger despite undergoing significant procedures like total hip replacements.
Exploring Other Options Besides Complete Joint Replacements
If you’re under 60 and suffering from late-stage osteoarthritis, the thought of a complete joint replacement might be daunting. But did you know there are other options available today that can help manage your condition without risking further degeneration or development of new joint-related issues caused by high impact activities like jogging/running? One such option is Hip Resurfacing .
Hip resurfacing – A viable alternative?
In contrast to total hip replacement surgery, where the entire hip joint is replaced with an artificial one, Hip Resurfacing involves replacing only the damaged surfaces of the joints. This procedure has been gaining popularity as it allows patients to retain more natural bone tissue and provides greater stability post-surgery.
The advantage here is twofold: Firstly, retaining more natural bone means less invasive surgery and potentially quicker recovery times. Secondly, this technique provides better long-term potentials for those who desire to remain involved in intense sporting activities such as running or jogging after their surgery.
The risks associated with high impact activities on late-stage osteoarthritis patients
While staying active is important for overall health and well-being, certain types of physical activity can pose challenges for individuals dealing with advanced stages of arthritis. High-impact activities can be detrimental to late-stage osteoarthritis patients, so it is essential to find a balance between strength training and cardiovascular workouts that will not overstress the joints.
- Maintain balance: It’s crucial that any exercise regime balances strength training (to support your joints) with cardiovascular workouts (for heart health).
- Pace yourself: Start slow and gradually increase intensity levels based on how comfortable you feel during workouts.
- Avoid overdoing it: Listen to your body. If something doesn’t feel right during or after exercising – stop immediately.
This isn’t meant to scare anyone away from being active but rather serve as a reminder about the importance of managing physical activity responsibly when living with conditions like osteoarthritis.
To summarize: Yes. You absolutely can jog again even after undergoing major procedures like total hip replacements; however always remember that everyone’s journey towards recovery will look different depending upon various factors including age, general health status etc., so please consult your healthcare provider before starting any new fitness program post-surgery.
Hip resurfacing is a viable alternative to complete joint replacements for those under 60 suffering from late-stage osteoarthritis who wish to continue engaging in high-impact sports like running or jogging after their operation. However, it’s important to manage physical activity responsibly when living with conditions like osteoarthritis by maintaining balance, pacing oneself and avoiding overdoing it. Always consult your healthcare provider before starting any new fitness program post-surgery.
FAQs in Relation to Can You Jog After Hip Replacement
Starting jogging after hip replacement: tips and tricks.
Begin with low-impact exercises like walking, gradually increasing distance and speed, and transition to a light jog under your doctor’s guidance.
Activities to Avoid After Hip Replacement Surgery
Avoid high-impact sports like football and basketball that involve jumping and sudden movements, and consult your physician for personalized advice.
Playing Sports After Hip Replacement: What You Need to Know
Participate in lower-impact sports such as golf, swimming, or cycling post-recovery, but approach running with caution.
Using a Treadmill After Hip Replacement: Safety Tips
Treadmill use is generally safe post-recovery, but always begin slowly under professional supervision and consider using incline settings for added challenge without increased risk. Check out this article for more information on treadmill exercises after hip replacement.
Yes, you can jog after hip replacement surgery! Proper care and rehabilitation, including physical therapy, can help you regain your pre-surgery fitness levels.
Don’t believe us? Check out inspiring stories of runners who have completed marathons after total hip replacement surgery.
But if you’re not a suitable candidate for complete joint replacements, consider exploring alternative options like hip resurfacing.
Similar Posts

Is Sprinting Better Than Jogging? A Fitness Comparison
Explore our in-depth analysis on “is sprinting better than jogging”, comparing benefits, muscle-building capabilities, and the impact on cardiovascular health.

Is Jogging in Place Effective? Unraveling the Truth
Is jogging in place effective?” Discover the benefits and techniques of this workout in our latest blog post.
How Long Does It Take to Jog a Mile: A Comprehensive Guide
Discover how long does it take to jog a mile, the factors affecting your average mile time and tips for improving running performance on DaDi’s blog.

How to Make a Bike Seat More Comfortable: Tips and Tricks
Proper Body Alignment and Bike Seat Setup Ensuring proper body alignment on your bike is crucial for a comfortable…

Who Won The Boston Marathon in 2023? Results, Highlights & More
Find out who won Boston Marathon 2023, with highlights, records, and historic moments in this thrilling race recap.

How Long Does It Take to Jog 5 Miles: A Comprehensive Guide
Discover how long does it take to jog 5 miles, factors affecting your running speed, and tips for beginners and experienced runners on DaDi’s blog.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

What I Wish I Knew Before Hip Replacement Surgery
MIDLIFE HEALTH
A total hip replacement at age 49 was scary, and it changed my life. Here’s what I learned.
Disclaimer : I am NOT a doctor and have no medical training. Nothing you read here should be construed as medical advice. If you are seeking medical advice, diagnoses, or treatment, consult a medical professional or healthcare provider. I am sharing my story for educational purposes only.
When my mobility evaporated at age 49, I was shocked to learn I needed hip surgery, and this is what I wish I knew before my hip replacement.
Being told you need a hip replacement can feel scary and overwhelming. Knowing what to expect and what I had control over, would have eased my anxiety about surgery and aided in recovery afterward.
Please comment below if you are also facing hip surgery and have questions about my experience.
Before I share what I learned, here is a quick recap on my hip replacement. Hip pain and limited mobility led me to learn I had hip dysplasia, which was never previously diagnosed. X-rays revealed the cartilage in my left hip had degenerated to the point that my only option was a total hip replacement. You can read the story of my hip replacement, including a week-by-week recovery in Hip Replacement Recovery.
After searching for the right doctor (more on that below), I opted for an anterior hip replacement , rather than a traditional posterior replacement. My surgeon was Dr. Craig Loucks of Peak Orthopedics in Denver. That was almost seven years ago, and I am happy to say that surgery completely changed my life for the better.

What I Learned and Wish I knew, Before Hip Replacement Surgery
I wasn't too young for a hip replacement.
When I first started experiencing pain and limited mobility, I was certain the problem was my back. I had struggled with back pain and stiffness since I was pregnant with my second son. Despite declining mobility, I had never heard of anyone younger than 50 needing hip replacement surgery and I was in my late 40s. So I pursued therapy for my back and as a result, I suffered needlessly for months before finally learning the problem was indeed my hip.
I wish I had known that hip replacements are increasingly common among younger patients, and I wasn’t too young for the procedure. According to the Cleveland Clinic, hip replacements among patients aged 45-54, increased 200% between 2000 and 2010. Part of the reason is that newer materials used in hip replacements now last longer, so younger patients are having the surgery sooner.

It was ok to be choosy about the surgeon for my hip replacement
Once my hip degeneration was diagnosed, I made an appointment with a local orthopedic surgeon recommended by several friends. He was a leading expert. This would be simple, Ithought — we’d meet and I would schedule my surgery. I was a busy mom with kids who were 16 and 13. Hip pain was interfering with my sleep, and my lack of mobility was problematic for all of us. The sooner I had surgery, the better.
I was incredibly nervous on the day of the meeting; I was taking the first concrete step toward surgery. Rather than leaving that appointment feeling at ease, I left feeling more anxious than before. The appointment had been somewhat rushed, and although the doctor was pleasant enough, something felt off. It didn’t occur to me that I had every right to consider other surgeons. People said this surgeon was great; was I being irrational?
I decided to do additional research about the options available, and that was when I learned about an anterior hip replacement. With its muscle-sparing technique and faster short-term recovery, it seemed like something I should consider. I was surprised the first surgeon hadn’t mentioned it. I checked back on their website and learned that they didn’t do that style of surgery. I wanted to talk to a doctor who did.
Meeting with Dr. Craig Loucks was an entirely different experience. He took time to explain everything and answer all my questions. I felt my anxiety lift as he reassured me that I was a perfect candidate and my life would totally change post-surgery. He advised I have my hip replacement ASAP. By the end of the appointment, I had scheduled surgery and felt hopeful for the first time in months.
I wish I had known that I should do my own research and it was reasonable to meet with multiple doctors. I didn’t have to go with the first doctor I met with. It would have saved me some anxiety.

Preparing for surgery would feel like a part-time job
My surgeon had an unexpected opening, and his office asked if I wanted surgery in three weeks. Otherwise, I’d have to wait a while. I jumped at the chance. I wish I’d known what those next three weeks would look like.
A hip replacement is still a major surgery. As such, there are many tests and appointments required before surgery. I needed an electrocardiogram to ensure my heart was strong enough for surgery. I also had to see my regular doctor for bloodwork and a complete physical to ensure I was healthy and could have surgery.
Complications began almost immediately. I couldn’t schedule surgery until my insurance company authorized it so that delayed things. I was told insurance companies can take up to two weeks to process the request.
My doctor’s office never sent bloodwork to the surgeon, which required extra phone calls. And there were endless email exchanges with Dr. Loucks’ surgery scheduler as I provided all the required information and test results to their office — the paperwork seemed endless.
I had to meet with a physical therapist before surgery, so I would have everything in place to begin PT when the surgeon gave me the ok. PT is a crucial part of recovery.
I was also preparing for my mom to visit; she’d stay for a week or two after surgery to help with the kids.
I wish I had known before hip surgery that three weeks would be tight timing for all the pre-op requirements because it made the preparation especially busy and stressful.

My recovery would be 2-steps forward and 1-step back
I was home the same day I had surgery which was wonderful. I was grateful it was over. But there was lots to do and manage; I found the compression girdle and tights I had to wear a bit inconvenient. There were medications to track as well. And that first week felt as though a horse had kicked my upper thigh, where my incision was. I ached and so I did very little.
By week two, I felt better and was very tired of being in bed. My husband took my mom and I for a drive into the mountains and I managed a short walk on a nature trail; I breathed in the crisp fall air. It felt wonderful. I felt ready to begin more exercise but was not permitted to walk other than a very short jaunt. My surgeon had given me a stern warning against doing too much too soon, even though I felt ready. I wasn’t prepared for how frustrating that would feel.
Then I hit a plateau in week three, more achy pain. The journey to full recovery would take time, and I had to be patient. Recovery might not be entirely linear. I wish I had known that those first weeks would come with ups and downs as I dealt with progress and what felt like setbacks.

At times, I would question my hip replacement recovery
As mentioned above, there was some pain with recovery. It was manageable but still discouraging at times. Interestingly, it was a different pain than I had had in my hip joint. My hip pain was entirely gone which was a huge relief.
Pain is interesting because although you are told to expect it, dealing with pain in recovery is more difficult for some people than others. For me the issue was around week four when I wondered if my residual pain would ever resolve? Was this “normal” versus something that meant I wasn’t progressing in my healing. I called the surgeon and my mind was put at ease. I’d see them two weeks later as planned.
I wish I had talked more with my surgeon about what type of pain to expect and what was normal recovery versus what were red flags suggesting I should give them a call. And I wished I had called them sooner to put my mind at ease.

Post-surgery physical therapy would require patience
I knew I’d be doing physical therapy and was ready to commit to a challenging routine. But my therapist had me doing very basic exercises to start, three weeks post-surgery. I had lost some balance, for example, and needed to regain it. I was frustrated. I wanted my fitness level back and felt ready to get more active. But I needed to follow his lead on what I should be doing and when. That required patience.
As with the rest of my hip replacement recovery, knowing something and experiencing it are different. I hadn’t expected my balance to be off and needed to work on basics. Getting back to my previous fitness level would take more time and patience than I anticipated.

I could enjoy exercise other than running
My surgeon advised me that once I recovered from surgery, I could do everything I did before, other than running and high-impact exercises. Although I was a casual runner, I liked that it was an efficient way to get a cardio workout and alleviate stress; I ran a few days a week.
So when Dr. Loucks told me running was prohibited after surgery, I was initially disappointed. It felt like another loss I had to accept.
I wish I’d known that once I got used to other forms of exercise, I wouldn’t miss running at all. I grew to love indoor cycling, and a personal trainer helped me establish a new routine to support my physical therapy and regain the strength I’d lost when I’d been inactive. With a new routine, I gained muscle and surpassed my previous level of fitness.

Life after my hip replacement would be better than I imagined
At my appointment at seven weeks after hip surgery, I was given the go-ahead for more exercise. From there, things rapidly improved. It would take about six months before I got to a point where I wasn’t being cautious of my hip at all and truly felt myself.
Just over a year later, I went on a bucket list trip to India. I also changed my perspective on prioritizing myself and my health, which enabled me to get into the best shape of my life. I wrote about how my hip replacement inspired me to prioritize my health in: Fit At Fifty .
Learning that you require a total hip replacement is scary and stressful. More than anything else, I wish I had saved myself a lot of anxiety by believing that everything would go smoothly and my life after surgery would be even sweeter than before. Once you have a hip replacement, you appreciate your health and mobility in a new way. hip
74 Responses
I so agree..I have experienced the same thoughts even..the plateaus and all. It has only been 2 months..in good shape but older than you..have ups and downs..to be expected! Thanks for sharing..feeling encouraged and most of all ..we still can walk and enjoy life. The best to you.
Hi Sue. So glad to hear you are on the road to recovery. Absolutely — being able to walk and enjoy life is what it’s all about.
I’m preparing for THR ROBOITICLY…your story helps me with the anxiety I’m beginning to feel. I will be keeping my own dairy of the hip replacement surgery too help with the feeling of anxiety 😅. Thank you sincerely
Hi Evan. I’m glad it helped. Very best wishes to you!
I had the anterior approach, robotically assisted THR procedure 17 days ago and I’m pain free (in my hip) with only residual soreness in my thigh from the surgery. Now walking 3/4 mi./day with a cane for stability only. I won’t kid you, the first few days were rough, but mostly learning how to navigate moving and how not to move. Do exactly what your surgeon tells you to do, and especially what they tell you not to do. It works. My surgeon told me, ” You are unique, your hip is not”. At the beginning, the pain was very manageable with opioids and I only needed them for 3 days. It wasn’t bad. Anticipating the surgery is far worse than the experience. Once you have it done, you’ll be so focused on recovery, the anxiety will disappear. Be excited. YOU WILL BE FINE!
Fantastic advice and I am so happy to hear how well you are doing, Mike! Susan
Both the short term and lifelong restrictions after a hip replacement make me feel indescribably angry. How do I deal with that? Some of the suggestions I see online are economically impossible for me. Some of them might be fine at home, but cannot be put in to practice outside the home. Others seem achievable only in La La Land.
Hi Kristin – The recovery takes some time, but the long-term benefits of a new hip make it worthwhile. Yes the compression socks and girdle and requirement to ice are a lot initially. I am not sure what long-term restrictions you are referring to. I am able to do all I did before with the exception of running, high-impact aerobics and skiing bumps. Sending you my best!
I’m still in the “I’m too young for a hip replacement” stage … at 62! My ortho doctor told me I’m “bone-on-bone.” I’ve had one set of bilateral cortisone injections (both hips) and have my second set scheduled for next week, 5 months after the first injections. My doctor is great, not pushing me either way. He takes the time to answer all my questions, and he only does anterior replacements, which is “the better way” to go. But I’m still trying to figure out when the time is right! I want to continue playing pickleball!
Great to hear you like your doctor. I know it can feel like a tough decision. Best wishes.
So glad I stumbled on your blog. I’ve been oscillating about the surgery weighing living with hip pain vs loosing flexibility perhaps for the rest of my life. I really need my flexibility to do yoga to fully stretch out and to sit at a potter’s wheel which is definitely more than a 90° bend at the hip since you lean over the pot. *Globtrotter, can you bend over a touch the floor? Can you cross your legs to put your shoes on? And, can you sit on a low stool and lean over as if you were throwing a pot on a potter’s wheel? Thanks for your input
Hi Ramsey – Yes, I can do all of the things you asked about. My flexibility is great. Definitely discuss short and long-term expectations with your surgeon. You do have to limit certain movements in the first weeks following the surgery. They will explain all that. Sending you my very best! Susan
I had anterior hip replacement 2 years ago and I am very disappointed in the outcome. I cannot raise my leg to put socks or shoes on. Can’t cross my leg unless I do it manually. My leg is numb from groin to top of knee from center of thigh to my ITBand. I need the other hip done and dreading the thought of it. Been to 4 PT and massage therapy. Going to see a neurologist May 1st.
Oh Palma, I am so sorry to hear that you are dealing with these issues post surgery. You must be very frustrated. I hope the neurologist is able to provide some answers and help. Good luck!
Thanks for sharing this, I’m 37 and about to have my hip replaced this week. I’ve been struggling for 13 years (previously had hip surgery but not a replacement), so I’m really excited about the possibility about doing basic things like walking (and maybe even hiking!) but also nervous about the actual surgery and recovery, or if I will end up worse then I am already. Appreciate this share – thank you.
Dear Kristine, I am so sorry to hear of all the struggles you have had at such a young age. I hope your surgery went well! I am sure you were in great hands. I am sending you my very best in your recovery and hope that before long you will be out hiking and doing everything else you want to do! Warmly, Susan
Just stumbled across your blog, preparing for my THJR in 2 days time. It’s a relief to read that you have been able to resume an active life. Similar to you, I’m 47, diagnosed with hip dysplasia after years of attributing pain to other issues (ITB, hip flexors) and playing basketball for 30+years. I know I won’t be able to go back to basketball but good to know you have been able to enjoy other activities, and I’m looking forward to exploring new sports. About to read your recovery journey. Thanks for sharing your story.
Hi Tricia. Thanks for sharing your story. I hope your surgery went smoothly and very best wishes with the recovery. Susan
Hi I’m 49 years old and my journey is more scary since I’m a physician knowing what can go right and wrong at the same time , I have hip dysplasia too for which my surgery won’t be as simple as the conventional one . Being a doctor and and having an excellent orthopedics who is also specialist in complex hip reconstruction, I still feel unwell about surgery and how my life will be after my surgery assuming that no complications arise , one of the most common complication is dislocation which can happen at any time , I think my life will change and I’m not sure how much pain I will be experiencing after surgery and for how long . What will be my level of fitness , will I be walking without an assisted device ? Will I walk normal again ? I have been postponing my decision for years now but my doctor think that is now the time . How was your surgery experience with the hip dysplasia?
Hello. I know that all the uncertainties can feel scary. My recovery was mostly very smooth. I detail it week by week in the story. I did have some pain initially but it was quote manageable. I am sure it is harder knowing more about what can go wrong. Sending my best wishes!
This is definitely what I needed to read today. I’m 45 and just finding out this week that hip replacement maybe my only option after a year of so many other treatments. Your story makes me much more optimistic about the future.
Hi Jennifer, Glad to hear you feel encouraged and optimistic. I know it’s disheartening to get the news that you need a THR. Wishing you all the best! Susan
I have been having steroid injections in my right hip once a year for the last 5 years. Since I turned 65, it has now gotten to the point where I am having them every 3-4 months out of the year just to be able tolerate the pain. I went to see my orthopedic surgeon to discuss having a hip replacement and he explained the surgery to me and said that he performs the posterior type hip replacement. I’m confident in my doctor but I have always had this fear of having the surgery. We have scheduled my surgery for the end of this year. Now that I have read about everything involved with the recovery and how long I will be off my feet and going through PT makes me more anxious…Any advice?
Hi Renee – I really can’t offer advice as I am not an expert and everyone’s recovery is a little different. For me, the recovery required patience but really wasn’t that bad and my improved quality of life has been so worth it! Susan
I had my Anterior THJR 5 weeks ago right before my 49th birthday. I am also diagnosed with hip dysplasia at birth and a few more hip and back problems related to that. I had been getting injections for years that were no longer effective so surgery was my only choice. I must say that I didn’t take it as easy as I should have the first week and was in horrible pain through week two. Starting week two I was doing 4 simple PT exercises twice daily, icing and elevating 4 times a day and staring to feel like I was making progress. Now I see my physical therapist weekly, and am applying myself to the 10 exercises that I do at home twice a day. I saw my surgeon’s assistant at my 2 week post op and no follow up for 2 month and a half along with not getting a lot of aftercare advice on Don’ts has been frightening. I’m just now reading online that I probably won’t be able to sit indian style ever again. That has always been my least painful way of sitting since I was a kiddo. All in all I will be having my other hip replaced after I’m thoroughly recovered.
Dear Brittany. It’s great to hear you are so committed to your PT! FYI, I am able to sit “Indian style”. Best with your continued recovery!
I had the Anterior THR, and really never missed a beat! The easiest recovery because no muscles were cut.
Fantastic. Thanks for sharing.
I’m petrified of hip (I need both done) surgery due to the things I’ve read about how fatal fracture during surgery can be. But I am in so much pain I’ve become sedentary. How do I know if my bones are strong enough to avoid fracture during surgery?
Hi there – I was scared as well and of course there are risks with any surgery. Your surgeon should be able to put any risks in perspective for you. Susan
I am 74 and had a partial hip replacement 6 weeks ago. I fell on my tile floor at 2AM and out came the EMTS. I waited 27 hours for surgery but was drugged the entire time and remember nothing until I was in a hospital room. I signed a consent that I have no memory of signing. My daughter was my proxy and should have signed and been able to ask questions. After the surgery at my 4 week visit all was well. it is now six weeks and I drive and use a cane. It was a left side surgery. My daughter asked about the implant and we were told metal on metal. My daughter, a health professional asks had they not all been recalled in 2004-5. She mentioned . possible future problems and his response was that none of HIS patients had had problems. I asked if my own ortho could come and they said too high up the food chain and did not get called. Tour metal on metal is chrome and cobalt. Over time it can cause myriad symptoms, none of them good. I will probably call the manufacturer. Recommendation I read is to get blood baselines of chromium and cobalt. My go back to my ortho of 25 years to get an opinion about both the implant and bloodwork. also because I am on PPO medicare with a 2ndary I spent 2 weeks in an SNL with daily PT/OT. Except for my concerns about the implant it was a lot easier recovery than new knees, a rotator cuff repair, breast cancer and a few more. get off the narcotics as soon as you can and have a Tylenol regime. I have done that for 6 weeks
HI Catlin – thank you for sharing your story. It sounds like you are on the road to recovery. Wishing you all the best. Susan
I wish someone would talk about the mental aspect. It can be more scary than the physical pain.
I agree, the mental aspect is significant. I also had a lot of anxiety leading up to my surgery. Thanks for your comment.
I’m not sure when you had your surgery but thank you for this. I’m 48 years old and have a hip replacement scheduled in a month. I have been dealing with hip pain for 2 years. My first doctor told me I needed to wait till I was 55 and I left his appointment so disheartened. I finally decided this summer to get a second opinion and the surgeon told me I was a perfect candidate and not to wait any longer because my quality of life was more important. I cried when he told me that. Thank you for talking about your recovery. I honestly have no idea what to expect with an anterior hip replacement. I’m nervous but excited and so looking forward to not being in pain anymore. Thank you again for sharing.
Hi Bethany. I was 49 when I had my anterior replacement and also sought a second opinion in order to find teh right surgeon, so we have a lot in common. Very best wishes with your surgery. Susan
Hi Susan, I’m due for a THR in 2 days. Like others here I am terrified that I will never be able to manage my life again, and terrified of the pain. Reading your blog has comforted me greatly – thanks so much for sharing.
Hi Nionie. I am so glad it helped reassure you.Very best wishes with your surgery. Susan
Hi Jack here in scotland .just been diagnosed with osteoathritice in left hip .consultant said cam impingment with labrel tear.zaid would not push me towards surgery yet.i feel really down as been active all my life and ski 3 trips a season .even standing or 30min walk I in pain.cannot find any pain management.did not think would be able to ski again if get hip replacement.age 62.
Hi Jack, So sorry to hear this; I can relate to the pain and feeling down about giving up beloved activities. Fellow skier here and I was able to ski after surgery, once it had all fully healed. My doctor just advised I avoid bumps or any other impact exercise. Obviously speak to your surgeon about what you can do following surgery, timelines etc. Wishing you the best!
If metal on metal is recalled, what are surgeons using and what is the best materials used
HI Leona – This is often changing. I believe mine is a combo of metal, ceramic and plastic. Best, Susan
I needed to read this today! I am 41 and just had my THR clearance appt with my PHP:( I was a runner and often felt I had to move my hips around and into place before walking even in my 20’s, but I would take that back in a heart beat. The out of nowhere pain came at 37 about a year after my third babe (I think hip kiddo carrying didn’t do me any favors;) My doctor did an injection as a “test”, but it didn’t provide any pain relief, so I failed to believe his diagnosis and started trying to heal myself with every alternative therapy known to man! 4 years later I am still in pain with less mobility, although the pain has changed considerably…I gained a limp!? My biggest anxiety is that I go through with the life/body changing surgery and it doesn’t fix the root cause of my problem (possibly pelvic instability)…I would be DEVASTATED to continue on this way, but only now with a fake/limiting hip! Do you mind if I ask how long you had your pain before the surgery? What did you try before surgery? Did the pain change? How were the muscles around the hip? How was the other side? Did you develop crazy imbalances as I have?;) Either way, your positive experience was definitely what I needed today! THANK YOU
Hi Crystal. So sorry to hear you’ve been dealing with this. I had pain for months before surgery. I can’t now remember exactly how long but it had progressively gotten worse until constant pain and could barely walk. For me, there was no doubt that my hip was the problem because an x-ray showed the cartilage in my left hip joint was entirely gone; I had bone on bone arthritis. At that time, I was diagnosed with hip dysplasia on both sides which was the cause. I was born with it but never diagnosed. For some reason, my right side did not have the same arthritis as the left. To this day, 7 years later, it has not been a problem even though it also has hip dysplasia. I hope that answers some questions. Good luck getting to the root of the problem. For me a second opinion was very valuable. Best wishes to you, Crystal! Susan
Crystal, I am in the same boat as you. I have had hip pain since I had 4 falls in the spring but it doesn’t hurt where it should. I don’t have constant pain and I also had the hip corisone injections and they did nothing. I have been doing therapeutic massage and my muscles are super tight. It has helped but not totally done away with the pain. I also did PT and went to a chiropractor. I’ve had several xrays and all say I have severe arthritis. But I was also told by MD and PTs that just the xrays or MRI’s don’t tell the whole story and may look bad but if you don’t have pain, you don’t need a hip replacement. So I feel the same way worrying it won’t fix my problems. I can’t find a doctor who can tell me the pain is from my hips which is what I really want. If I do end up having surgery, I’m going with the SuperPath method. Have you seen a sports medicine doc?? They are more familar with soft tissue and pelvic issues.
Thanks for helpful comments as I am preparing for a hip and knee replacement. The pain is becoming the kind as “described as, ….barely able to walk. All very encouraging.
Glad it helped! Good luck Mariyah!
I’ve been trying to decide between getting the surgery or trying injections. I am scared of both. Do you know anything about the injections.
I did have an injection before my surgery. It was before a trip to Europe with my family and it was very helpful in giving me mobility. It helped for a few months, I’d say. It doesn’t seem to be a permanent solution. Susan
Hi Susan. I have scheduled THR with the same great Dr 7 times since Jan 2020. It has been cancelled 6 times & #7 will be cancelled tomorrow. 2 were because of Covid & the rest for various reasons. With Gods intervention on 2 occasions, (referral & conversation) I got a 2nd opinion today. I feel so much more comfortable about the surgery now. Something just wasn’t right. The first Dr is a #1 Dr here but I needed a different comfort level. Since I made the decision 2 weeks ago to do a 2nd opinion, I have had a peace in my soul. Yes, I am still anxious at times, I even whimpered at the appt today. I made the surgical date for 10/31/23. A lot to do & I will do it. #8 will be GREAT. Thank you for sharing & listening.
Thanks for much for sharing this. Great to hear you found someone who made you comfortable. I hope your surgery and recovery go well and you are on your way to better mobility.
How are you doing after surgery ? Sending prayers up for you Cathy
Hi Cathy. It’s 7 years later and I am still doing great. Healthy and happy, and very grateful. Susan
I am 68 1/2. Tish
I am a 69 year old male with bone on bone arthritis in my right hip. I have seen 4 surgeons in good hospitals and am told I am a good candidate for thr. I have had pain in the last 12 to 15months in my hip and now both knees are hurting me (structurally I have been assured that both knees are fine). However I am anxious about the surgery and pain after the surgery. My goals are walking pain free and being able to play golf again without having pain. Thanks for your blogs.
I can relate to the anxiety. Best wishes to you, Larry.
Thank you so much for sharing your journey. I can’t wait to read your Life after hip replacement entry. I’m 45 and have been struggling with hip pain and walking “ugly” for a few years or even longer. I can’t remember I just dealt with it. I was a fitness instructor and just pushed through until the pandemic. After PT, injections and struggling during my travels I’ve decided to get the THR and my doctor is using direct anterior approach. I keep reading my booklet he gave me over and over and I’m so nervous but looking forward to improvement in my quality of life. Thanks again for sharing and I look forward to reading more. I can’t wait to walk pain free in Africa next year !!!
Wishing you all the best with your surgery and recovery, Ebony. I was in Africa this year; it’s magical!
Hi and thanks so much for writing about this topic. I’m 67 yr old female outdoor enthusiast and getting an anterior hip replacement in 3 weeks. How do you know when you’re ready ? When you go from hip pain, to limping, to needing support to walk up hill or stairs. Or as my Dr said to me you’re ready when you come back to me and tell me you’re ready – he was so right! Took me 6 months to decide as I watched my mobility degrade. Mental angst – I get it. Never had surgery until 2 years ago when I fell and broke a wrist – so if your mental image is I’m a healthy, able person you need to keep thinking that IMHO and let the Dr. help revitalize you and keep that mental image of yourself a reality. Hope that helps. I’ll check in after the big day.
Hi Mary. I think you are right. Each os us will know when it’s the right time…for me the diminished mobility made it a clear decision. Very best wishes to you with the surgery. Please do let us know how you’re doing. Susan
Hi there. Three weeks ago, I had total hip replacement surgery, posterior. I have good days and I have bad days still. I can’t sleep at night because of pain and also I’m not a back sleeper – but right now that is how I’m supposed to sleep. Before surgery, I hurt for several years only to find out I was totally bone on bone. I am starting to question whether I should have gotten this surgery or not.
Hi Debbie, I am so sorry to hear that you are struggling with pain and sleeping. I also had good days and bad days and dealt with pain. I contacted my surgeon’s office when I had concerns that things might not be healing properly and that was helpful. You might want to do the same? Best wishes with your recovery! I hope things improve soon. Susan
I am about to have a replacement – I’m 54 and was a yoga teacher for years with a (stupid) insane practice that caused injury after injury and wear and tear. I’m now at zero medial rotation and 10% lateral rotation (insane when I could once stand up with my leg behind my head – please don’t try this, I’m quite certain this did for my hip). I’ve also got very little cartilage left and a constant catching in my groin … but aside from that, I don’t have a lot of pain and am still pretty active although massively compensating elsewhere in my body due to my very limited hip movement. I’m having a massive wobble about the whole thing, feeling really anxious and have spent the entire weekend talking myself out of the surgery. I spoke to a friend last night and a few other people I know who have gone through the replacement and they all said they feel great and don’t regret it and that it’s totally normal to feel anxious and doubtful. Any advice would be gratefully received!
Hi Sarah, Sorry for my delayed reply; I have been traveling. I appreciate you sharing your story and can so relate to the “massive wobble” as you called it. Like your friends, I don’t regret my surgery at all. And I agree that compensating with other parts of our body can cause other problems. I also felt very anxious ahead of surgery. Perhaps another conversation with someone at the surgeon’s office would help to put your mind at ease. Whatever you decide, I wish you the best.
Hi! I’m so glad to have stumbled on your blog. I have an appt with an Orthopedic surgeon in 6 weeks to discuss Direct Anterior Approach hip replacement. I am 59, am avid hiker and long stride walker. MRA of hip confirmed hip dysplasia, Osteoarthritis and zero cartilage in the joint. The worry that comes with the recovery and limits surrounding it has me stressed out, but the pain has taken away what I love to do. I appreciate your candor when describing your recovery. Thanks for sharing!
Hi Teri. I am so glad my story was helpful to you. Best wishes to you as you forge ahead to better mobility! Susan
Could you talk about the process of choosing a doctor for the surgery? Did you stay local or look for the “best” doctor in the state (eg US News & World Reports rankings)? What would be the disadvantages of being 2 hrs away from your doctor’s office? I’ve asked around, but can’t find anyone in my area whose had surgery near me.
Hi Janet. I started by asking for recommendations from friends for orthopedic surgeons. I didn’t like the first surgeon I met with so sought out another opinion. I believe I found my surgeon via a google search for doctors who performed the anterior method. Once I met with my doctor I knew he was right for me. I can’t really answer your questions about distance from the office. Mine was about a 40 minute drive; my husband came with me and was the driver. It was day surgery. There were multiple appointments required so you would have to do that drive each time. The doctor’s offie should be able to help answer that.
I had a similar situation with needing the surgery but I’m putting it off because I have a five year old at home and no bathroom on the same floor as me. Any thoughts on how long these things would be a major issue post surgery typically?
Hi. It’s hard to say for sure regarding your five year old. I needed help from my mom for about a week and my kids were teenagers. I could drive fairly soon but there’s a lot of icing etc that needs to happen. The bathroom was less of an issue. We have a small set of stairs and I was manging those fairly early on. Hope that helps.
Do you miss running? I’m looking at a hip replacement and I can’t imagine not being able to run anymore. Is it just for a while after surgery or is it never again?
I was advised to give up running entirely — both for the sake of my new joint and the hip dysplasia in my other hip. I now spin on a bike instead and love it. I don’t miss running, but was never a huge runner.
Hello, Susan. I am 53 and having a total hip replacement scheduled for June 14, 2024. I still have about three more months to wait until surgery. I can barely walk and wondering if you have advice on pain management until surgery. I take Advil and Aleve right now. I also wondered about losing weight. I have put on 10-15 pounds due to not being able to exercise the way I use to. I think if I lose the weight it could help ease the pain. Any advice?
Hi Raylenne, I am so sorry to hear you are dealing with pain while you wait for surgery. I have no idea if weight loss would help. I think that would be a question for you doctor. I did have a steroid shot in my hip joint which gave me relief for a few months, before I went ahead with surgery. You might inquire if that’s an option for you. Sending you my best wishes! Susan
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
FOR UPDATES & MIDLIFE INSPIRATION
Please check your email for confirmation.
I’m glad you’re here. Can we talk about midlife? I reached my late 40’s, realized my kids were growing up, and adventure began calling in a new way: big travel adventures as well as everyday ones. I want Midlife Globetrotter to be a place where we explore how to add a sense of fun, freedom and meaning to these precious years. Let’s celebrate how far we’ve come, and all that’s ahead.
LET'S CONNECT!
- Destinations
- Travel Planning
- Solo Travel
- Make Travel Matter
More to Explore

Why a Momcation is Good for You and Your Family

Getting Healthy & Fit at Fifty

My Emotional Upheaval at Midlife

Life After a Hip Replacement – My Story

Making Yourself a Priority at Midlife
Quick links.
© COPYRIGHT Midlife Globetrotter 2020-2024
Privacy & Disclosures
- Workers' Compensation
- OrthoAccess ® | Immediate Care
- Request An Appointment
Running After Hip Replacement: Yes, It Can Be Done and This Patient Ran a Marathon
With more than 500 completed races to his credit, you could say Tom is passionate about running, but most recently, he wondered what it would be like running after hip replacement surgery .
He started his running career in high school where he participated in cross country and spent the bulk of his adult life running in 5Ks, then graduated to 10Ks and half marathons.
“I didn’t run my first marathon until I was 40 in 2002,” Tom says.
Over the course of a couple of decades, Tom injured his knees and developed arthritis in one of his hips.
This blog describes Tom’s running after hip replacement experience, including what led him to IBJI orthopedic surgeons and how he finished a marathon just two years after surgery.

Running After Hip Replacement and Knee Surgeries
“I had meniscus surgery on both knees in 2003 and 2004,” Tom says, adding that he sought out care from three IBJI physicians - David Raab, MD , the late Philip Fitzsimons, MD, and Gregory Portland, MD . The surgeries were successful and Tom hasn’t had any significant knee problems since.
The Journey to Running After Hip Replacement
Although his knee problems were cured and he went back to running, Tom’s right hip started to give him pain about five years ago. He learned he had arthritis and that he would eventually need surgery when it became too painful.
Yes or No to Running After Hip Replacement?
Most orthopedic surgeons don’t recommend running after hip replacement, but Michael O’Rourke, MD had an optimistic approach, according to Tom.
“He didn’t prohibit running like some other doctors,” Tom says. “A friend of my wife’s had surgery with him and he told her she could get back to some running. I found that to be very encouraging and that’s why I chose Dr. O’Rourke.”
Tom’s hip was bone-on-bone and he was still running, but he figured he would have to retire after running his 20th marathon. After all, it was a nice round number, he said.
Running after hip replacement in a marathon or even a shorter course wasn’t something he thought possible. Surgery, he knew, was definitely going to be his next step.
Running After Hip Replacement Becomes a Reality
At the beginning of 2019, Tom decided to have total hip replacement surgery with Dr. O’Rourke. He ran the Boston Marathon that April, then had the surgery in June.
He says he was literally walking in the hospital that day, and climbing stairs the next.
He spent two nights in the hospital and was home without needing crutches. It looked like running after hip replacement wasn’t a far-fetched dream. “I was running by September, and doing 5K races again in October.”
Running After Hip Replacement During COVID
When COVID hit, it seemed like running in any race - whether it was running before or running after hip replacement - was out of the question.
“I ran with my running club in Evanston ,” Tom says, “but there really weren’t any races to do in 2020. I did a half marathon in May of 2021. Most of my friends were going to be doing fall marathons.”
Over the summer of 2021, he gradually increased the distance of his weekend long runs. “I played it by ear and my hip seemed to be doing fine,” he says. “I found it to be easy to run with my friends, so I ran with them.”
Tom comfortably worked up to 15 miles with them, then 18, and realized that he could participate in a fall marathon.
Running After Hip Replacement: Tom Registers for the New York Marathon
“I decided on New York City because I’d run it twice before and it is one of my favorite marathons for the excitement of the crowds,” Tom says. “Chicago was an option, but on Columbus Day, it can be warm here, while New York in November is reliably cool.”
A Funny Thing Happened While Running After Hip Replacement
As Tom got back to regularly training with his running club, he was doing a Saturday morning long run with several other runners when he encountered a familiar face on Sheridan Road in Kenilworth. “A couple was walking towards us with their dog,” Tom says. “It turned out that it was Dr. O’Rourke. I wondered how he would feel knowing his total hip replacement patient was out doing a 20-mile run.”
Running After Hip Replacement: Finishing 26.2 Miles
“I was able to do five 20-mile training runs in preparation for New York City,” Tom says, adding that his running club was paramount to his success. “On the day of the marathon, the weather was perfect for running and I was able to complete the 26.2 miles just fine.”
Tom used the race to fundraise for the Michael J. Fox Foundation , supporting research for Parkinson’s Disease.
Running After Hip Replacement: How Tom Placed
Tom’s time for the 2021 TCS New York City Marathon was four hours and 17 minutes. He was happy with the result, finishing in the top 40 percent of runners.
He says it was difficult to conquer the bridges and rolling hills since his training was mostly along Illinois’ flat terrains, but he was able to do it without pain.

Hope for Running After Hip Replacement
Tom attributes his successful and pain-free running after hip replacement to physical therapy sessions at the IBJI Wilmette Physical Therapy location.
He got the positive mental attitude about running after hip replacement from his own personal research.
“I went to hiprunner.com which was full of stories of people who had come back after total hip replacement surgery to do marathons,” Tom says. “I knew that despite all that I had read about it being a death sentence for running, I saw stories of people who had done it.”
There also was a woman in his own running club who, running after hip replacement, completed the BMW Berlin Marathon .
Running After Hip Replacement Surgery: Will the Other Hip Hold?
Tom gets asked about his left hip, and whether or not it has arthritis. He doesn’t know what caused his painful hip arthritis , but so far, his non-surgery hip is doing fine. It could have been genetics — his mother had both hips replaced — or it could have been that he runs a lot.
Tom knows he may wear out his new hip, but he tells people that he’d rather have orthopedic problems from running and live into his 90s than to not run and possibly develop cardiac problems in his 60s.
“I was able to recover and bounce back pretty quickly,” Tom says. “It helps that I was 56 at the time of the hip replacement. I am one of the younger, fitter patients as far as joint replacement goes.”
Running After Hip Replacement: Reaping the Rewards
Tom’s love of running isn’t just about the physical high he gets. “It’s where I make my friends,” he says. “It would have been really tough if the surgery were a death sentence for my running.”
What Does the Future Hold for Running After Hip Replacement?
Tom says he plans to pace himself in the future by doing a half marathon in January 2022 and possibly another marathon in the fall. “I’m definitely going to keep going,” he says.
Referring Others Who Want to Run After Hip Replacement
“When anybody asks me, I tell them Dr. O’Rourke did my surgery,” Tom says. “It was successful and at this point, I’m very grateful and appreciative that I’m still able to run.”
Running After Hip Replacement: Learn More
You may be wondering about what is involved with a hip replacement surgery . Check out the IBJI OrthoInform Podcast featuring Dr. O’Rourke’s total hip replacement episode . You can also download our Ultimate Guide to Hip Pain Relief to get all the details about what causes hip pain and the treatments available to help you get back to feeling your best.
Please note: Patients' results may vary.

- Email Address *
- IBJI OrthoInform Podcast Listen to Episodes
- Move Better Magazine View Publications
Search the site
Hip replacement journey.
There are three resources to help you prepare and then recover from your hip replacement surgery.
The first is an education class presentation which will guide you through the entire journey and is a MUST W ATCH
To support this there is the ‘Your Personal Guide to Hip Replacement Surgery’ booklet.
Lastly, there are also bite-size video clips which you can go to as many times as you need. These videos will be most appropriate at various time throughout the journey.
2. Your Personal Guide to Hip Replacement Booklet which will be sent to you in the post, or alternatively you can view it by clicking on this link HERE .
3. Video Clips We have created a series of short video clips which follows your hip replacement journey from beginning to end. Please watch these at your leisure and refer back to them at the relevant stage of your journey. If you can bring in a portable computer/tablet, it would be helpful to watch these again whilst in hospital. Although we would like you to watch all the videos before your surgery date, they have separated into pre , during and post your hospital admission. The Orange videos cover the time between now and your admission to hospital. The Yellow videos relate to your hospital stay. And finally, the Green videos guide you through your rehabilitation after you leave the hospital. Please click on the 'Next-Stage' icon at the bottom of the page to see the next series of videos.
Useful Websites

Organisational structure
Board of directors.
- Who's who
- Working with partner organisations
Meetings and papers
- Board Meetings
- Annual General Meeting (AGM)
- Council of Governors
- Charity Trustee
- Charity Trustee Meeting
- Charity Trustee meeting
Objectives, values and strategy
- Why we care
- Sustainability
Equality, diversity and inclusion
- Publications and reports
- Publications
- Performance and staffing
- Fraud Awareness
- Safeguarding - adults and children
- Patient Forum
- Questions or concerns about your care, or the care of a friend or relative
Research at SWFT
- Research Department - Performance
MySWFT staff app
- MOBILE PRIVACY STATEMENT
- Veterans Covenant Healthcare Alliance

Our services
- Adult in-hospital services
- Adult out-of-hospital services
- Children, young people and family services
Find services near you
- Service Locations
- SWFT Supporters
- Video Consultations
- Patient Portal – MyCare in Warwickshire

Looking after me
- Community pharmacists
- Coventry and Warwickshire Integrated Care Record (ICR)
- Health2Home - online shop for health products
Health and wellbeing
- Advice for carers
- Alcohol advice and information
Eating well with SWFT
- Food for inpatients
- General Wellbeing- The How Are You Quiz
- Healthy Ageing
- Keeping active
- Mental health and wellbeing
- Norovirus and winter bugs advice
- Sexual health and wellbeing services
- NHS Warwickshire Stop Smoking Services
- Weight management
- Health and Wellbeing Events
Health and Wellbeing hubs
- Help us manage demand for our services this winter
- There's no place like home
- Local organisations, groups and agencies for advice and support services
- Monkeypox patient information
- Patient information leaflets
- Rising cost of living
- Return Scheme for Walking Aids
- Warwickshire Wheelchair Service

Our hospitals
- Consultant directory
Warwick Hospital
- Visitor information
- Staying in hospital
- Same sex accommodation
- Car parking
- Keeping you safe
- Department of Chaplaincy and Spiritual Care
Leamington Spa Hospital
Stratford hospital.
- The Grafton Suite
Stratford Hospital- Building One
- Stratford Hospital- Health and Well Being Information Centre
- Café and Lomas Suite
- Health and Wellbeing Information Centre
- Lomas Suite
- Digital Innovation Hub
Ellen Badger Hospital
- A new Ellen Badger Hospital
- Do I need a joint replacement?
- Find a Doctor

Travel after Joint Replacement Surgery
You may be worried about traveling in the first months following surgery. One concern is sitting in a car or airplane seat for long stretches of time and the risk of forming a blood clot in your leg – also known as deep vein thrombosis (DVT). Several studies have shown that, if appropriate measures are taken , it is safe to travel soon after your joint replacement without an increased risk of developing a blood clot for most patients.
If you have a higher than normal risk factors for blood clots, it is important to have a discussion about post-surgery travel plans with your primary care physician and surgeon prior to joint replacement because DVT is a serious condition that can be life threatening. This may potentially affect your surgeon’s choice of medication to prevent blood clots after surgery.
Most people will feel safe to travel within a few weeks of surgery; however, keep in mind that your comfort level may also play an important role in determining when you are ready to take a long trip. Anticipate that you may be more sore, stiff or swollen when traveling within a few weeks of surgery. This increase in discomfort will likely be short-lived, but you may experience a slight setback in recovery and should have a plan in place to address any increase in pain. Depending on the progress of your recovery, you may find it easier to use a cane, crutches or a walker (or at least have one available) when traveling even if you were not using them prior to the trip.
What precautions should I take when traveling with my joint replacement?
In general, there is an increased risk of developing a blood clot immediately after surgery whether or not you plan to travel long distance. If appropriate measures are followed, these risks can be minimized and make it possible to travel soon after surgery. These precautions include using compression stockings , and/or mobile compression devices and taking medication that can range from aspirin to prescription blood thinners to prevent a blood clot. We recommend continuing the use of these preventive methods when traveling. These are other precautions that can be beneficial and are recommended:
- Walk and move around frequently. This can consist of basic stretching and getting up to walk the aisle of the plane or stopping the car to walk every one to two hours.
- Do calf squeezes and ankle pumps to keep the circulation in your legs moving.
- Pull your knees to your chest to stretch your legs.
- Stay well hydrated by drinking plenty of fluids like water and juice. Avoid dehydrating beverages like coffee and alcohol.
If you are planning to travel after your joint replacement, please discuss this with your surgeon before your surgery so you can both work together in developing a customized plan for a safe journey.
More information concerning travel and the risk of blood clot along with the symptoms of DVT and pulmonary embolism can be found on the US Centers for Disease Control website .
See also “ Will my artificial joint set off airport security metal detectors? ”
- Ball ST, Pinsorsnak P, Amstutz HC, Schmalzried TP. Extended travel after hip arthroplasty surgery. Is it safe? J Arthroplasty 22(6 Suppl 2): 29, 2007
- Cooper HJ, Sanders SA, Berger RA. Risk of symptomatic venous thromboembolism associated with flying in the early postoperative period following elective total hip and knee arthroplasty. J Arthroplasty 29(6): 1119, 2014
- Nwachukwu BU, Dy CJ, Burket JC, Padgett DE, Lyman S. Risk for Complication after Total Joint Arthroplasty at a Center of Excellence: The Impact of Patient Travel Distance. J Arthroplasty 30(6): 1058, 2015
Print Friendly
Print a copy of this article.
This article has been written and peer reviewed by the AAHKS Patient and Public Relations Committee and the AAHKS Evidence Based Medicine Committee. Links to these pages or content used from the articles must be given proper citation to the American Association of Hip and Knee Surgeons.
- Dance Magazine
- Dance Spirit
- Dance Teacher
- The Dance Edit
- Events Calendar
- College Guide
- Newsletters

After Hip Replacement, PBT’s Jessica McCann Is Back Onstage and Sharing Her Recovery Journey
In December 2022, Pittsburgh Ballet Theatre soloist Jessica McCann learned that her right hip was the equivalent to that of a 90-year-old’s. Bone spurs, calcium deposits, and a ready-to-rupture bone cyst could cause permanent damage, her doctors told her. Without a hip replacement, she would not be able to continue to dance professionally.
Stop dancing? McCann wasn’t having any of that.
She had put off addressing her growing hip pain long enough, and, like an increasing number of dancers with significant hip damage and deterioration, she opted for the surgery.
On April 21, 2023, the California native, then 32, had her right hip replaced at the Hospital for Special Surgery in New York City. Less than a week later, she was walking without crutches. By August, she was back in the studio for her ninth season with PBT. In October, she returned to the stage looking better than ever, performing in Annabelle Lopez Ochoa’s acrobatic Lacrimosa .
For McCann, the unknown was not whether she would return to dancing, but the lack of information and support she found in going about her surgical journey. Below, McCann shares why she wants to be an advocate and resource for other dancers who need to have a hip replacement and want to return to performing.
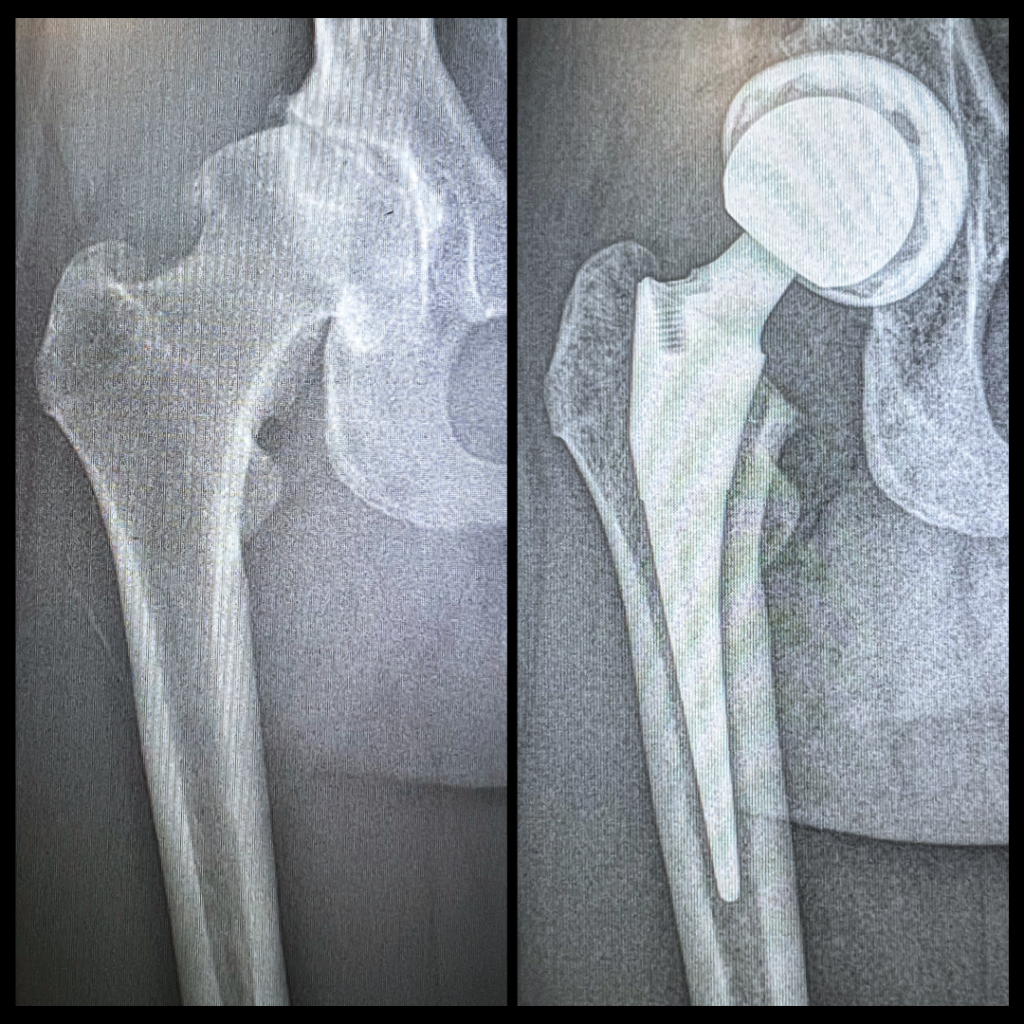
When you found out that you needed a total hip replacement, what kind of information was available?
There was not a lot of information that I could find about hip replacements in ballet and returning to dancing. There was only information about hip resurfacing and examples of dancers who had hip replacements after their performance careers. It felt incredibly isolating, and I had to forge my own way.
What was the main thing you were looking to find out?
If it was possible to have a hip replaced and continue my dance career. In my head, I was determined it would be possible. I never considered retiring for one second throughout the entire process.
What were a few of the most important things you learned about a hip replacement that you want to pass along to other dancers?
Find a surgeon who wants to work with your goals. I wanted the greatest range of motion for dancing. The technology is there to have a hip replaced and continue your career. I received the new dual mobility hip replacement from Dr. Edwin Su in New York City, who had done similar surgeries on other dancers and understood the range of motion I was trying to achieve.

What do you want others to know about ignoring pain and putting off surgery?
I waited too long. I was in so much pain that I couldn’t take class, and my husband had to carry me around so that I could still perform. I would definitely recommend if you are having pain, that you find out what it is. The sooner you know what is going on with your body, the sooner you can fix it.
What was the most challenging part of your recovery?
Patience. You have to allow your body to heal while you’re strengthening it. Don’t skip any steps in the recovery process or overdo it. Love yourself and your body and let it do its job.
What ballet steps were the hardest to get back to doing?
I had to retrain my body to do specific steps. It took months to get my arabesque back, but now I can make all the proper ballet positions, which blows my mind.
How do you think knowing someone like you, who went through the surgery, would have helped during your hip replacement journey?
It would have been that bright light I needed. Support is so important. I felt like I went through a grieving process. I was in denial. Some days, I would be very upset, and others, I would sit in my car and cry because I didn’t have anyone who understood what I was going through or any examples of others who went through the same process. It was more complicated than it needed to be, and if I had that support, it would have been a lot easier. I want to be that bright light for others and let them know they can do this, and here are the steps.

You’ve chronicled your surgery and recovery; how can people hear about your story or contact you for information that might help them?
I talk about my journey in several episodes of my podcast, Two Women Two Worlds , with former dancer Tilda Karine (available on Apple Podcasts and Spotify). On my Instagram page ( @flexiejaybird ), there are updates on my recovery, and you can see videos on how I am actually moving. People can message me there for information and advice.
Why is it important to you to help others going through this process?
Because of the lack of information. I have had so many professional dancers reach out to me, wanting to know what kind of hip replacement I had, what doctors to go to, and everything I have learned.
Do you have a personal message you want to say to dancers about to embark on this same surgery?
You’re not alone—others are going through the same thing. Don’t be afraid to ask for help. The recovery time is fast compared to other surgeries. Determination and goal setting are crucial to getting back onstage. You have to really want it. The mental game and strain were hard, but it was so worth it for me.

How an Injury Led Seth Orza to Build a New Ballet Shoe and a Post-Performance Career

What Happens to Audition Materials After You Press “Send”?

Rediscovering Madame Mariquita, the Prolific Choreographer Who Helped Modernize French Ballet

Madison Ballet Comes Into Its Own Under Director Ja’ Malik

Want to keep reading? Only Pointe+ members can view this story.
Get access to exclusive ballet content and ways to take your dancing to the next level.
Dear Doctor: Orthopedic surgeon comments on close connection between hip join, knee pain
- Published: Mar. 28, 2024, 5:55 a.m.

Often knee pain is related to problems in the hip joint. Getty Images. Getty Images
- Dr. Keith Roach
DEAR DR. ROACH: I read your recent column about a person who had knee pain after a knee replacement. I am a retired orthopedic surgeon who performed on over 10,000 total joints of the hip, knee and shoulder in my 47 years of active surgical practice. A well-done total knee replacement does not give the patient much pain postoperatively. I saw many patients who had this story in my career, and the first thing that comes to mind is that the patient was having referred pain to the knee from an arthritic hip joint.
Oftentimes, the surgeon who performed a painful knee replacement never X-rayed the hip or did a complete exam to look for a limited range of motion in the hip. The patient who has knee pain after a total knee replacement needs to have an examination and X-ray of the hip.
I saw more than a few patients who had surgery on their knee when it was their arthritic hip causing referred knee pain that was the real diagnosis. In this case, performing a total hip replacement may eliminate the pain completely. Qualified orthopedic surgeons will agree with me in this case. My advice to inexperienced surgeons is: “Always check the hip before jumping into a total knee replacement!” -- Gary Wolfgang, M.D., Retired Orthopedic Surgeon
ANSWER: I thank Dr. Wolfgang for writing and for the important reminder of the close connection between the knee and hip. It isn’t that the knee doesn’t have any problems; it’s that there may be more than one cause for knee pain, and I have certainly seen, as Dr. Wolfgang has, many patients with knee pain whose pain was actually due to a hip problem. So, replacing the knee won’t help the hip, which is the underlying cause of the pain.
DEAR DR. ROACH: I have just had my prostate gland surgically removed three weeks ago, and I am experiencing incontinence because of the surgery. I am worried that if I drink my usual amount of 8 glasses of water a day, like I did in the past, I will be inside the bathroom more than I am outside of it.
What is your opinion on this issue of not drinking enough water because of my fear of bathroom trips? Do you think I should just keep drinking water and not care about the trips to the bathrooms? -- M.G.
ANSWER: Some degree of incontinence is extremely common after surgery for prostate cancer. But you will be glad to hear that over time, most men regain much better control over their bladder function. The rates of complete continence are much higher one month after surgery compared to one week, and the rates continue to improve months or even years after surgery. The use of pelvic floor muscle training also speeds up the recovery of bladder control.
In the short-term, you absolutely need to stay well-hydrated, especially after surgery, but this doesn’t mean you need to force down fluids. Most people don’t need 8 glasses a day; 4 is enough. Thirst remains an excellent guide of whether you need fluids or not.
More advice
- Ask Amy: Request for an ‘open marriage’ probably means his wife has found someone new
- Dear Abby: Grieving daughter hurt by insensitive Facebook post about her mother's death
- Dear Doctor: Long-lasting bad cough could be due to several issues. Asthma is most common
- Miss Manners: April 1st birthday results in years of pranks, jokes. Please can it just stop?
- People’s Pharmacy: Does this sleep aid actually cause restless leg syndrome?
Dr. Roach regrets that he is unable to answer individual letters, but will incorporate them in the column whenever possible. Readers may email questions to [email protected] or send mail to 628 Virginia Dr., Orlando, FL 32803.
(c) 2022 North America Syndicate Inc.
All Rights Reserved
If you purchase a product or register for an account through a link on our site, we may receive compensation. By using this site, you consent to our User Agreement and agree that your clicks, interactions, and personal information may be collected, recorded, and/or stored by us and social media and other third-party partners in accordance with our Privacy Policy.

Knee pain may be linked to the hip
Q: I read your recent column about a person who had knee pain after a knee replacement. I am a retired orthopedic surgeon who performed on over 10,000 total joints of the hip, knee and shoulder in my 47 years of active surgical practice. A well-done total knee replacement does not give the patient much pain postoperatively. I saw many patients who had this story in my career, and the first thing that comes to mind is that the patient was having referred pain to the knee from an arthritic hip joint.
Oftentimes, the surgeon who performed a painful knee replacement never X-rayed the hip or did a complete exam to look for a limited range of motion in the hip. The patient who has knee pain after a total knee replacement needs to have an examination and X-ray of the hip.
I saw more than a few patients who had surgery on their knee when it was their arthritic hip causing referred knee pain that was the real diagnosis. In this case, performing a total hip replacement may eliminate the pain completely. Qualified orthopedic surgeons will agree with me in this case. My advice to inexperienced surgeons is: “Always check the hip before jumping into a total knee replacement!”
Gary Wolfgang, M.D.,
retired orthopedic surgeon
A: I thank Dr. Wolfgang for writing and for the important reminder of the close connection between the knee and hip. It isn’t that the knee doesn’t have any problems; it’s that there may be more than one cause for knee pain, and I have certainly seen, as Dr. Wolfgang has, many patients with knee pain whose pain was actually due to a hip problem. So, replacing the knee won’t help the hip, which is the underlying cause of the pain.
Q: I have just had my prostate gland surgically removed three weeks ago, and I am experiencing incontinence because of the surgery. I am worried that if I drink my usual amount of eight glasses of water a day, like I did in the past, I will be inside the bathroom more than I am outside of it.
What is your opinion on this issue of not drinking enough water because of my fear of bathroom trips? Do you think I should just keep drinking water and not care about the trips to the bathrooms?
A: Some degree of incontinence is extremely common after surgery for prostate cancer. But you will be glad to hear that over time, most men regain much better control over their bladder function. The rates of complete continence are much higher one month after surgery compared to one week, and the rates continue to improve months or even years after surgery. The use of pelvic floor muscle training also speeds up the recovery of bladder control.
In the short-term, you absolutely need to stay well-hydrated, especially after surgery, but this doesn’t mean you need to force down fluids. Most people don’t need eight glasses a day; four is enough. Thirst remains an excellent guide of whether you need fluids or not.
Q: I am a 79-year-old woman who weighs 123 pounds and exercises with Zumba, yoga and cardio drumming. I feel well and have plenty of energy, friends, support and family. I have been on a low-salt eating program to treat Meniere’s disease for 25 years. My blood pressure is 115/69 mm Hg.
My doctor recently retired, so my new doctor took blood tests and discovered that I had an estimated glomerular filtration rate (eGFR) of less than 59. They sent me to a nephrologist, and the nephrologist said to cut down my total liquid intake to 7-8 cups a day and up my protein to 80-100 grams a day.
This seem contrary to everything I have ever heard. Eating more protein is not hard, but I’m feeling tired, deprived and constipated from such little liquid. Can you explain why I would be directed to drink so little liquid? Can I find a dietary plan to help with this variety of ailments?
A: This advice is contrary to what I was taught and what is published in the literature — so much so that I wonder if there wasn’t a miscommunication.
Protein restriction has been part of the standard of care for decades, and its benefit in preventing progression to dialysis or a transplant has been shown in many studies. For a 56-kilogram woman like yourself, your goal would be 35-45 grams of protein per day. Some studies have also shown that plant-based protein may have benefits over animal protein.
People with chronic kidney disease are at risk for fluid overload and low sodium levels, which can be dangerous. However, restricting you to 2 liters is not usually necessary, and given your current symptoms, it isn’t the best idea, unless the nephrologist knows something that I don’t. (For example, if you already had a low sodium level, modest fluid restriction would be appropriate.)
Q: I take 20 mg of famotidine and have for years. Is this safe to take daily? I’ve tried looking up the answer online and get a lot of conflicting results.
A: In an ideal world, it would be great if you didn’t have to take any medications. However, reflux disease is very common; about 20% of the North American population has this symptomatic disease, with an even higher prevalence in older ages.
Lifestyle changes are the first line of treatment. Avoidance of food triggers, weight loss if appropriate, elevation of the head of your bed, and avoiding eating at least two hours before bed are among the most effective. Smoking and excess alcohol use should be stopped.
When lifestyle changes aren’t enough, a histamine-2 blocker like famotidine is a reasonable option, especially for someone with intermittent symptoms. Side effects are rare, and if you haven’t had them yet, you aren’t likely to get them. Proton pump inhibitors like omeprazole have more clearly defined risks with long-term use, so these should be reserved for when they are truly necessary. Famotidine starts working quickly, while omeprazole and similar drugs take days to work.
Dr. Roach regrets that he
is unable to answer individual letters, but will incorporate them in the column whenever possible. Readers may email questions
to [email protected] or send mail to 628 Virginia Drive, Orlando, FL 32803.

Lewiston Sun Journal
Account Subscription: ACTIVE
Questions about your account? Our customer service team can be reached at [email protected] during business hours at (207) 791-6000 .
Pain after a total knee replacement might be due to the hip

You are able to gift 5 more articles this month.
Anyone can access the link you share with no account required. Learn more .
With a Lewiston Sun Journal subscription, you can gift 5 articles each month.
It looks like you do not have any active subscriptions. To get one, go to the subscriptions page .
Loading....

Dr. Keith Roach
DEAR DR. ROACH: I read your recent column about a person who had knee pain after a knee replacement. I am a retired orthopedic surgeon who performed on over 10,000 total joints of the hip, knee and shoulder in my 47 years of active surgical practice. A well-done total knee replacement does not give the patient much pain postoperatively. I saw many patients who had this story in my career, and the first thing that comes to mind is that the patient was having referred pain to the knee from an arthritic hip joint. Oftentimes, the surgeon who performed a painful knee replacement never X-rayed the hip or did a complete exam to look for a limited range of motion in the hip. The patient who has knee pain after a total knee replacement needs to have an examination and X-ray of the hip. I saw more than a few patients who had surgery on their knee when it was their arthritic hip causing referred knee pain that was the real diagnosis. In this case, performing a total hip replacement may eliminate the pain completely. Qualified orthopedic surgeons will agree with me in this case. My advice to inexperienced surgeons is: “Always check the hip before jumping into a total knee replacement!” — Gary Wolfgang, M.D., Retired Orthopedic Surgeon ANSWER: I thank Dr. Wolfgang for writing and for the important reminder of the close connection between the knee and hip. It isn’t that the knee doesn’t have any problems; it’s that there may be more than one cause for knee pain, and I have certainly seen, as Dr. Wolfgang has, many patients with knee pain whose pain was actually due to a hip problem. So, replacing the knee won’t help the hip, which is the underlying cause of the pain. DEAR DR. ROACH: I have just had my prostate gland surgically removed three weeks ago, and I am experiencing incontinence because of the surgery. I am worried that if I drink my usual amount of 8 glasses of water a day, like I did in the past, I will be inside the bathroom more than I am outside of it. What is your opinion on this issue of not drinking enough water because of my fear of bathroom trips? Do you think I should just keep drinking water and not care about the trips to the bathrooms? — M.G. ANSWER: Some degree of incontinence is extremely common after surgery for prostate cancer. But you will be glad to hear that over time, most men regain much better control over their bladder function. The rates of complete continence are much higher one month after surgery compared to one week, and the rates continue to improve months or even years after surgery. The use of pelvic floor muscle training also speeds up the recovery of bladder control. In the short-term, you absolutely need to stay well-hydrated, especially after surgery, but this doesn’t mean you need to force down fluids. Most people don’t need 8 glasses a day; 4 is enough. Thirst remains an excellent guide of whether you need fluids or not. * * * Dr. Roach regrets that he is unable to answer individual letters, but will incorporate them in the column whenever possible. Readers may email questions to [email protected] or send mail to 628 Virginia Dr., Orlando, FL 32803. (c) 2024 North America Syndicate Inc. All Rights Reserved
Success. Please wait for the page to reload. If the page does not reload within 5 seconds, please refresh the page.
Enter your email and password to access comments.
Forgot Password?
Don't have a commenting profile? Create one.
Hi, to comment on stories you must create a commenting profile . This profile is in addition to your subscription and website login. Already have a commenting profile? Login .
Invalid username/password.
Please check your email to confirm and complete your registration.
Create a commenting profile by providing an email address, password and display name. You will receive an email to complete the registration. Please note the display name will appear on screen when you participate.
Already registered? Log in to join the discussion.
Only subscribers are eligible to post comments. Please subscribe or login first for digital access. Here’s why .
Use the form below to reset your password. When you've submitted your account email, we will send an email with a reset code.
Send questions/comments to the editors.
Spring storm could bring a foot of snow to parts of Maine
Leeds man charged with murder in connection with windham man’s disappearance, frustration reigns as a warm winter melted hopes for outdoor maine pursuits, watch the story from nbc news on the sun journal and national trust for local news, tracy jean’s coffee boutique closes in lewiston, moves to bath, member log in.
Please enter your username and password below. Already a subscriber but don't have one? Click here .
Not a subscriber? Click here to see your options
- Join Our Newsletter
- Post a Listing
- Your Listings
- Your Profile
- Your Subscriptions
- Payment History
- Sign up for Daily Headlines
- Sign up for Notifications
Your Good Health: Hip might be causing pain after knee surgery
- Share by Email
- Share on Facebook
- Share on LinkedIn
- Share via Text Message

Dear Dr. Roach: I read your recent column about a person who had knee pain after a knee replacement. I am a retired orthopedic surgeon who performed on over 10,000 total joints of the hip, knee and shoulder in my 47 years of active surgical practice.
A well-done total knee replacement does not give the patient much pain post- operatively. I saw many patients who had this story in my career, and the first thing that comes to mind is that the patient was having referred pain to the knee from an arthritic hip joint.
Oftentimes, the surgeon who performed a painful knee replacement never X-rayed the hip or did a complete exam to look for a limited range of motion in the hip. The patient who has knee pain after a total knee replacement needs to have an examination and X-ray of the hip.
I saw more than a few patients who had surgery on their knee when it was their arthritic hip causing referred knee pain that was the real diagnosis. In this case, performing a total hip replacement may eliminate the pain completely. Qualified orthopedic surgeons will agree with me in this case.
My advice to inexperienced surgeons is: “Always check the hip before jumping into a total knee replacement!”
Gary Wolfgang, M.D., Retired orthopedic surgeon
I thank Dr. Wolfgang for writing and for the important reminder of the close connection between the knee and hip. It isn’t that the knee doesn’t have any problems; it’s that there may be more than one cause for knee pain, and I have certainly seen, as Dr. Wolfgang has, many patients with knee pain whose pain was actually due to a hip problem. So, replacing the knee won’t help the hip, which is the underlying cause of the pain.
Dear Dr. Roach: I have just had my prostate gland surgically removed three weeks ago, and I am experiencing incontinence because of the surgery. I am worried that if I drink my usual amount of eight glasses of water a day, like I did in the past, I will be inside the bathroom more than I am outside of it.
What is your opinion on this issue of not drinking enough water because of my fear of bathroom trips? Do you think I should just keep drinking water and not care about the trips to the bathrooms?
Some degree of incontinence is extremely common after surgery for prostate cancer. But you will be glad to hear that over time, most men regain much better control over their bladder function.
The rates of complete continence are much higher one month after surgery compared to one week, and the rates continue to improve months or even years after surgery. The use of pelvic floor muscle training also speeds up the recovery of bladder control.
In the short-term, you absolutely need to stay well-hydrated, especially after surgery, but this doesn’t mean you need to force down fluids.
Most people don’t need eight glasses a day; four is enough. Thirst remains an excellent guide of whether you need fluids or not.
Dr. Roach regrets that he is unable to answer individual letters, but will incorporate them in the column whenever possible. Readers may email questions to [email protected].
- See a typo/mistake?
- Have a story/tip?
This has been shared 0 times

Featured Flyer
Dr. Roach: Hip may be causing pain after surgery, not the replaced knee
Dear Dr. Roach: I read your recent column about a person who had knee pain after a knee replacement. I am a retired orthopedic surgeon who performed on over 10,000 total joints of the hip, knee and shoulder in my 47 years of active surgical practice. A well-done total knee replacement does not give the patient much pain postoperatively. I saw many patients who had this story in my career, and the first thing that comes to mind is that the patient was having referred pain to the knee from an arthritic hip joint.
Oftentimes, the surgeon who performed a painful knee replacement never X-rayed the hip or did a complete exam to look for a limited range of motion in the hip. The patient who has knee pain after a total knee replacement needs to have an examination and X-ray of the hip.
Also: Steatotic liver disease can be treated with weight loss, exercise
I saw more than a few patients who had surgery on their knee when it was their arthritic hip causing referred knee pain that was the real diagnosis. In this case, performing a total hip replacement may eliminate the pain completely. Qualified orthopedic surgeons will agree with me in this case. My advice to inexperienced surgeons is: “Always check the hip before jumping into a total knee replacement!”
— Gary Wolfgang, M.D., Retired Orthopedic Surgeon
Dear Gary Wolfgang, M.D.,: I thank Dr. Wolfgang for writing and for the important reminder of the close connection between the knee and hip. It isn’t that the knee doesn’t have any problems; it’s that there may be more than one cause for knee pain, and I have certainly seen, as Dr. Wolfgang has, many patients with knee pain whose pain was actually due to a hip problem. So, replacing the knee won’t help the hip, which is the underlying cause of the pain.
Dear Dr. Roach: I have just had my prostate gland surgically removed three weeks ago, and I am experiencing incontinence because of the surgery. I am worried that if I drink my usual amount of 8 glasses of water a day, like I did in the past, I will be inside the bathroom more than I am outside of it.
What is your opinion on this issue of not drinking enough water because of my fear of bathroom trips? Do you think I should just keep drinking water and not care about the trips to the bathrooms?
Dear M.G.: Some degree of incontinence is extremely common after surgery for prostate cancer. But you will be glad to hear that over time, most men regain much better control over their bladder function. The rates of complete continence are much higher one month after surgery compared to one week, and the rates continue to improve months or even years after surgery. The use of pelvic floor muscle training also speeds up the recovery of bladder control.
In the short-term, you absolutely need to stay well-hydrated, especially after surgery, but this doesn’t mean you need to force down fluids. Most people don’t need 8 glasses a day; 4 is enough. Thirst remains an excellent guide of whether you need fluids or not.
Readers may email questions to [email protected].

IMAGES
VIDEO
COMMENTS
Remember, after hip replacement surgery, the journey to recovery is a marathon, not a sprint, and with the right exercises, you'll reach your milestones confidently and safely. Neglecting Overall Health: A Top Mistake After Surgery.
At first, you'll use a walker and then a cane for balance. According to the AAOS, you can start off walking 5 to 10 minutes at a time, 3 or 4 times a day. Then, as your strength improves, you ...
Request an Appointment. 410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. Find a Doctor. A Johns Hopkins expert answers common questions about recovery and rehabilitation, downtime after the surgery, and warning signs of potential complications.
The First Week After Hip Replacement and Infection Prevention. Yet another key safety concern in the hip replacement recovery period is infection of the surgical site or implant. While implant infection is a very low risk factor, it can occur in an extremely small percentage of cases and every patient should watch for them.
The first few days after hip replacement surgery are crucial for initiating recovery and setting the stage for a smooth journey. Here's what you can expect during this initial phase: Hospital Stay: Pain Management: Your primary concern will likely be pain management. The hospital staff will provide medication to keep you comfortable, and they ...
Beyond 2-3 months. After 2-3 months of partial or total hip replacement, a person may be able to resume daily activities but should continue with daily physical therapy and regular walking. As ...
During hip replacement, a surgeon removes the damaged sections of the hip joint and replaces them with parts usually constructed of metal, ceramic and very hard plastic. This artificial joint (prosthesis) helps reduce pain and improve function. Also called total hip arthroplasty, hip replacement surgery might be an option if hip pain interferes ...
Let's delve deeper into the details to make your total hip replacement recovery journey smoother. What To Expect After Hip Replacement Surgery. After your surgery, you'll wake up in a recovery room and be monitored for any immediate post-operative complications. Pain management is a priority, and you'll be given medications to alleviate ...
Exercises for After Hip Replacement in the Greater Jacksonville Area. Healing after hip replacement surgery is a process that requires time, patience, and commitment. Incorporating safe and effective exercises into your daily routine can significantly improve your recovery journey, leading to enhanced mobility and a better quality of life.
After a hip replacement surgery, the journey to full recovery truly begins, and physical therapy plays a starring role in this process. At Avid Sports Medicine, we believe that a well-structured physical therapy program is crucial for a successful recovery. Here's how physical therapy can make a difference in your post-surgery life.
Hip Flexor Stretch. Kneel on one knee with the other foot in front, forming a 90-degree angle. Gently push your hips forward, feeling a stretch in the front of the hip of the kneeling leg. Hold for 15-30 seconds and switch legs. This stretch targets the hip flexors.
One-to-three days after a hip replacement. The initial recovery phase typically takes place in hospital. The average hospital stay following hip replacement ranges from one to three days. During this time, pain management, monitoring, and physiotherapy are provided to help you regain strength and mobility. If you have a hip replacement at a ...
Here are some tips to help manage pain and swelling during this period: Movement is key. The more you move, the less the hip and muscles stiffen up. Rest between therapy sessions. Ice the leg and the incision site. Take anti-inflammatory medications (after consulting with your doctor) 3.
After undergoing hip replacement surgery, it is crucial to prepare yourself for the journey of recovery. This phase is essential for regaining mobility and ensuring a successful outcome. By understanding the recovery process, setting realistic expectations, and making necessary preparations, you can make your post-surgery experience more ...
The role of confidence during the journey through hip replacement. Confidence, ... surgery 252 and can help to predict outcomes. 253 We also know that realisation of patients' pre-operative expectations after hip and knee replacement surgery are significant in influencing their reported outcomes and satisfaction. 145, 165, 254 This body of ...
Dressing After Hip Replacement: The Basics. Before we dive into the step-by-step dressing guide, let's start with some basic considerations for dressing after your hip replacement: 1. Choose the Right Clothing: Your choice of clothing is pivotal in ensuring a smooth dressing process. Opt for garments that are easy to put on and take off.
The Journey of Recovery After Hip Replacement Recovering from hip replacement surgery is a unique journey for each person. Regaining strength and suppleness in the hip muscles is an integral part of recuperation after a hip replacement, so that one can get back to their usual activities - such as running.
The journey to full recovery would take time, and I had to be patient. ... Thank you so much for sharing your journey. I can't wait to read your Life after hip replacement entry. I'm 45 and have been struggling with hip pain and walking "ugly" for a few years or even longer. I can't remember I just dealt with it.
The Journey to Running After Hip Replacement. Although his knee problems were cured and he went back to running, Tom's right hip started to give him pain about five years ago. He learned he had arthritis and that he would eventually need surgery when it became too painful.
There are three resources to help you prepare and then recover from your hip replacement surgery. The first is an education class presentation which will guide you through the entire journey and is a MUST WATCH. To support this there is the 'Your Personal Guide to Hip Replacement Surgery' booklet. Lastly, there are also bite-size video ...
If you are planning to travel after your joint replacement, please discuss this with your surgeon before your surgery so you can both work together in developing a customized plan for a safe journey. ... Pinsorsnak P, Amstutz HC, Schmalzried TP. Extended travel after hip arthroplasty surgery. Is it safe? J Arthroplasty 22(6 Suppl 2): 29, 2007;
From left: X-rays of McCann's before and after hip replacement surgery. Photo courtesy PBT. ... I talk about my journey in several episodes of my podcast, Two Women Two Worlds, with former dancer Tilda Karine (available on Apple Podcasts and Spotify). On my Instagram page ...
DEAR DR. ROACH: I read your recent column about a person who had knee pain after a knee replacement. I am a retired orthopedic surgeon who performed on over 10,000 total joints of the hip, knee ...
Q: I read your recent column about a person who had knee pain after a knee replacement. I am a retired orthopedic surgeon who performed on over 10,000 total joints of the hip, knee and shoulder in ...
DEAR DR. ROACH: I read your recent column about a person who had knee pain after a knee replacement. I am a retired orthopedic surgeon who performed on over 10,000 total joints of the hip, knee ...
Dear Dr. Roach: I read your recent column about a person who had knee pain after a knee replacement. I am a retired orthopedic surgeon who performed on over 10,000 total joints of the hip, knee ...
Joe Lieberman, the first Jewish vice-presidential nominee of a major party, whose conscience and independent streak later led him on a journey away from his home in the Democratic Party, has died ...
Dear Dr. Roach: I read your recent column about a person who had knee pain after a knee replacement.I am a retired orthopedic surgeon who performed on over 10,000 total joints of the hip, knee and ...