
Mon - Fri 9am - 8pm
Sat 9am - 4pm
Sun 10am - 4pm
- 0800 294 2969
- Single Trip Travel Insurance
- Annual Travel Insurance
- Cruise Travel Insurance
- Family Travel Insurance
- Staycations
- Winter Sports
- Coronavirus
- Business Travel Insurance
- School Trip Travel Insurance
- All No Upper Age Limit Travel Insurance >
- Car Insurance
- Home Insurance
- Smart Luggage
- Life Insurance

Specialist Travel Insurance with no upper age limit
- Angioplasty
- Atrial Fibrillation
- Cardiomyopathy
- High Blood Pressure
- Multiple Sclerosis
- Breast Cancer
- Skin Cancer
- Lung Cancer
- Prostate Cancer
- Crohn’s Disease
- Back Problems
- Osteoporosis
- South Africa
- All Africa Insurance >
- All Asia Insurance >
- The Dominican Republic
- All Caribbean Insurance >
- All Central America Insurance >
- All Europe Insurance >
- Puerto Rico
- All North America Insurance >
- New Zealand
- All Oceania Insurance >
- All South America Insurance >
- Get a Quote
- Airport Hotels & Parking
- Travel Money
- Travel Advice
- Working with Us
- Medical Advice Hub
- Brand Showcase
- Meet The Team
- Careers: Apprenticeship Scheme
- Amend your policy
- Your Questions Answered
- Make A Complaint
- Making a Claim
Home > Latest News > Essential Guide to Travelling with High Blood Pressure
Essential Guide to Travelling with High Blood Pressure
by Phil Day | Feb 4, 2021 | Guides | 0 comments

by Phil Day
4 February 2021
An essential guide to travelling with High Blood Pressure By Phil Day, Superintendent Pharmacist – Pharmacy2U
Blood pressure is the measurement of the pressure of the blood pressing against the walls of your arteries, as it travels away from the heart. It’s one of the 4 vital signs which are monitored by medical professionals (including body temperature, pulse rate and respiratory rate) and there can be serious implications if it’s too high (hypertension).
In this article I’m going to explore high blood pressure , how it can be managed and how to be prepared when travelling.
What is high blood pressure (hypertension)?
If you have a reading of 140/90mmHg or above, this is considered to be high blood pressure.
However if you’re 80 or older, then it’s considered to be high if it’s over 150/90mmHg.
What are the symptoms of high blood pressure?
The symptoms of high blood pressure are rarely noticeable, which means you could be living with it without knowing.
The only way to tell if you have high blood pressure is by having it measured.
When your blood pressure is high, it puts an extra strain in your heart, blood vessels, and other organs in your body. Left untreated, it can lead to potentially life-threatening conditions such as heart disease, heart failure, strokes, kidney disease, aortic aneurysms , and others.
What causes high blood pressure?
The causes of high blood pressure are not always clear, but there are several factors that increase the risk, including:
- Not exercising enough
- Drinking too much alcohol, coffee or other caffeine-based drinks
- Eating too much salt and too few fruits and vegetables
- Not getting enough sleep, or having poor quality sleep
- Having a relative with high blood pressure
- Aged over 65
- Being of black African or black Caribbean descent
How is high blood pressure treated?
High blood pressure can usually be successfully managed , although the recommended treatment may vary from person to person.
Lowering a raised blood pressure reduces risk of developing a more serious health condition later.
By making changes to your lifestyle, it’s possible to reach and maintain a normal blood pressure.
Changes you could make include:
- Stopping smoking
- Exercising regularly
- Cutting back on alcohol
- Drinking fewer caffeinated drinks
- Losing weight, if you’re overweight
There are also medicines which can be prescribed to help keep your blood pressure under control.
Many people will need to take a combination of different medicines and the medicines you are prescribed may vary depending on age and ethnicity.
If you’re under 55 years old you’ll usually be offered or an angiotensin-2 receptor blocker (ARB), or an ACE inhibitor. If you’re 55 years old or older or of African or Caribbean origin then you’ll usually be offered a medicine called a calcium channel blocker.
It’s important to take any medicines prescribed exactly as agreed with your doctor.
When you’re taking medicine to treat high blood pressure, you will probably not feel any different – but this doesn’t mean it’s not working or that it’s not important for you to take it every day.
It’s lowering your risk of worsening health in the future.
Can I travel with high blood pressure?
Having high blood pressure shouldn’t be a barrier to travelling, but it is always a good idea to check with your GP before making any travel plans. If you’re wondering, ‘Can you fly with high blood pressure?’ the answer is yes. For those concerned about high blood pressure flying, If your high blood pressure is well controlled with medication, then flying with high blood pressure should be perfectly fine, as long as you take the right precautions. It’s important to note that there isn’t a legally imposed blood pressure limit for flying, but maintaining control over your blood pressure is crucial for safe air travel.
Tips for travelling with high blood pressure:
- Choose Travel Insurance that covers pre-existing medical conditions and make sure you declare High Blood Pressure if you have been diagnosed with it. That means it will cover any high blood pressure related medical costs if you need treatment while on holiday.
- Pack your medication in your hand luggage so that you have easy access to it and minimise the risk of your medication getting lost in your suitcase. It is a good idea to take extra medication with you just in case you lose any or end up being delayed.
- You should also take your prescription with you, as this will help in the event that you need to get more medication while you are away.
- It is best to take your own food to take on the plane with you as airline food can sometimes have high levels of salt which can increase your blood pressure levels.
- If you have a trip planned full of adrenaline-filled activities, check them with your GP just to make sure they are happy for you to take part (and mention to your Insurance provider)
- If you are travelling to a different time zone you may want to adjust the time you take your medication accordingly. However, if you want to keep taking it at the same time you do at home, for example with breakfast, this is also fine to do. Just make sure you are taking the medicine as prescribed and not taking more than the recommended dose.
How to get your high blood pressure medication from Pharmacy2U
If you have an NHS repeat prescription for high blood pressure, then Pharmacy2U can help. Our UK-based team of pharmacists can help you cut out unnecessary trips to the GP or pharmacist by delivering the medication you need to your door . Our simple service lets you order your prescription from anywhere and registration is quick and simple.
For more information and support about high blood pressure , talk to your GP or pharmacist.
Visit Pharmacy2U’s website >
Travel Insurance for High Blood Pressure
Get a quote today and ensure you declare any pre-existing medical conditions, including High Blood Pressure.

How Just Travel Cover helped me see the world…
May 15, 2024 | Blogs
We caught up with Mrs Norton, who took out her 30th policy with Just Travel Cover this year, ahead of a five week round-the-world-World Cruise....

Travellers risk ‘financial ruin’ without Travel Insurance, say ABTA
May 1, 2024 | Blogs
ABTA says big increase in medical costs abroad makes Travel Insurance even more essential. The travel association has warned travellers that ...

Travel Insurance Checklist – Everything you need to know
Mar 20, 2024 | Blogs
We know that Travel Insurance can be complex especially for those who have pre-existing medical conditions, so we have pulled together our go-to...
Compare prices in minutes

Copyright © 2023. Just Travel Cover
- Travel Tips Advice
- Compare Travel Insurance
- Pre-Existing Medical Conditions
- Holiday Home Insurance
Customer Services
- Opening Times
Victoria House, Toward Road, Sunderland, SR1 2QF
Call: 0800 294 2969
Monday - Thursday 9am - 6pm, Friday 9am - 5.30pm
Buy with Confidence
Secure Payments
UK Call Centre
Leading Broker
Justtravelcover.com is a trading style of Just Insurance Agents Limited, which is authorised and regulated by the Financial Conduct Authority (FCA) number 610022 for General Insurance Distribution activities. Registered in England. Company No 05399196, Victoria House, Toward Road, Sunderland SR1 2QF. Our services are covered by the Financial Ombudsman Service. If you cannot settle a complaint with us, eligible complainants may be entitled to refer it to the Financial Ombudsman Service for an independent assessment. The FOS Consumer Helpline is on 0800 023 4567 and their address is: Financial Ombudsman Service, Exchange Tower, London E14 9SR. Website: www.financial-ombudsman.org.uk/
Privacy Overview
Can You Fly With High Blood Pressure? What You Need To Know

Traveling is a fantastic way to escape the daily routine, experience new cultures, and create unforgettable memories. However, traveling can be challenging if you have certain health conditions, such as:
- High blood pressure
- Asthma & allergies
However, living with health conditions shouldn’t stop you from exploring the world. With adequate preparation and the right precautions, you can have a safe and enjoyable trip.
In today’s post, we’ll share everything you need to know about traveling with high blood pressure, including:
- What hypertension is
- Risks of traveling with high blood pressure
- What to consider when planning your trip
- Some tips on high blood pressure and flying
Without further ado, let’s begin.
What is Hypertension? (aka High Blood Pressure)
For most people, hypertension is defined as a blood pressure reading over 140/90 mm Hg. According to WHO, approximately 1.28 billion adults aged 30 to 79 suffer from hypertension worldwide, and 46% are unaware of it. Besides, only 1 in 5 people (21%) has it under control.
High blood pressure is a leading cause of death or a contributing factor. Sadly, hypertension doesn’t show evident symptoms.
Severe high blood pressure cases (usually 180/120 or higher) may experience the following symptoms:
- Severe headaches
- Difficulty breathing
- Blurred vision
- Abnormal heart rhythm
All in all, high blood pressure is a common condition but it can be serious if it’s not treated. Typically, you can reduce your blood pressure by adopting a healthier lifestyle with practices like:
- Exercising regularly
- Keeping a healthy diet
- Quitting smoking
- Avoiding excessive alcohol and caffeine consumption
- Monitoring blood pressure at home or your local pharmacy
- Reducing stress
- Minimizing salt consumption
Nonetheless, some people may need to take medications.
High Blood Pressure and Flying: What Are The Risks?
Overall, high blood pressure patients who take medication don’t have an increased risk of health problems at higher altitudes. Nevertheless, poorly controlled or severe hypertension does increase this risk.
The effects of occasional flying on heart health are relatively unstudied. Yet, according to a recent study , even men in good health have an increased blood pressure of 6% during commercial flights.
According to the CDC , about 1 in 600 flights experience a medical emergency, such as:
- Heart problems
- Nausea or vomiting
And blood pressure may be a contributing factor to some of these emergencies.
What to Consider When Planning Your Trip
Traveling to high altitudes (5,000 to 11,500 feet) can increase blood pressure. Why? At these heights, your blood works harder to deliver oxygen, causing blood pressure to rise.
Therefore, when planning your trip, you may want to avoid destinations like:
However, if you already booked your trip, don’t panic: managing your blood pressure at high altitudes is possible. Experts recommend:
- Light physical activity
- Avoid climbing more than 300 meters per day
Be extra mindful of these tips when staying in mountainous areas, like the Alps or the Andes.
Overall, traveling at high altitudes shouldn’t be a problem as long as your blood pressure is controlled and you take some precautions. Here are some tips you may want to consider:
- Consult your doctor 8 weeks before your trip to discuss your travel plans.
- Get your medication ready , and make sure to bring enough to cover your whole trip. Besides, bringing a bit extra may be a good idea in case your return flight gets rescheduled.
- Keep your alcohol and caffeine consumption to a minimum during your flight to avoid dehydration.
- Be careful with airline food, it might have high sodium levels , which can raise your blood pressure.
- Taking Dramamine to avoid motion sickness doesn’t interfere with blood pressure medications.
- Avoid using sedative and hypnotic medications before and during flight.
- Promote circulation by moving around during your flight with walks every two hours and by moving in your seat.
Key Takeaways
Ultimately, traveling with high blood pressure doesn’t have to limit your travel plans. With proper planning, taking necessary precautions, and consulting your doctor, you can enjoy your trip confidently and safely.
Remember to:
- Monitor your blood pressure
- Make wise choices regarding food and drink
- Stay active during your journey
Want to get tested for COVID before your next trip? No matter where you are, or what type of test you need, find testing locations near you with our international directory .
Have Travel Questions?
Join our Facebook community full of travelers like you
Recent posts

COVID Testing in San Antonio

Best Foods for COVID Recovery

COVID Testing in Spanish: What to Know and Who to Ask

COVID Pandemic Effects: Social Impact, Mental Health, Worklife, and more
Share this article.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Anatol J Cardiol
- v.25(Suppl 1); 2021

Systemic arterial hypertension and flight
Hypertension is the major preventable cause of cardiovascular disease and all-cause death. Given its overall high prevalence, hypertension would be one of our major concerns in commercial flights. Hence, the management of hypertension is of great importance. Herein, we discuss the pathophysiological factors for elevated blood pressure during flight, and we make recommendations which should be followed by the passengers and the flight crew and the physicians for trouble-free air travel.
Introduction
Conventionally, hypertension is defined as office systolic blood pressure (SBP) values ≥140 mm Hg and/or diastolic blood pressure (DBP) values ≥90 mm Hg or requiring antihypertensive medication ( 1 ). On the basis of office BP, approximately 1.13 billion people were affected by hypertension in 2015, and hypertension is the major preventable cause of cardiovascular disease (CVD) and all-cause death ( 2 ). In the PatenT2 (the prevalence, awareness, treatment, and control of hypertension in Turkey) trial, the overall age and sex-adjusted prevalence of hypertension was found as 30.3% ( 3 ).
Approximately, 40 million people use commercial flights annually ( 4 ). It is estimated that by 2030, half of the passengers in commercial flights will be over 50 years of age because of increased life spans. At the same time, our ability to care for patients with cardiac diseases and advancement in flying technology improve continuously. Accordingly, we can predict a higher number of “older” individuals or those with cardiac diseases will travel in commercial flights ( 5 ). Given its overall prevalence mentioned above, hypertension would be one of our major concerns. The management of hypertension should be considered, both for the passengers and the flight crew.
The main pathophysiological factor during a flight is altitude related decrease in oxygen saturation. Commercial airplanes fly at 30,000–40,000 feet (corresponding to 9,000–12,000 m) above the sea level. However, commercial flights maintain a relative cabin altitude between 5,000 and 8,000 feet during routine flights. However, at this altitude, the barometric pressure decreases from a normal sea level value of 760 to 560 mm Hg. This pressure change is related to the decrease in arterial oxygen tension, which is well tolerated in healthy individuals but might trigger ischemia and arrhythmia in susceptible patients. The inspired PO 2 falls by 4 mm Hg per 1,000 feet above sea level. Consequently, the patients with concomitant pulmonary diseases such as chronic obstructive pulmonary disease and pulmonary hypertension may require supplemental oxygen during travel. In addition, some patients with cardiovascular diseases such as severe left and/or right ventricular dysfunction and congenital heart diseases can be more sensitive to changes in arterial oxygen saturation ( 4 , 6 , 7 ). The details of acute and chronic cardiovascular changes for adaption to high altitude will not be mentioned in detail. Basically, an increase in heart rate, cardiac contractility, and cardiac output could alter systemic blood pressure. Hypoxia triggers peripheral vasodilatation and activation of the sympathetic nervous system. In patients with hypertension, however, endothelial dysfunction may inhibit hypoxic vasodilatation and even induce peripheral vasoconstriction. In healthy individuals, these mechanisms overall result in a non-significant increase of blood pressure, but with high inter-individual variability. Only a modest increase was observed in patients with controlled blood pressure ( 8 – 10 ). However, there is still a potential risk for significant elevation in systemic arterial pressure in those with uncontrolled blood pressure. Stressful factors related to flight such as increased anxiety especially during take-off and landing, changes in body position induced by acceleration and deceleration, and aircraft noise have been shown to negatively affect the mood state of the crew ( 11 ). These factors should be regarded as confounders for changes in blood pressure, both in passengers and flight crew.
Unfortunately, most data regarding changes in cardiac responses during flight were derived either from retrospective studies or small observational trials. In a recent study ( 12 ), 12 men without any known cardiac disease or coronary risk factors were monitored in commercial flights. A decrease in arterial oxygen saturation was observed during the flight when compared with baseline, with the lowest saturation recorded at 120 minutes in cruise altitude. The heart rates were similar at different times of the flight, and the maximum SBP and DBP values were recorded at the time of takeoff. The lowest SBP and DBP values were measured at cruise altitude. Oliveira-Silva et al. ( 13 ) have monitored 22 physically active men, free from pathological conditions and medications during commercial flights. They reported 24% elevated heart rate, 6% increase in blood pressure, and reduced parameters of heart rate variability.
Furthermore, important cardiovascular responses are less understood and reported during spaceflights. Norsk et al. ( 14 ) have observed male astronauts and demonstrated that weightlessness in space initially induced an increase in stroke volume and cardiac output by 35%–41% between 3 and 6 months, accompanied by unchanged or slightly reduced blood pressure by 8–10 mm Hg mainly owing to decrease in systemic vascular resistance.
Despite differences in the civil aviation authority rules among countries, some cardiovascular conditions are generally accepted to be a contraindication for air travel ( 7 , 8 , 15 , 16 ). Some examples are unstable chest pain, recent myocardial infarction, or cerebrovascular event (within the previous 2 weeks), decompensated heart failure, poorly controlled arrhythmias, uncontrolled hypertension, or pregnancy with preeclampsia. There is no cut-off blood pressure value for “uncontrolled hypertension.” However, patients with a value of greater than 180/120 mm Hg as well as those with dizziness, chest pain, confusion, severe headache, and visual problems must seek specific care. General recommendations for air travelers with hypertension are listed in Table 1 . Apart from air travelers, the flight crew, particularly pilots with elevated blood pressure. Should be evaluated and managed carefully according to the instructions from the national civil aviation authorities. Overall, pilots with well-controlled hypertension (central acting agents such as reserpine and methyldopa are prohibited) and without any end-organ damage are not suspended from flying ( 16 ).
General recommendations for air travelers with hypertension ( 7 , 8 , 16 , 17)
The number of air travelers with cardiac diseases is continuing to increase. All passengers with cardiovascular disease should take tailored advice based on their current status. High-altitude exposure is well tolerated by the hypertensive except for those with uncontrolled blood pressure levels and/or with accompanying serious cardiovascular problems. These patients must seek specific advice from their physician. General recommendations should be followed by the passengers and the flight crew for trouble-free air travel.
Conflict of interest: None declared.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Guidelines for Flying With Heart Disease
Air travel is generally safe for heart patients, with appropriate precautions
- Pre-Flight Evaluation
Planning and Prevention
During your flight.
If you have heart disease, you can fly safely as a passenger on an airplane, but you need to be aware of your risks and take necessary precautions.
Heart conditions that can lead to health emergencies when flying include coronary artery disease (CAD) , cardiac arrhythmia (irregular heart rate), recent heart surgery, an implanted heart device, heart failure , and pulmonary arterial disease.
When planning air travel, anxiety about the prevention and treatment of a heart attack on a plane or worrying about questions such as "can flying cause heart attacks" may give you the jitters. You can shrink your concern about things like fear of having a heart attack after flying by planning ahead.
Air travel does not pose major risks to most people with heart disease. But there are some aspects of flying that can be problematic when you have certain heart conditions.
When you have heart disease, air flight can lead to problems due to the confined space, low oxygen concentration, dehydration, air pressure, high altitude, and the potential for increased stress. Keep in mind some of these issues compound each other's effects on your health.
Confined Space
The prolonged lack of physical movement and dehydration on an airplane may increase your risk of blood clots, including deep vein thrombosis (DVT) or pulmonary embolism (PE) . One of the biggest risks for people with heart disease who are flying is developing venous thrombosis.
These risks are higher if you have CAD or an implanted heart device, such as an artificial heart valve or a coronary stent. And if you have an arrhythmia, a blood clot in your heart can lead to a stroke.
One of the biggest risks for people with heart disease who are flying is developing an arterial blood clot or venous thrombosis.
Low Oxygen and Air Pressure
The partial pressure of oxygen is slightly lower at high altitudes than at ground level. And, while this discrepancy on an airplane is typically inconsequential, the reduced oxygen pressure in airplane cabins can lead to less-than-optimal oxygen concentration in your body if you have heart disease.
This exacerbates the effects of pre-existing heart diseases such as CAD and pulmonary hypertension .
The changes in gas pressure in an airplane cabin can translate to changes in gas volume in the body. For some people, airplane cabin pressure causes air expansion in the lungs. This can lead to serious lung or heart damage if you are recovering from recent heart surgery.
Dehydration
Dehydration due to cabin pressure at high altitude can affect your blood pressure, causing exacerbation of heart disease. This is especially problematic if you have heart failure, CAD, or an arrhythmia.
If you experience stress due to generalized anxiety about traveling or sudden turbulence on your flight, you could have an exacerbation of your hypertension or CAD.
Pre-Flight Health Evaluation
Before you fly, talk to your healthcare provider about whether you need any pre-flight tests or medication adjustments. If your heart disease is stable and well-controlled, it is considered safe for you to travel on an airplane.
But, if you're very concerned about your health due to recent symptoms, it might be better for you to confirm that it's safe with your healthcare provider first before you book a ticket that you may have to cancel.
Indications that your heart condition is unstable include:
- Heart surgery within three months
- Chest pain or a heart attack within three months
- A stroke within six months
- Uncontrolled hypertension
- Very low blood pressure
- An irregular heart rhythm that isn't controlled
If you've had a recent heart attack, a cardiologist may suggest a stress test prior to flying.
Your healthcare provider might also check your oxygen blood saturation. Heart disease with lower than 91% O2 saturation may be associated with an increased risk of flying.
Unstable heart disease is associated with a higher risk of adverse events due to flying, and you may need to avoid flying, at least temporarily, until your condition is well controlled.
People with pacemakers or implantable defibrillators can fly safely.
As you plan your flight, you need to make sure that you do so with your heart condition in mind so you can pre-emptively minimize problems.
While it's safe for you to fly with a pacemaker or defibrillator, security equipment might interfere with your device function. Ask your healthcare provider or check with the manufacturer to see if it's safe for you to go through security.
If you need to carry any liquid medications or supplemental oxygen through security, ask your healthcare provider or pharmacist for a document explaining that you need to carry it on the plane with you.
Carry a copy of your medication list, allergies, your healthcare providers' contact information, and family members' contact information in case you have a health emergency.
To avoid unnecessary anxiety, get to the airport in plenty of time to avoid stressful rushing.
As you plan your time in-flight, be sure to take the following steps:
- Request an aisle seat if you tend to need to make frequent trips to the bathroom (a common effect of congestive heart failure ) and so you can get up and walk around periodically.
- Make sure you pack all your prescriptions within reach so you won't miss any of your scheduled doses, even if there's a delay in your flight or connections.
- Consider wearing compression socks, especially on a long trip, to help prevent blood clots in your legs.
If you have been cleared by your healthcare provider to fly, rest assured that you are at very low risk of developing a problem. You can relax and do whatever you like to do on flights—snack, read, rest, or enjoy entertainment or games.
Stay hydrated and avoid excessive alcohol and caffeine, which are both dehydrating. And, if possible, get up and walk for a few minutes every two hours on a long flight, or do leg exercises, such as pumping your calves up and down, to prevent DVT.
If you develop any concerning issues while flying, let your flight attendant know right away.
People with heart disease are at higher risk for developing severe complications from COVID-19, so it's especially important for those with heart disease to wear a mask and practice social distancing while traveling.
Warning Signs
Complications can manifest with a variety of symptoms. Many of these might not turn out to be dangerous, but getting prompt medical attention can prevent serious consequences.
Symptoms to watch for:
- Lightheadedness
- Dyspnea (shortness of breath)
- Angina (chest pain)
- Palpitations (rapid heart rate)
- Tachypnea (rapid breathing)
To prepare for health emergencies, the U.S. Federal Aviation Administration mandates that supplemental oxygen and an automated external defibrillator (AED) is on board for passenger airplanes that carry 30 passengers or more. Flight crews receive training in the management of in-flight medical emergencies and there are protocols in place for flight diversions if necessary.
A Word From Verywell
For most people who have heart disease , it is possible to fly safely as long as precautions are taken. Only 8% percent of medical emergencies in the air are cardiac events, but cardiac events are the most common in-flight medical cause of death.
This means that you don't need to avoid air travel if you have stable heart disease, but you do need to take precautions and be aware of warning signs so you can get prompt attention if you start to develop any trouble.
Hammadah M, Kindya BR, Allard‐Ratick MP, et al. Navigating air travel and cardiovascular concerns: Is the sky the limit? Clinical Cardiology . 2017;40(9):660-666. doi:10.1002/clc.22741.
Greenleaf JE, Rehrer NJ, Mohler SR, Quach DT, Evans DG. Airline chair-rest deconditioning: induction of immobilisation thromboemboli? . Sports Med. 2004;34(11):705-25.doi:10.2165/00007256-200434110-00002
American Heart Association. Travel and heart disease .
Ruskin KJ, Hernandez KA, Barash PG. Management of in-flight medical emergencies . Anesthesiology. 2008;108(4):749-55.doi:10.1097/ALN.0b013e31816725bc
Naqvi N, Doughty VL, Starling L, et al. Hypoxic challenge testing (fitness to fly) in children with complex congenital heart disease . Heart. 2018;104(16):1333-1338.doi:10.1136/heartjnl-2017-312753
By Richard N. Fogoros, MD Richard N. Fogoros, MD, is a retired professor of medicine and board-certified in internal medicine, clinical cardiology, and clinical electrophysiology.
Telephone Hours
Opening Hours
- Mon-Fri: 8:30am - 8pm
- Sat: 9am - 5:30pm
- Sun: 10am - 5pm
Bank Holiday Opening Hours:
- 6th May: 9am-5pm
- 27th May: 9am-5pm
- Mon-Fri: 9:00am - 8:00pm
- Sat: 9:00am - 5:30pm
- Sun: 10:00am - 5:00pm
Flying with High Blood Pressure
Can I fly with high blood pressure? Read this guide for up-to-date information and top tips for travelling with high-pressure.
Page contents
Can you fly with high blood pressure.
Millions of people fly safely with high blood pressure every year. However, there are things you should check before travelling – talk to your doctor, take your medication and travel with a blood pressure monitor – to help avoid any issues.

Before travelling with high blood pressure
Before you fly, consider visiting your doctor to discuss your travel plans – particularly if your blood pressure is unstable.
They will determine whether or not you should fly. This of course is an important consideration for your health, but also for your Travel Insurance – as you will need to be determined fit to travel for your policy to be valid.
If your doctor deems it unsafe for you to fly, they still may be able to recommend a better time for you to travel or for you to change your travel plans slightly.
Travel Insurance
You must remember to declare your high blood pressure as a pre-existing medical condition. There are many complications of high blood pressure – such as a blood clot – which you may not associate with the condition but that you won’t be covered for unless you declare high blood pressure. You’ll need cover from a specialist medical Travel Insurance provider .
Benefits of AllClear Cover
Simple 3 step quote process, 1. call us or click a quote button on our site, 2. complete our simple medical screening process, 3. get your quotes.
High blood pressure is often a condition that people don’t bother to declare, says Dr Harikrishna Patel from AllClear: “It’s often something which people get used to living with and don’t give a second thought to.”
But this is not necessarily the case: “Travelling invariably means a disruption to routine and possibly a change in time zone, so tablets may be delayed or missed altogether. Heat, physical exertion, change in diet or a tummy upset can all have an impact.
So what might be a stable medical condition at home could potentially be a problem abroad that results in a medical emergency claim.”
- If you’re taking blood pressure medication and your journey will involve you being away from home for more than a couple of weeks, make sure you have enough medication to last the duration of your trip, including extras in case of emergency.
- Consider also the time zone of your destination, as you may need to take your medication at a different time to normal.
- If you will need to take medication during your flight, be sure to speak with your airline to confirm it’s allowed in your carry-on bag.
- Bring a copy of your prescription and a letter from your doctor explaining your condition and treatment.
Blood Pressure Checker
If your blood pressure is unstable, it’s well worth investing in a good blood pressure monitor. That way you can keep an eye on your blood pressure while you’re on holiday, and ensure that it remains within a safe range.
High blood pressure is considered a level consistently at or above 140mmHg and/or 90mmHg .
Before you travel
Check the local weather and time zone of your destination and plan accordingly. Avoid travelling to places that are very hot, cold, or high in altitude, as they may affect your blood pressure.
Reduce stress
Take time to minimise the level of stress you are exposed to. This can be through simple things, like making sure you’re up to date with the latest travel updates from the FCDO before you travel or packing a few days in advance so you know you have everything you need.
You can also practice some relaxation techniques, such as deep breathing, meditation, or listening to soothing music.
During the flight
If you have high blood pressure, there are a few things you can do while flying which may help.
Eating and drinking
Stay hydrated and avoid alcohol, caffeine, and salty foods. These can dehydrate you and raise your blood pressure. Drink plenty of water and eat fresh fruits and vegetables instead.
Staying active
Walking around the plane as regularly as possible can aid circulation and reduce the risk of DVT . Gentle leg exercises from your seat can also help ensure you keep circulation moving throughout the flight. This activity helps reduce the risk of any blood clots, and you can also buy flight socks to help in this regard.
After you travel
Check your blood pressure again when you return home and compare it with your previous readings. If you notice any significant changes or symptoms, contact your doctor or seek medical attention immediately.
Resume your normal medication schedule and lifestyle as soon as possible. If you have made any adjustments to your medication or dosage while travelling, consult your doctor before changing them back. Also, try to maintain a healthy diet, exercise regularly, and manage your stress levels to keep your blood pressure under control.
The information in this blog post is not intended to replace professional medical advice. It is a general overview of a broad medical care topic. Blog posts are not tailored to one person’s specific medical requirements, diagnosis or treatment. If you do notice symptoms or you require medical advice, you should always consult your doctor or healthcare provider to obtain professional medical help. Read through our disclaimer for more information.
Written by Lydia Crispin , MA Content Creator at AllClear Edited by Letitia Smith , M.Sc. Content Manager at AllClear
Written by: Lydia Crispin | Travel Insurance Expert Last Updated: 23 August 2023
† Based on Trustpilot reviews of all companies in the Travel Insurance Company category that have over 70,000 reviews as of January 2024. AllClear Gold Plus achieved a Which? Best Buy.
Policy Wordings
Modern Slavery Statement
MaPS Travel Insurance Directory
Earn rewards by sharing with friends

Travelling with high blood pressure

- 1 Get in/Get around
- 4.1 Sodium intake
- 4.2 Sugar intake
- 4.3 Conclusion
- 7 Stay safe
Every year, millions of people with high blood pressure travel for business, leisure and family functions. People with high blood pressure deal with all the issues other travelers contend with, but also others unique to their situations. In order to have as safe, comfortable and enjoyable a trip as possible, these challenges need to be addressed.
Get in/Get around [ edit ]

If you need to travel by plane, there are special issues you must deal with if you have high blood pressure. First, you must not count on being served low-salt food on the plane, though on many flights, you might be fed a meal or snack that includes an undressed salad or crudités. But while bringing your own food onto the plane is a good idea for anyone, it's particularly important if you are on a low-salt diet. Either cook some low-salt food yourself and pack it or purchase some low-salt snack, such as fresh fruit or vegetables , hard boiled eggs or unsalted chips.
Second, many people experience ear or sinus pain, due to the change in air pressure when ascending and especially on descending. People without high blood pressure have a choice of various decongestants to use, but the most widely available decongestants all risk raising your blood pressure. However, fortunately, saline nose drops are sold in health food and drugstores, you may find them just as effective as a drug like Afrin in preventing pain from pressurization, and unless nasty additives are put into the formula (read the ingredients list), you are very unlikely to suffer any negative side effects from using them at will.
Third, everyone should get up and walk around a plane during a long flight, if possible, but this is particularly recommended for people with high blood pressure.
A fourth consideration involves where you should plan to travel, if you have the choice. This is particularly true if you also have a heart condition in addition to high blood pressure, as you may want to avoid destinations with very hot or cold weather or at high altitudes , lest you strain your heart. In addition, cold weather in particular can be dangerous for people with hypertension , so while the Wikivoyage article on cold weather can be a useful general reference, be sure to check with a trusted physician before you plan that winter vacation to the Arctic, and if you do need to get around in cold weather, bundle up appropriately and consider limiting your time outdoors.
Do [ edit ]

Depending on how well-controlled your blood pressure is and your general level of fitness, many activities may be perfectly safe and may be beneficial for you. This likely includes walking and hiking , but it is always best to check with your personal physician or cardiologist before you go, particularly if you have any doubts. Although certain kinds of exercise can increase blood pressure while you're doing them, regular exercise may lower blood pressure over time, and increasing your fitness level — carefully — is an excellent idea. If you plan to have an active trip, it's particularly important for you to attend to your fitness level with a program of exercise before you go. Exercise can mean walking, swimming or cycling and doesn't have to feel like an extremely rigorous workout (or start out as one).
Be sure to check the level of difficulty before you set out on an activity. You do not want it to come as a surprise that the last five kilometers of an otherwise easy hike are steeply uphill. Somebody not used to people with your condition might forget such "details". On guided physical activities, consider choosing a guide who understands your condition.
If you want to try activities that may put stresses on your body that it is not accustomed to, consult your doctor first. Articles here such as scuba diving , marathon race and altitude sickness have some basic information but only superficially address prior medical conditions.
Buy [ edit ]

First, make sure to buy the medications you need before you go. Should you be traveling for longer than the usual period for a refill of your prescriptions, ask your pharmacy for a vacation supply. If you are traveling for longer than they can supply you and you will be in a foreign country when you will need a refill, find out before you go what you will need to do to get more meds. In some places, a pharmacist may be able to prescribe a new supply for you without an appointment, whereas in others, you will have to make an appointment and be examined by a doctor in order to get a prescription, and it might be expensive and time-consuming to do all of this.
Second, if you have any reason to believe your blood pressure is not well-controlled, you should buy a good digital blood pressure monitor. Bring it into your doctor's office and test its readings for accuracy against the ones they get with their own professional equipment. In order to save yourself from needless worry, if your arms have a large circumference, make sure you get a monitor with an adjustable cuff that is described as being suitable for people with large arms, even though it may cost more (monitors with overly small cuffs are likely to give you inaccurately high blood pressure readings). When you travel, make sure your monitor has live batteries, and bring additional batteries with you.
Third, particularly if you are going to a country where emergency medical care and hospital stays may be very expensive and not covered by the policy that covers your health care at home, consider buying travel insurance , because you don't want to be faced with an unpayable debt of tens of thousands of dollars for a sudden heart attack or cerebral hemorrhage while on vacation. When buying travel insurance it is very important to tell the insurer about your medical condition(s); otherwise, they will send you a quote from the small print rather than money for the hospital bill. Insurance included with package holidays or bank accounts is unlikely to be sufficient.
Eat [ edit ]

Sodium intake [ edit ]
Especially if your blood pressure is not well-controlled, it may be crucial for you to eat a very low-sodium diet. A figure often mentioned as the upper limit for daily sodium intake is 2-2.4 grams — for example, the U.S. Food and Drug Administration recommends that "the general population consume no more than 2,300 milligrams of sodium a day", about a teaspoon of salt. But remember that sodium occurs naturally in many foods as well, so total sodium intake is more than just the amount of salt added, and some people need to limit themselves to far less than 2.3 grams of sodium per day, so be sure to get individual advice.
The best way to ensure a low-sodium diet is to know exactly what you are eating, by having and using your own cooking facilities and otherwise eating items like fresh fruit and vegetables and packaged goods that you have carefully checked for sodium amounts (yogurt is frequently a good low-sodium source of nutrition). Restaurants typically use a lot of salt, even if you cannot taste it. Restaurant-made soups, salad dressings and sauces should all be assumed by default to have a lot of salt, and you should also be very cautious about bread and other baked goods (although in Tuscany , bread is traditionally made without salt, that is seldom true anywhere else). That said, while almost no restaurants will make low-salt sauces for you from scratch, as they were already prepared hours before your meal, quite a few restaurants will work with you to provide you with low-salt items like undressed salads with no cheese or croutons, to which you can add oil and vinegar; steamed items without sauce; dishes that are sauteed or stir-fried without salt, soy sauce, salty stocks, et al.; or sometimes, baked vegetables or other baked or grilled items to which salt has not been added. However, it is quite unsafe to assume a restaurant will accommodate you if you haven't checked with them beforehand in person or by phone (etc.), especially if they are very busy and in a rush to turn over your table to the next customer.
Some cuisines are particularly difficult for people on low-salt diets. For example, in Southeast Asia , most food has shrimp paste, fish sauce or salted, dried shrimps (sometimes ground up) among the ingredients, even if you can't taste them separately. Also, beware of hot sauces, soy sauce, oyster sauce, restaurant-made stocks, and almost all varieties of cheese. And of course, not knowing the local language makes it much more difficult to communicate your health imperatives to your waiter.
Sugar intake [ edit ]
There is increasing evidence that for many people, an excess of dietary sugar may be even worse than an excess of dietary sodium and likely to raise your blood pressure by a greater amount. Keep that in mind and consider limiting or avoiding high-glycemic foods (there are many online lists showing the glycemic index and/or glycemic load of foods; here's another [dead link] ), including sweet desserts made with sucrose (table sugar), white rice, white bread and bagels, and also many processed foods you might not suspect without checking the ingredients list and nutrient panel. In certain countries such as the United States , it's also very common for all sorts of restaurants to add lots of sugar to sauces to please customers' sweet teeth.
Conclusion [ edit ]
While it may be OK for people with controlled blood pressure to eat out now and then, especially if your blood pressure remains on the high side while on medication, you are really best off cooking your own food as much as possible, if you can.
Drink [ edit ]
People with high blood pressure might consider limiting or avoiding the intake of caffeine (such as in coffee , tea , hot chocolate and colas), alcohol (see here , for example) and sugary drinks including sodas and sweet juices. In terms of alcoholic beverages, note in particular that cocktails almost all have sugar or some other sweetener as a major ingredient. However, even if you completely avoid all of these types of beverages, there are many delicious herbal teas and other types of drinks that you may find in your travels. As for the rest, consult your physician, but it's quite possible that in moderation, a bit of alcohol or tea now and then may not do you appreciable harm.
Sleep [ edit ]
If you can stay in accommodations with at least some cooking facilities and a refrigerator, it will be easier for you to control your diet.
Stay safe [ edit ]

If your blood pressure goes up to a life-threatening level (as a general reference the American Heart Association considers 180/120 a hypertensive emergency requiring immediate medical care), get to an emergency room in a hospital immediately! Also, be cautious about physical symptoms involving very high blood pressure (especially fainting, severe headache and various other kinds of persistent pains), even if your blood pressure is a bit lower than the nightmare numbers mentioned above.
Do not feel impelled to avoid all physical activity unnecessarily; double-check with your physician, but the chances are, s/he will tell you that exercise, within appropriate limits for your fitness level, is good for your health. But do try not to overexert yourself. If you feel short of breath or have other symptoms of exhaustion, stop what you are doing, sit down and relax, and if you are doing anything very strenuous that could put you in danger, make sure not to do it by yourself, so that in a pinch, another person can get help for you.
See also [ edit ]
- Dealing with emergencies
- Physical fitness
- Senior travel
- Stay healthy
- Has custom banner
- Articles with dead external links
- Topic articles
- Usable topics
- Usable articles
Navigation menu

Traveling With High Blood Pressure: Travel Tips From Cardiologist Dr. Desai
Dr. Monali Desai is a practicing cardiologist in New York and founder of IfWeWereFamily.com where she writes about health and nutrition, offering science-backed advice for living a healthier life.
High blood pressure, also known as hypertension, does not always have noticeable symptoms. But when signs do show, they can include a variety of symptoms: severe headaches, fatigue or confusion, vision problems, chest pain, and difficulty breathing.
Traveling can be stressful. If you have high blood pressure, being stressed can raise your blood pressure even further.
Many things can happen during travel that can make your blood pressure high. Stress can come from being late, experiencing delays and setbacks, and worrying about having remembered everything.

Nine tips for traveling with high blood pressure
At the airport
1. Get to the airport early. Leave yourself plenty of time to check your bag, go through security, and get to your gate early. If you’re stressed out about missing your flight, this can raise your blood pressure.
On the plane
2. Avoid eating salty snacks and drinking alcohol. This can change the salt-to-water balance in your body and increase your blood pressure. Staying well hydrated with water is also essential for the same reason.
3. Keep extra blood pressure medication in your carry-on bag in case your flight or trip is delayed or your checked bag gets lost.
4. Stay mobile on the plane. Walk in the aisles, especially on long flights. This will help prevent blood clots.
While Traveling
5. Watch out for your body’s salt-to-water ratio getting out of balance and making your blood pressure high. This can happen by eating too many salty foods, being outside in the sun, and not drinking enough water.
6. Portable blood pressure machines are relatively small and inexpensive, so take one with you.
7. Make sure you have enough blood pressure medication to last for the duration of your trip. It’s also a good idea to take at least an extra week’s worth of medication in case your trip is delayed. If you’re in your home country and you do run out, ask your doctor’s office to call in replacement medication to a local pharmacy.
8. If you’re in a foreign country, it’s a good idea to take a copy of your prescription with you, in case your medication gets lost and you need to get some more from a local chemist or doctor.
Ask your hotel for a recommendation for a local doctor or chemist who can prescribe replacement medication until you get back home.
Be aware that different countries don’t necessarily carry the same tablets you’re taking at home. If your medication does get lost or you run out, missing it for a few days can be dangerous to your health as it increases your risk of heart attack and stroke.
9. Buy travel insurance in case something happens while you’re on vacation and you need to go to the doctor. Always make sure you are properly insured before traveling. It’s important to let your insurer know if you have been diagnosed with high blood pressure too.

Monali Desai
Dr. Monali Desai is a cardiologist and a contributor for Thrive Global. She has been featured on a variety of sites including Healthline, Shape, and mindbodygreen. She writes about a wide range of topics from preventative cardiology to holistic medicine. Follow her on Instagram for more science-backed health and nutrition tips.
Hotel Review: The Beaumont in London Is An Artful Escape from the Busy City
6 of the scariest things about airports to send a shiver down your spine, leave a reply cancel reply.
Your email address will not be published.
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Try These 5 Tips To Prevent Lost Luggage Next Time You Travel

Gary, the Gold Coast Airport therapy dog has returned

In-flight tips during covid from a New York travel professional

Seven therapy dog programs now back at airports

Fifteen New Therapy Dog Programs Launched In The US in 2019
Useful Pages
Travelling with high blood pressure.

If your high blood pressure is under control, it should not prevent you from travelling or flying. However, you should still take precautions to maintain good health and prevent high blood pressure occurring when on holiday.
What is hypertension (high blood pressure)?
Hypertension is the medical term for high blood pressure. More than one in four adults in the UK have high blood pressure.
High blood pressure is when your blood pressure (the force of your blood pushing against the walls of your blood vessels) is consistently too high.
To find out if you have high blood pressure, visit your GP or local pharmacy to get your blood pressure checked.
What are the symptoms of high blood pressure?
High blood pressure is hard to detect and you may have it without realising. If your blood pressure is extremely high, you might experience symptoms like severe headaches, fatigue, difficulty breathing, chest pain and irregular heartbeat.
Risk of high blood pressure
High blood pressure puts pressure on your heart and other organs (brain, kidneys, eyes). If you have untreated high blood pressure you are at risk of developing serious conditions such as heart disease, kidney disease or a stroke.
Causes of high blood pressure
You are at risk of developing high pressure if you:
- are 65 or over
- are overweight (or obese)
- don't exercise
- drink excessive amounts of alcohol
- have a relative with high blood pressure
Visit your doctor regularly to check your blood pressure, especially before travelling.
Flying with high blood pressure
It is safe to fly with high blood pressure if it is well controlled. However, you may experience some discomfort during your flight such as an earache. Your blood pressure is likely to rise as well, but this is normal. If your blood pressure is unstable or very high, then you should talk to your doctor before flying.
Rises in blood pressure
Aeroplane cabins have less oxygen. Less oxygen in the blood can lead to high blood pressure.
If you already have high blood pressure, you are at a higher risk of developing heart failure, coronary artery disease, and other health conditions. This doesn't mean you can't fly, but you must take precautions to lower your risk.
Avoid salty food or drinking alcohol. If you take blood pressure medication, pack it in your carry-on so you can take it as needed.
Deep Vein Thrombosis
Deep vein thrombosis (DVT) occurs when a blood clot forms in the leg. The clot can break off and move through the blood to your brain, lungs or heart (causing an embolism). Flying puts you at higher risk of developing DVT since it limits your mobility.
You can take precautions to keep your blood circulating as normal, these include wearing comfortable and loose-fitting clothing, bending and straightening your legs, massaging your calf muscles, and walking up and down the aisles.

Earache or temporary hearing loss
Why you fly, you might experience a painful earache or temporary hearing loss to due to the rapid change in altitude as the plane takes off and lands. There are some things you can do to avoid a painful earache.
Try swallowing which will cause the air pressure in your ear to equalise, chewing gum or sucking on hard boiled sweets, yawning, and drinking lots of water.
What to consider before planning your trip
Choosing a holiday destination.
If you have high blood pressure, deciding on a holiday destination may be challenging, as you may have health-related concerns to consider. Use the gov.uk website for travel advice by country.
Environment
When choosing a holiday environment, think about the symptoms and what makes these worse.
Extreme heat can cause dizziness or fainting, and risk dehydration. Hilly places require you to be physically fit and can make you breathless. Are there adequate amenities (you may take diuretics and need to use the toilet frequently).
Accommodation
Does your accommodation suit your access needs? Do you need to avoid flights of stairs or need to use a lift? Choose ground-floor accommodation. Contact your preferred accommodation to check what help will be available to you.
Altitude sickness
Travelling to high altitudes (5,000 to 11,500 feet above sea level) can raise a person’s blood pressure. At high altitudes, the blood in your body works harder to pump oxygen. This stress can cause high blood pressure.
However, if you have already booked your trip, there are ways to manage your blood pressure at high altitude. Experts recommend only light physical activity to avoid putting a strain on your heart. You should avoid climbing more than 300 meters per day when in high-altitude locations to reduce breathlessness.
If you are yet to book your trip, you should avoid countries with high altitude. Countries like:
And be especially careful if you’re staying in mountainous regions such as the Alps.
If your high blood pressure is under control, and you take some precautions, travelling at high altitudes shouldn't be a problem.
Preparing for your trip
Speak to your gp.
Visit your GP eight weeks before you travel to discuss your travel plans. Your doctor will check your blood pressure and determine if it is suitable for you to fly. If you are considered unfit to fly, your GP will advise you on how to change your travel plans to suit your needs.
Prepare your medication
If you are taking blood pressure medication and your journey will involve you being away from home for more than a couple of weeks, make sure you have enough medication to last the duration of your trip—usually enough for your holiday plus an extra week. And never put them in your checked-in luggage, if your case is lost or stolen, you’ll lose all your medication. Always store it in your carry-on.
Remember to pack your blood pressure monitor, especially if you have high blood pressure (pulmonary hypertension) or your blood pressure isn't well controlled. A blood pressure monitor ensures that your blood pressure remains within a safe range.
Travelling checklist
It may be helpful to carry the following with you in your hand luggage:
- your passport
- your EHIC card
- your insurance documents
- your prescription or a list of your medication
- a letter from your GP or specialist explaining your condition (if required)
- any tests results you think might be important (ECG record)
- a portable blood pressure monitor (if needed)
- oxygen if you suffer from pulmonary hypertension
- flight socks
- travel sickness medication
- Healthy snacks and water
High blood pressure and travel insurance
Do i need travel insurance if i have high blood pressure.
If your blood pressure is normal, but you have had high blood pressure previously, or you use medication to keep your blood pressure low, you will need to declare it as a pre-existing medical condition.
If you have complications abroad and haven't declared your condition, your claim may be invalid. It is vital that you state your pre-existing condition even if your blood levels are normal.
How to apply for travel insurance
We make it easy for people with high blood pressure to find insurance. Take our blood pressure questionnaire . Our questionnaire will ask you to enter your details and answer any questions relevant to your condition. Your answers allow us to assess your current health condition and list suitable insurance options, which means we’ll do the searching for you.

Apply for an EHIC medical card
If you’re travelling in Europe, make sure you own a European Health Insurance Card (EHIC card). The EHIC card protects you from expensive medical bills and may allow you to receive free or reduced-cost health care.
Visit our EHIC card page for details about how to apply, renew or replace an EHIC card plus a comprehensive list of countries it’s accepted in, and the circumstances it covers.
Travelling with children with high blood pressure
Children of all ages (from birth to teens) can have high blood pressure. Just like high blood pressure in adults, it's hard to spot and often goes unnoticed. Children with high blood pressure should be treated the same as adults when travelling.
If your child has a history of high blood pressure or takes medication to control it, consult your GP about your travel plans.
When not to travel with high blood pressure
As long as your blood pressure is controlled, you should be able to travel as normal. Check with your doctor if you are unsure about how fit you are to travel.
What do the different blood pressure readings mean?
- Less than 120 over 80: Your blood pressure is normal.
- Between 120 over 80 and 140 over 90: Your blood pressure is higher than normal.
- 140 over 90 or higher: You have high blood pressure. You should consult your GP.
If your blood pressure is higher than 120 over 80, seek medical advice before you travel.
Enjoy your trip!
Having high blood pressure should not stop you from enjoying a globe-trotting lifestyle. Travelling abroad, including flying, is generally fine if your high blood pressure is well controlled.
More advice
- Travel advice
- Medical condition - High Blood Pressure
Ready for your online quote?
Tired of looking around for medical travel insurance? Why not use our quick and simple quote engine?
In need of assistance?
Our medical travel insurance team are ready to provide you with assistance regarding your quote. If you would prefer to talk to an advisor to receive a quote or have a query please contact our UK based customer service team. Find out details on our contact us page .

Medical travel insurance is an online comparison website for those with pre-existing medical conditions requiring travel insurance. Medical travel insurance www.medicaltravelinsurance.co.uk is a trading style of Brokersure Ltd. Brokersure is authorised and regulated by the FCA.
For more information regarding Medical Travel Insurance click here , alternatively phone or email us.
Phone: 0330 880 3601
Email: [email protected]
- Medical Travel Insurance
- Digital House
- Threshelfords Business Park
- Inworth Road
Opening Hours
- Open Monday to Friday 8:30am to 6pm, Saturday 8:30am to 4pm and closed Sundays
Useful Links
- Get a Quote
- Policy Documents
- Terms & Conditions
- Terms Of Business

Medicaltravelinsurance.co.uk travel insurance is a trading style of Brokersure Ltd who are authorised and regulated by the Financial Conduct Authority. FCA No: 501719. Brokersure Ltd, Digital House, Threshelfords Business Park, Inworth Road, Feering, Essex, CO5 9SE.
Copyright © Brokersure Ltd 2024. All rights reserved.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 06 January 2022
Travelling with heart failure: risk assessment and practical recommendations
- Stephan von Haehling 1 , 2 ,
- Christoph Birner 3 , 4 ,
- Elke Dworatzek 5 , 6 ,
- Stefan Frantz 7 ,
- Kristian Hellenkamp 1 ,
- Carsten W. Israel 8 ,
- Tibor Kempf 9 ,
- Hermann H. Klein 10 ,
- Christoph Knosalla ORCID: orcid.org/0000-0002-8127-5019 6 , 11 , 12 ,
- Ulrich Laufs ORCID: orcid.org/0000-0003-2620-9323 13 ,
- Philip Raake 14 , 15 ,
- Rolf Wachter 1 , 2 , 13 &
- Gerd Hasenfuss 1 , 2
Nature Reviews Cardiology volume 19 , pages 302–313 ( 2022 ) Cite this article
40k Accesses
6 Citations
165 Altmetric
Metrics details
- Heart failure
- Patient education
Patients with heart failure are at a higher risk of cardiovascular events compared with the general population, particularly during domestic or international travel. Patients with heart failure should adhere to specific recommendations during travel to lower their risk of developing heart failure symptoms. In this Review, we aim to provide clinicians with a set of guidelines for patients with heart failure embarking on national or international travel. Considerations when choosing a travel destination include travel distance and time, the season upon arrival, air pollution levels, jet lag and altitude level because all these factors can increase the risk of symptom development in patients with heart failure. In particular, volume depletion is of major concern while travelling given that it can contribute to worsening heart failure symptoms. Pre-travel risk assessment should be performed by a clinician 4–6 weeks before departure, and patients should receive advice on potential travel-related illness and on strategies to prevent volume depletion. Oxygen supplementation might be useful for patients who are very symptomatic. Upon arrival at the destination, potential drug-induced photosensitivity (particularly in tropical destinations) and risks associated with the local cuisine require consideration. Special recommendations are needed for patients with cardiac implantable electronic devices or left ventricular assist devices as well as for those who have undergone major cardiac surgery.
Patients with heart failure (HF) are recommended to schedule a specialist consultation for pre-travel risk assessment 4–6 weeks before departure.
Preparation for travel requires special considerations in patients with HF, including the choice of destination, availability of medical resources and strategies to prevent volume depletion.
Most patients with HF can travel when medically stable; patients with a ground-level oxygen saturation ≤90% or those in NYHA class III–IV might need an on-board medical oxygen supply.
All medication and important documents should be stored in carry-on luggage.
Volume depletion and dehydration are important considerations requiring meticulous attention with regards to medication adjustment and fluid intake.
Patients with implantable cardiac devices might require extra time at security checkpoints and additional documents; for some patients, remote monitoring of implantable cardiac devices might be useful.
Similar content being viewed by others

Evaluating the “holiday season effect” of hospital care on the risk of mortality from pulmonary embolism: a nationwide analysis in Taiwan
The role of cardiac rehabilitation in improving cardiovascular outcomes
Variation in community and ambulance care processes for out-of-hospital cardiac arrest during the COVID-19 pandemic: a systematic review and meta-analysis
Introduction.
Domestic and international travel are associated with increased health risks, with 20–70% of individuals reporting health issues during their travels 1 . During international travel, 1–5% of individuals seek medical attention and the rate of death among travellers is 1 in 100,000, with cardiovascular disease being the most frequent cause of death 1 . Trauma, particularly from motor vehicle accidents, is another major cause of death while travelling 1 . Health-care providers are frequently approached by patients for advice on how to prepare for travel or to determine whether travelling is advisable at all. General practitioners can provide information to healthy individuals but specialist consultation is of benefit for patients with underlying illnesses such heart failure (HF) 2 . Indeed, many patients with HF intend to travel for business or leisure. Although some guidance has been published 3 , a systematic overview of recommendations for patients with HF planning to travel is not yet available. In this Review, we aim to provide clinicians with recommendations for preparatory measures before travel to inform and educate patients with HF. We discuss factors that might increase the risk of HF symptom development, such as local climate, air pollution levels and altitude levels, and provide specific guidance for patients with a cardiac implantable device and those who have undergone major surgery.
Which patients with HF can travel safely?
To date, guidance on travel recommendations for patients with HF is limited. In general, patients with NYHA class I–III HF who are stable should be able to travel safely 4 . However, patients with NYHA class III HF who are planning to travel by air should be advised to consider on-board medical oxygen support. Patients with NYHA class IV should not travel; however, if travel is unavoidable, on-board oxygen and medical assistance should be requested. A patient with an oxygen saturation rate >90% at ground level usually will not require medical oxygen during flight 5 . An overview of whether travelling is advisable for different classes of HF 6 , 7 is provided in Box 1 . An overview of contraindications for air travel in patients with cardiovascular diseases is provided in Box 2 .
Box 1 Travel recommendations for patients with heart failure
Chronic stable heart failure
NYHA class I–II: travel advisable, if patient is stable
NYHA class III: travel advisable, if patient is stable; consider use of on-board medical oxygen during air travel
NYHA class IV: travel not advisable; if travel is unavoidable, on-board oyxgen and medical assistance are required
Acute heart failure decompensation
Travel not advisable until at least 6 weeks after discharge and rehabilitation, if patient is stable
Ventricular assist device implantation
Travel advisable after hospital discharge and rehabilitation, if patient is stable
Heart transplantation
Not advisable until at least 1 year after transplantation surgery, if patient is stable
Implantable cardioverter–defibrillator or cardiac resynchronization therapy implantation
Not advisable until at least 2 weeks after discharge, if patient is stable
Box 2 Contraindications for air travel in patients with cardiovascular disease
Myocardial infarction (ST-elevation or non-ST-elevation myocardial infarction) within the previous 2 weeks
Unstable angina without further diagnostics and treatment
Percutaneous coronary angioplasty within the previous 2 weeks; in patients who have undergone uncomplicated percutaneous coronary intervention, shorter time frames might be acceptable
Cardiac surgery or interventional valve therapy within the previous 3 weeks
NYHA class IV heart failure or any decompensated heart failure
Untreated arrhythmias (ventricular or supraventricular)
Eisenmenger syndrome
Uncontrolled pulmonary artery hypertension
Pneumothorax (such as after major cardiac surgery)
Choice of destination
The choice of destination for travel can have important health implications for patients with HF, particularly when travelling abroad. Considerations include the local climate, air pollution levels, altitude levels, the season upon arrival, the distance and time for travelling, jet lag, and vaccines required.
Effects of transitioning climates on HF
Individuals who transition through climates different to the one they reside in (such as someone living in the arctic travelling to a tropical island) are at an increased health risk. In general, people living in warmer regions tend to be most vulnerable to cold weather and, conversely, those residing in a cold climate are most sensitive to heat 8 . Exposure to extreme heat has been associated with increased morbidity and mortality from heat exhaustion and heat stroke 9 , 10 . Maintenance of homeostasis during hot weather requires an increase in cardiac output; heat tolerance is impaired when cardiac output cannot be increased to meet the requirements of heat loss. Numerous medications that are frequently prescribed for individuals with HF can also increase susceptibility to heat stroke, including loop diuretics, serotonic antidepressants, angiotensin-converting enzyme inhibitors and proton-pump inhibitors 11 , 12 , 13 . Colder temperatures are less likely to have effects on cardiovascular health but have been associated with increased morbidity among patients with respiratory disease 14 . Patients with HF should be advised to choose either spring or autumn for international travel to avoid travelling during extremities in weather and to adjust medications that can contribute to volume depletion. Appropriate clothing is required for the site of departure, the destination and for the journey itself. Given the challenges in contacting a patient’s primary care physician if the patient is in a different country or continent, distant travel destinations might only be advisable for patients who are well-informed about their medication regimen, dietary restrictions and exercise limitations.
Endemic diseases
The need for immunization for travel depends on the destination. In general, the status of routine vaccinations, such as the diphtheria, measles–mumps–rubella, pertussis, tetanus and varicella vaccines, should be checked before travelling abroad. For all patients with HF, vaccines are required for pneumococcal disease, influenza and coronavirus disease 2019 (COVID-19). Other destination-dependent vaccines are provided in Table 1 .
Air pollution and HF
Air pollution can be measured by the air quality index, which integrates measures for the five main air pollutants: ground-level ozone, particulate matter, carbon monoxide, sulfur dioxide and nitrogen dioxide. An air quality index value of 0–50 indicates good air quality, 51–100 indicates moderately polluted air, >100 indicates an unhealthy level of air pollution and >300 designates a hazardous environment 15 . Particulate matter (PM) of ≤10 µm (PM 10 ) or ≤2.5 µm (PM 2.5 ) in diameter are linked with increased cardiopulmonary mortality 16 , 17 as well as with an increased risk of hospitalization for HF 18 and death 19 . The pathophysiological mechanisms underlying this increased risk remain elusive. Accumulating evidence points towards a crucial role of PM-induced systemic oxidative stress 20 and endothelial dysfunction 21 in the development of arterial vasoconstriction and elevated systemic blood pressure 22 . In addition, PM-induced pulmonary vasoconstriction results from increases in pulmonary and right ventricular diastolic filling pressures, which affect right ventricular performance 22 . Given that the effects of air pollutants on cardiovascular performance and outcomes can occur within hours or days of exposure 23 , patients with HF should be advised to avoid travelling to locations with high levels of air pollution.
Altitude-induced hypoxia and HF
Patients with HF are more susceptible to the physiological changes induced by high altitude exposure than the general population 24 . During air travel, cabin pressure is required to be no less than the barometric pressure at an altitude of 2,438 m (8,000 ft), which is classified as an intermediate altitude 25 (Fig. 1a ). Cabin pressures usually remain higher than this altitude, particularly during long-haul flights 26 . Travel to high altitude locations that are >2,500 m above sea level triggers physiological acclimatization processes within the cardiocirculatory and pulmonary systems 27 , 28 (Fig. 1b ). These processes are initiated by a gradual decrease in barometric pressure, which in turn lowers the partial pressure of oxygen in inspired air. Hypobaric hypoxia leads to a fast increase in respiratory rate and tidal volume 29 , which leads to respiratory alkalosis and hypoxic diuresis 30 . Hypoxia induces pulmonary vasoconstriction and eventual pulmonary hypertension, an important trigger for high altitude pulmonary oedema 31 . To compensate for the lower arterial oxygen content, heart rate and stroke volume are increased via activation of the sympathetic nervous system 26 , 32 , 33 , 34 . Together, these physiological adaptations limit the exercise capacity of patients with HF and make them prone to cardiac decompensation. However, studies that assessed simulated altitude-induced hypoxia in patients with NYHA class III–IV HF showed that high altitude was not associated with angina, arrhythmia, or ischaemia 35 , 36 and that the degree of the reduction of maximum work capacity was dependent on the individual’s exercise tolerance at sea level 35 . The ESC and other professional societies recommend that the assessment of safety of high altitude exposure for patients with HF should depend on their functional capacity (that is, NYHA class) at sea level 35 , 37 . Furthermore, certain drugs that are prescribed to patients with HF can further interfere with the physiological adaptation processes at high altitudes. For example, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers can reduce renal erythropoietin production, thereby hampering the compensatory rise in haematocrit mediated by altitude-induced hypoxia 38 . Therefore, diuretic therapy should be tailored to the individual to account for clinical signs of dehydration (such as through hypoxic diuresis) or fluid gain 39 . Finally, anaemia reduces oxygen delivery, and muscle loss (present in patients with sarcopenia or cachexia) reduces maximal physical workload and time to fatigue; patients with these conditions in addition to HF need to have special considerations when planning to travel to high altitude locations. To summarize, travel to destinations at an intermediate altitude (~2,000 m) is safe for patients with HF who have good exercise tolerance at sea level.
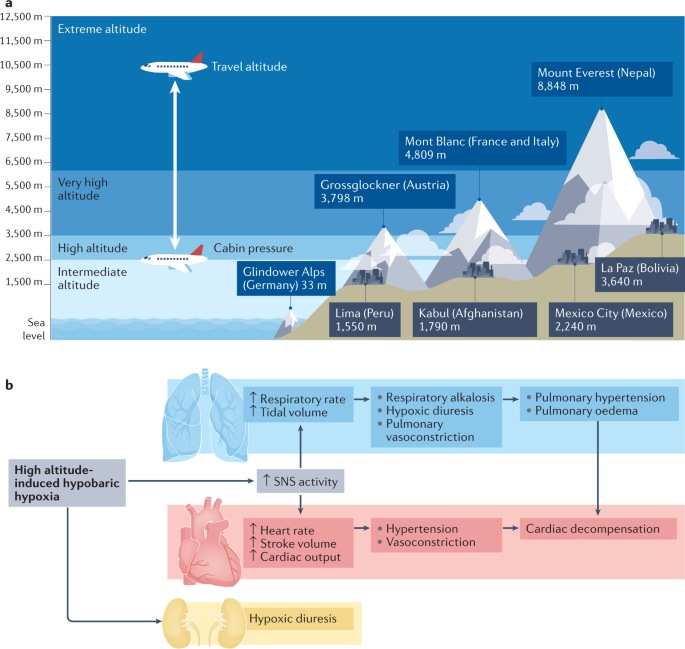
a | Definitions of height and examples of mountains and cities at different altitudes. Most aircraft fly at approximately 10,000–12,000 m (33,000–42,000 ft) above sea level, with the cabin pressurized to an equivalent of 2,438 m (8,000 ft). b | High altitude-induced hypobaric hypoxia leads to an increase in respiratory rate and tidal volume, which promotes respiratory alkalosis, hypoxic diuresis, pulmonary vasoconstriction and, ultimately, pulmonary hypertension and pulmonary oedema. Compensatory mechanisms of this hypoxia include increases in heart rate and stroke volume via activation of the sympathetic nervous system (SNS). Together, these changes can limit exercise capacity and promote cardiac decompensation.
Seasonal variations and HF
Hospitalizations owing to worsening HF show intriguing seasonality, with a substantial decline during warmer periods and an increase during colder periods 18 , 40 , especially in older patients 41 . Temperature had the greatest (inverse) correlation with hospitalizations for HF among other causative environmental factors such as humidity, precipitation or irradiation 16 . Skin cooling has been shown to increase vascular resistance 42 and plasma noradrenaline concentration 43 , which might lead to HF decompensation. Beyond neurohumoural activation and haemodynamic stress, respiratory infections, which peak during the colder months, can precipitate and aggravate HF symptoms 41 . Furthermore, vitamin D insufficiency during winter has also been linked to worsening HF 44 . Interestingly, the effect of seasonal variability on health is more prominent in elderly people and winter hospitalization is associated with both poorer short-term and long-term prognosis 41 . These observations suggest that patients with more severe HF (and worse prognosis) are prone to decompensation during winter and that these patients and older patients with more advanced disease should be advised to avoid travelling to colder regions. Of note, a study from Norway reported that the Christmas winter period was associated with the highest rates of excess all-cause and cardiovascular deaths 45 . Overall, appropriate clothing and heating strategies need to be carefully selected for optimal stabilization of body core temperatures, vitamin D levels should be measured before departure and supplemented if required, and vaccines against influenza and pneunococcal disease should be administered 40 (Table 1 ).
Preparing to travel
Any patient with a history of HF should seek medical consultation before departure, particularly when travelling overseas or when leaving for a long period. Women are generally more likely to seek pre-travel medical advice than men 46 and are also more likely to have travel-related worries 47 . A cross-sectional national survey found that a low perceived need was among the main causes for avoiding medical care, often because patients expected their illness or symptoms to improve over time 48 . For patients with HF, travel preparation should include a specialist consultation approximately 4–6 weeks before departure. This consultation should follow a structured and sequenced approach, which should involve risk assessment (including an evaluation of medical history and travel itinerary), interventions required before departure (including physical examination or setting up of remote monitoring for cardiac implantable devices) and focused education on topics such as medications and factors that can lead to volume depletion. For example, the presence of anaemia might cause lightheadedness, angina or loss of consciousness, particularly during flights 49 , 50 . Medication regimens should be optimized before departure and patients with iron deficiency should be considered for repletion therapy. Suggestions for topics to cover during this consultation are summarized in Box 3 .
Box 3 Recommendations for pre-travel assessment
Risk assessment
Full medical history (current medications, immunization history, history of surgeries or device implantation, immune status, allergies, pregnancy or breast feeding)
Previous travel experience (particularly to the same destination) or risk tolerance
Travel itinerary (destination, mode of travel, travel distance, season, air pollution levels, potential jet lag, clothing required and altitude)
Activities planned (such as adventure sports or hiking, mass gatherings)
Type of accommodation
In-office interventions
Physical examination, electrocardiogram tracing, biochemistry analysis (plasma levels of creatinine, ferritin, glucose, glycated haemoglobin, N-terminal pro-B-type natriuretic peptide, potassium, sodium, transferrin saturation, thyroid-stimulating hormone, vitamin D and urea, estimated glomerular filtration rate, and lipid profile and liver function tests), full blood count (to identify potential anaemia), exercise test and/or transthoracic echocardiography
Set up remote monitoring of implanted devices
Administration of immunizations (routine vaccines include measles–mumps–rubella, tetanus–diphtheria–pertussis, coronavirus disease 2019 (COVID-19), pneumococcal disease and influenza as well as any destination-specific vaccine that might be needed for diseases such as hepatitis A or yellow fever) or malaria chemoprophylaxis (if required)
Strategies to prevent or treat traveller’s diarrhoea (food and water precautions, oral rehydration, treatment with loperamide and bismuth subsalicylate, and antibiotic self-treatment options for severe diarrhoea)
Focused education before travel
Medical kit and documents required during travel: personal health kit (medication, device information or medical records), evacuation and health insurance
Location of medical facilities at destination
Education on heart failure medication adjustment (to avoid dehydration and volume overload), cardiac device handling, telemonitoring and factors that contribute to volume depletion (excess alcohol, coffee or salt intake; traveller’s diarrhoea)
Patients with a cardiac implanted device should avoid strong electromagnetic fields
Travel-related illnesses: altitude illness, traveller’s thrombosis, bloodborne and sexually transmitted diseases, transportation-associated illnesses, respiratory infections, rabies and other animal-associated illness, and skin conditions and wounds
Personal protection for vector-borne disease (if at risk)
Risk assessment and medication adjustment
As mentioned in the previous section, pre-travel risk assessment should consider the type and duration of travel, the travel destination, and the medical history of the patient. Typical health emergencies that patients with HF might encounter during travel are listed in Table 2 . Patients should be advised that provision of incomplete medical information during a cardiac emergency might increase the risk of death. Any accompanying travellers need to know where to find important documents (Box 4 ) in case of an emergency. Given the difficulty in obtaining prescription drugs in a different country as well as the different brands of drugs having varying strengths in different countries, extra medication should be brought on the trip. Importantly, some over-the-counter drugs might be legal in the patient’s home country but illegal elsewhere (such as certain analgesics).
Box 4 Medication and documents required during travel
Sufficient medication for the whole journey (consider bringing extra drugs in case of unforeseen delays in returning home)
Medication to be kept in carry-on luggage for flights (in case of loss of luggage or emergency)
Photocopy of last prescription
Insurance card
Patient identification card
List of diagnosed health conditions and prescribed medicines
Last discharge letter from hospital
Device interrogation print-out
List of names and phone numbers of cardiologist and other relevant clinicians
Remote device monitoring
Remote monitoring is recommended by the ESC and other professional societies for patients with cardiac implantable devices such as pacemakers, implantable cardioverter–defibrillators (ICDs) and implantable cardiac monitors 51 , 52 , 53 . Most remote monitoring systems use a transmitter (base station) placed in the vicinity of the implanted device, with information sent via an internet connection to a remote monitoring service. Alternatively, alerts can be activated after events that trigger an immediate remote transmission (for example, after ICD shock, detection of ventricular tachyarrhythmias or signs of lead failure). Given that travelling is usually associated with increased physical activity levels, daily remote monitoring might be useful for the detection of events such as arrhythmias, HF decompensation or device malfunction (Box 5 ).
Box 5 Travel-related activities and related cardiac events reported via remote monitoring
Sports (such as swimming and diving)
Arrhythmias (atrial fibrillation, ventricular tachyarrhythmia or premature ventricular contractions)
Heart failure decompensation
Damage to the implanted cardiac lead (fracture or insulation failure)
Cardiac device compression with loss of function (during diving)
Stay in high altitude
Eating out (higher intake of sodium) and alcohol consumption
Reduced adherence to medication
Arrhythmias
Travel by aircraft
Electromagnetic interference with cardiac electronic device
Travel by train or ship
Special considerations
Patients who have undergone recent surgery.
Major cardiac surgery ranges from minimally invasive approaches to complete sternotomy. The Canadian Cardiac Society guidelines on air travel recommend that patients with a haemoglobin level <9 g/dl who have undergone coronary artery bypass graft surgery should be advised against air travel 54 ; recommendations for travel in patients with HF who have undergone coronary artery bypass graft surgery should perhaps be even more conservative. These patients should be advised not to travel by air until intrathoracic gas resorption is completed given that gas expands when air pressure is reduced with increasing altitude (the Boyle law) 4 . Gas resorption usually takes 3–10 days after surgery. Any air remaining in the pericardial space or in the thoracic cavity can expand by up to 60%, which might be dangerous and painful 4 . Indeed, the Aerospace Medical Association guidelines state that pneumothorax is an absolute contraindication to air travel and advocate an interval of 2–3 weeks before flying after thoracic surgery 5 . Furthermore, patients who have had a recent operation are in a state of increased oxygen consumption owing to the trauma of surgery, possible presence of sepsis and increased adrenergic outflow. A 2017 study compared complication rates between ground and air travel 5–25 days after pulmonary resection 55 . Air travel was as safe as ground travel if the chest tubes were removed after the absence of ongoing air leak and an output <300 ml over 24 hours combined with adequate pain medication and an active ambulation schedule.
Patients with LVADs
Left ventricular assist devices (LVADs) are increasingly implanted as a bridging strategy while patients wait for heart transplantation or as a permanent therapy for end-stage HF. Patients in either category can travel by air if medically stable and rehabilitation measures have been performed 56 . Box 6 lists precautions before and during travel for patients with an LVAD.
Box 6 Considerations before and during travel for patients with an LVAD
Considerations before departure
Approval should be sought from the responsible left ventricular assist devices (LVAD) centre, including an airline information letter (templates from LVAD manufacturer)
Closest LVAD centres within the travel destination should be located as possible emergency contacts
All LVAD-related equipment needs to be stored in carry-on luggage with handling advice and emergency contact information attached and batteries should be fully charged before departure
The size and weight of the equipment should be checked to ensure that it can be carried on board the plane and the airport and airline need to be informed about the LVAD before arrival to the airport
Considerations during travel
Flight attendants and other personnel need to be informed about the LVAD and the location of the emergency information card
Patients need to maintain fluid intake to avoid low flow alarms from the LVAD pump
For flights longer than 2 hours, support stockings should be considered
Considerations while en route
Departure from home.
Patients with HF or ischaemic heart disease need to take extra caution on the way to and from the departure point, such as an airport or train station, given the multitude of stressors: commotion, a delay or any last-minute changes to the train or flight, and lifting of heavy luggage, all of which can increase physical and mental exertion and risk of myocardial ischaemia 57 , 58 . As such, travel planning should include estimation of psychological stressors and physical loads as well as a plan for any emergencies (Table 2 ). Pre-planned assistance with luggage or transport by wheelchair at the point of departure might reduce pre-travel stress and physical exhaustion.
Dehydration and fluid intake
Patients with HF are susceptible to volume depletion during travel given that fluid intake, lifestyle and diuretics are tuned precisely to maintain a state of euvolaemia 59 (Fig. 2 ). A hypovolaemic state adversely affects cardiac and renal function, aggravates HF symptoms, and might interfere with the efficacy of HF medications. Fluid loss, caused by changes in temperature, diet (higher salt intake) or as a consequence of traveller’s diarrhoea, might occur during the flight.
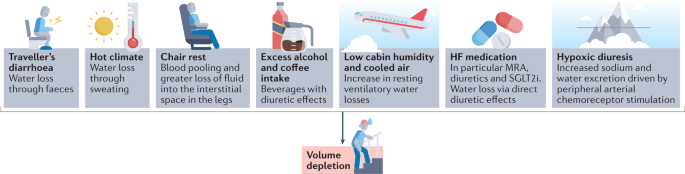
A vast array of factors contributes to volume depletion in patients with heart failure (HF) and require medication adjustment and increased fluid intake. MRA, mineralocorticoid receptor antagonists; SGLT2i, sodium–glucose cotransporter 2 inhibitor.
On board a plane, the low cabin humidity and cooled air can increase resting ventilatory water losses by approximately 200 ml per hour 60 . In addition, chair rest immobilization for 4 hours can decrease plasma volume by approximately 6% as a result of blood pooling and greater loss of fluid within the interstitial space in the legs 60 . Urinary output is often normal or only slightly reduced 61 . Sodium-free, alcoholic or caffeine-containing drinks consumed during the flight can promote diuresis and might further increase fluid loss. Furthermore, arrival to a hot and dry climate can result in loss of fluid through sweating and breathing by up to 1.2 l per day independently of physical activity 62 .
Apart from air travel and a transition in climate, acute diarrhoea is the most common illness in individuals travelling from resource-rich to resource-limited regions of the world 63 , 64 . Traveller’s diarrhoea usually occurs 4–14 days after arrival and results from bacterial (>90% of cases), viral and parasitic infections 64 . Approximately 10–40% of travellers to high-risk regions in Asia, Africa, and South and Central America experience diarrhoea during their travels 64 . Patients should be educated on food and water safety to prevent ingestion of pathogens. Cardiac dysfunction and HF management and treatment strategies, such as fluid restriction, diuretic therapy and renin–angiotensin–aldosterone system (RAAS) inhibitors, also increase the risk of diarrhoea-related complications in patients with HF during (temporal) hypovolaemia 63 , 64 .
Signs and symptoms of volume depletion and dehydration-associated electrolyte or acid–base disorders include fatigue, exercise intolerance, weight loss, increase in heart rate, muscle cramps, weakness, postural dizziness, abdominal pain, low urine volume, low blood pressure, lethargy and confusion. On the basis of invidualized risk assessment, patients should be advised to increase fluid intake by 0.5–1 l per day and to avoid alcohol or excessive coffee consumption during long-haul flights and hot weather. In case of signs and symptoms of volume depletion, therapy with diuretics, mineralocorticoid receptor antagonists and sodium–glucose cotransporter 2 inhibitors should be stopped or reduced for a day or longer until symptoms have resolved and body weight has returned to normal 65 . In case of postural or symptomatic hypotension, therapy with RAAS inhibitors and angiotensin receptor blocker–neprilysin inhibitors should be reduced or discontinued until symptoms have resolved; patients who experience postural or symptomatic hypotension require medical evaluation.
In a hot environment, patients with HF are advised to restrain from strenuous activity to avoid increased fluid loss. In case of uncomplicated traveller’s diarrhoea, patients need to increase fluid intake with oral rehydration solutions and monitor body weight and urinary output to avoid dehydration. Given that patients with HF are at an increased risk of complications, an antimotility agent (loperamide) and an antibiotic (azithromycin or rifaximin) can be prescribed for self-treatment 63 , 64 .
Venous thromboembolism
The risk of deep venous thrombosis (DVT) is greatly increased in patients with incident HF according to data from the ARIC cohort 66 and a systematic review 67 . The term ‘economy class syndrome’ has been used to describe the venous complications caused by cramped seating conditions 68 . The risk of DVT or pulmonary embolism is increased during travel that is >4 hours in duration, most probably owing to the associated immobility that is a key component of the Virchow triad of hypercoagulability, stasis and endothelial injury. Travelling in general (>4 hours in the preceding 8 weeks) is associated with a twofold increase in the risk of venous thrombosis 69 . This risk seems to be similar regardless of the mode of transportation (airplane, bus or train) 67 . The overall absolute incidence of symptomatic venous thromboembolism (VTE) in healthy individuals within the first month after a flight lasting >4 hours is approximately 1 in 4,600 flights and increases by 18% for each additional 2 hours in flight duration 2 , 70 . Importantly, the risk of VTE in individuals with pro-thrombotic risk factors, such as chronic HF, is substantially higher than in the general population. A 2021 meta-analysis found that patients with chronic HF were at an increased risk of VTE (risk ratio 1.57, 95% CI 1.34–1.84) 71 . A window seat compared with an aisle seat has been associated with a twofold greater risk of VTE or a sixfold greater risk in individuals with a BMI of >30 kg/m 2 (ref. 72 ).
Strategies to prevent VTE include appropriate loose clothing, frequent walks, calf muscle exercises, use of elastic compression stockings and adequate hydration 73 . Leg exercises have been shown to improve popliteal venous flow during prolonged immobility in seated individuals 74 . Furthermore, a systematic review of 11 randomized trials that included 2,906 individuals revealed the benefits of compression stockings (15–30 mmHg) on reducing the incidence of asymptomatic DVT and, with less evidence, of leg oedema 75 .
The evidence for thromboprophylaxis to prevent VTE during travel is very limited. The LONFLIT-3 study 76 randomly assigned 300 individuals at high risk of flight-related VTE to receive aspirin, enoxaparine (a low-molecular-weight heparin) or no prophylaxis. In total, 4.8% of patients in the control group were diagnosed with asymptomatic DVT compared with 3.6% in the aspirin group and 0% in the enoxaparine group. The authors of this small study concluded that one dose of enoxaparine might be an important option for individuals at high risk of DVT during long-haul flights 76 . Of note, specific studies of thromboprophylaxis during long-haul travel in patients with HF are lacking.
Medical emergencies during air travel
Patients with HF can travel by air if their condition is stable (Box 1 ). Commercial airplanes are required to carry basic emergency medical equipment according to regulations of the Federal Aviation Administration (FAA) in the USA and the European Aviation Safety Agency (EASA) in Europe 77 . Commercial aircrafts travelling from Europe to the USA have to meet both FAA and EASA requirements and, thus, must carry on board an external automated defibrillator, a saline infusion system and a bag-valve mask resuscitator 77 .
Data on on-board medical emergencies are sparse owing to the lack of international registries 78 . According to the available data provided by the airline Lufthansa, which contains details on approximately 20,000 on-board medical events from 2000 to 2011, cardiac emergencies accounted for 43% of on-board incidents 77 . Reported medical issues included circulatory collapse, high blood pressure, chest symptoms and dehydration 47 . On-board treatment included blood pressure management in 76% of incidents, drug administration in 54%, oxygen delivery in 48%, blood glucose measurement in 9%, monitoring of oxygen saturation in 6% and use of an automated external defibrillator in 6% 77 .
Considerations at the destination
Dietary considerations.
Dietary intake of fluids, sodium, potassium and alcohol during travel should be guided by current ESC recommendations for the management of patients with HF 3 , 79 . According to the guidelines, fluid restriction of 1.5–2.0 l per day might be considered in patients with severe HF to relieve symptoms and congestion 80 . When travelling to hot and dry destinations, an additional intake of 0.5–1.0 l per day of non-alcoholic drinks is recommended. Patients at risk of volume overload or on moderate-to-high doses of diuretics should be advised to regularly check their body weight. In case of body weight changes, patients can adjust doses of diuretics and the amount of fluid intake for a few days until body weight has normalized. Controlling sodium intake is important for patients at risk of hyponatraemia and for the management of oedema, although evidence showing the effects of sodium intake on HF outcomes is scarce 3 . During travel, increased consumption of foods high in salt can adversely affect sodium and volume balance and thereby exacerbate HF symptoms by causing fluid retention. Patients with HF and cardiorenal syndrome and/or treated with RAAS inhibitors are at increased risk of hyperkalaemia 81 . In patients with advanced chronic kidney disease (estimated glomerular filtration rate <30 ml/min/1.73 m²), a daily sodium intake of <3 g is recommended 81 . These patients should also be aware that certain foods, such as fresh fruits, juices, vegetables and milk products, contain high amounts of potassium.
Drinking habits also change during vacation. Moderate-to-heavy alcohol consumption is associated with increased risk of supraventricular arrhythmias, especially atrial fibrillation, and high blood pressure 82 , 83 . Therefore, increased intake of alcoholic beverages might aggravate HF symptoms and promote volume overload. Alcohol intake should be limited to two units per day for men with HF, one unit for women with HF, or no intake if alcohol has caused or contributed to the individual’s HF, as recommended by the ESC 3 .
Drug-induced photosensitivity
Numerous classes of drugs commonly used for the treatment of patients with HF have been associated with photo-induced, cutaneous drug eruptions, which are adverse effects that occur as a result of the exposure to a drug (and its presence in the skin) and ultraviolet or visible radiation 84 . Box 7 provides an overview of drugs that have been linked with drug-induced photosensitivity. Amiodarone can cause drug-induced photosensitivity in >50% of treated patients 84 . The typical presentation of this adverse effect is a burning and tingling sensation in sun-exposed skin, with associated erythema. Amiodarone induces a distinctive blue–grey pigmentation on sun-exposed sites in 1–2% of patients, particularly after long-term sun exposure. Another prototypical drug class associated with photosensitivity is thiazide diuretics, which includes hydrochlorothiazide 85 . Thiazide diuretics can trigger a variety of photosensitive eruptions, including an exaggerated sunburn reaction, dermatitis and a lichenoid eruption.
Various factors, such as time of day, season, geographical location, altitude and weather conditions, can affect the amount of ultraviolet radiation exposure 86 . In general, patients with HF should be advised to seek shade when outside, in particular around midday, and to keep in mind that radiation can be stronger when reflected by water, sand or snow. Patients in areas with high sun exposure should wear clothing that protects as much of the body as possible as well as sunglasses and broad-brimmed hats. Broad-spectrum sunscreens with a sun protection factor of 30 or higher are recommended 86 .
Box 7 Medications linked to drug-induced photosensitivity 80
Angiotensin-converting enzyme inhibitors
Ramipril, enalapril and quinapril
Angiotensin receptor blockers
Candesartan, irbesartan, losartan, olmesartan, telmisartan and valsartan
Anti-arrhythmic drugs
Amiodarone and dronedarone
Anti-depressant drugs
Citalopram, clomipramine, escitalopram, fluoxetine, fluvoxamine, imipramine, paroxetine, sertraline, St. John’s wort and venlafaxine
Antimicrobial drugs
Anti-fungals, anti-malarials, anti-tuberculous drugs, anti-retrovirals, β-lactams, fluoroquinolones, nalidixic acid, sulphonamides and tetracyclines
Calcium channel blockers
Amlodipine, diltiazem and nifedipine
Bumetanide, furosemide, indapamide, thiazides and triamterene
3-Hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors
Atorvastatin, pravastatin and simvastatin
Non-steroidal anti-inflammatory drugs
Ampiroxicam, celecoxib, diclofenac, ibuprofen, indomethacin, ketoprofen, meclofenamide, nabumetone, naproxen, oxaprozin, piroxicam, sulindac and tiaprofenic acid
Psychotropic drugs
Anti-psychotic drugs (aripriprazole, chlorpromazine, clozanine, flupenthixol, haloperidol, olanzapine, risperidone and thioridazine) and anxiolytics (alprazolam and chlordiazepoxide)
Considerations for drivers
Driving regulations for individuals with HF take into account the severity of HF (NYHA class plus left ventricular ejection fraction) 54 . In the European Union, individuals with NYHA class I–III HF but not those with NYHA class IV HF are permitted to drive private vehicles. Patients with HF should ensure that they are permitted to drive in their travelling destination by accessing country-specific driving regulations online.
Considerations for patients with ICDs
Electromagnetic interference.
Many patients with HF are fitted with cardiac implantable electronic devices (CIEDs; namely ICDs), cardiac resynchronization therapy devices or pacemakers. These devices might be subject to electromagnetic interference (EMI) if exposed to a strong electromagnetic field (Table 3 ). Exposure of the device to EMI can result in device failure (loss of anti-bradycardia pacing with the risk of asystole), switch to asynchronous mode (pacing at a preset rate independent of intrinsic rhythm with the risk of inducing arrhythmias, including ventricular fibrillation), inappropriate tracking (atrial oversensing leading to rapid, irregular ventricular pacing) and in the inappropriate detection of ventricular tachyarrhythmias by ICDs, potentially with inappropriate shock therapy. High-voltage lines above trains, for example, have a strong electromagnetic field but the patient is shielded when inside the train. In trams or underground trains, electric motors can be located under the seat, whereas in cars and motorbikes, the only relevant source of EMI is the ignition system. Patients with a cardiac implantable device should be careful not lean over an unshielded, running motor.
Metal detectors at airport security checkpoints do not interfere with CIEDs 87 , 88 . However, patients with ICDs should be advised to have their device card ready to show to airport personnel before walking through the security checkpoint. To minimize the risk of interference, patients should move through metal detector gates at normal walking speed and should not linger. Hand-held scanners should not affect CIED functionality 89 but patients should ask personnel to move the wand over the device quickly and only once.
Magnets are not allowed in carry-on luggage and thus cannot be used to remedy inappropriate device activity on airplanes. EMI inside airplanes is rare but has been reported, for example, in association with electronic chair handles. Finally, cosmic radiation is approximately 100-fold higher during air travel, which increases the risk of radiation-induced EMI (for example, power-on reset).
Conclusions
The list of considerations for patients with HF embarking on national or international travel is extensive. Patients should be aware of an increased risk of cardiovascular events during their travels, which can be reduced with meticulous pre-travel risk assessment, physical examination, therapy adjustment and education. Pre-travel risk assessment should involve research into the local climate, air pollution levels, the distance and time for travelling, potential jet lag and altitude. En route, patients with HF should avoid volume depletion caused by extended chair rest, low cabin humidity and cooled air, excess alcohol or coffee intake, drugs with diuretic effects, hypoxia or traveller’s diarrhoea. Upon arrival at the destination, drug-induced photosensitivity and the health effects of local foods and beverages require consideration. Special recommendations are needed for patients after implantation of cardiac rhythm devices or LVADs as well as for patients who have undergone major cardiac surgery.
Ryan, E. T. & Kain, K. C. Health advice and immunizations for travelers. N. Engl. J. Med. 342 , 1716–1725 (2000).
Article CAS PubMed Google Scholar
Freedman, D. O., Chen, L. H. & Kozarsky, P. E. Medical considerations before international travel. N. Engl. J. Med. 375 , 247–260 (2016).
Article PubMed Google Scholar
Jaarsma, T. et al. Self-care of heart failure patients: practical management recommendations from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 23 , 157–174 (2021).
Smith, D. et al. Fitness to fly for passengers with cardiovascular disease. Heart 96 (Suppl. 2), ii1–ii16 (2010).
PubMed Google Scholar
Aerospace Medical Association. Medical considerations for airline travel: surgical conditions (ASMA, 2021).
Dharmarajan, K. et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ 350 , h411 (2015).
Article PubMed PubMed Central Google Scholar
Alba, C. et al. Complications after heart transplantation: hope for the best, but prepare for the worst. Int. J. Transpl. Res. Med. 2 , 022 (2016).
Article Google Scholar
Curriero, F. C. et al. Temperature and mortality in 11 cities of the eastern United States. Am. J. Epidemiol. 155 , 80–87 (2002).
De Blois, J. et al. The effects of climate change on cardiac health. Cardiology 131 , 209–217 (2015).
Kenny, G. P., Yardley, J., Brown, C., Sigal, R. J. & Jay, O. Heat stress in older individuals and patients with common chronic diseases. CMAJ 182 , 1053–1060 (2010).
Bouchama, A. & Knochel, J. P. Heat stroke. N. Engl. J. Med. 346 , 1978–1988 (2002).
Faunt, J. D. et al. The effete in the heat: heat-related hospital presentations during a ten day heat wave. Aust. N. Z. J. Med. 25 , 117–121 (1995).
Sommet, A., Durrieu, G., Lapeyre-Mestre, M., Montastruc, J. L. & Association of French PharmacoVigilance Centres. A comparative study of adverse drug reactions during two heat waves that occurred in France in 2003 and 2006. Pharmacoepidemiol. Drug Saf. 21 , 285–288 (2012).
McCormack, M. C. et al. Colder temperature is associated with increased COPD morbidity. Eur. Respir. J. 49 , 1601501 (2017).
AirNow. Air Quality Index (AQI) basics. AirNow https://airnow.gov/index.cfm?action=aqibasics.aqi (2019).
Miller, K. A. et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N. Engl. J. Med. 356 , 447–458 (2007).
Pope, C. A. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 287 , 1132–1141 (2002).
Article CAS PubMed PubMed Central Google Scholar
Escolar, V. et al. Impact of environmental factors on heart failure decompensations. ESC Heart Fail. 6 , 1226–1232 (2019).
Shah, A. S. et al. Global association of air pollution and heart failure: a systematic review and meta-analysis. Lancet 382 , 1039–1048 (2013).
Barregard, L. et al. Experimental exposure to wood-smoke particles in healthy humans: effects on markers of inflammation, coagulation, and lipid peroxidation. Inhal. Toxicol. 18 , 845–853 (2006).
Törnqvist, H. et al. Persistent endothelial dysfunction in humans after diesel exhaust inhalation. Am. J. Respir. Crit. Care Med. 176 , 395–400 (2007).
Wold, L. E. et al. Cardiovascular remodeling in response to long-term exposure to fine particulate matter air pollution. Circ. Heart Fail. 5 , 452–461 (2012).
Tofler, G. H. & Muller, J. E. Triggering of acute cardiovascular disease and potential preventive strategies. Circulation 114 , 1863–1872 (2006).
Higgins, J. P., Tuttle, T. & Higgins, J. A. Altitude and the heart: is going high safe for your cardiac patient? Am. Heart J. 159 , 25–32 (2010).
US Office of the Federal Register. Code of Federal Regulations: Title 14 aeronautics and space, part 25.841 (US Government Printing Office, 1986).
Seccombe, L. M. & Peters, M. J. Physiology in medicine: acute altitude exposure in patients with pulmonary and cardiovascular disease. J. Appl. Physiol. 116 , 478–485 (2014).
Imray, C., Booth, A., Wright, A. & Bradwell, A. Acute altitude illnesses. BMJ 343 , d4943 (2011).
Bärtsch, P. & Gibbs, J. S. Effect of altitude on the heart and the lungs. Circulation 116 , 2191–2202 (2007).
Jones, J. G., Bakewell, S. E., Heneghan, C. P., Jones, S. E. & Snape, S. L. Profound hypoxemia in pulmonary patients in airline-equivalent hypoxia: roles of VA/Q and shunt. Aviat. Space Env. Med. 79 , 81–86 (2008).
Sawka, M. N., Convertino, V. A., Eichner, E. R., Schnieder, S. M. & Young, A. J. Blood volume: importance and adaptations to exercise training, environmental stresses, and trauma/sickness. Med. Sci. Sports Exerc. 32 , 332–348 (2000).
Cheung, S. S. et al. Ventilatory chemosensitivity, cerebral and muscle oxygenation, and total hemoglobin mass before and after a 72-day mt. Everest expedition. High Alt. Med. Biol. 15 , 331–340 (2014).
Hughson, R. L., Yamamoto, Y., McCullough, R. E., Sutton, J. R. & Reeves, J. T. Sympathetic and parasympathetic indicators of heart rate control at altitude studied by spectral analysis. J. Appl. Physiol. 77 , 2537–2542 (1994).
Vogel, J. A. & Harris, C. W. Cardiopulmonary responses of resting man during early exposure to high altitude. J. Appl. Physiol. 22 , 1124–1128 (1967).
Heistad, D. D., Abboud, F. M. & Dickinson, W. Richards Lecture: circulatory adjustments to hypoxia. Circulation 61 , 463–470 (1980).
Agostoni, P. et al. Effects of simulated altitude-induced hypoxia on exercise capacity in patients with chronic heart failure. Am. J. Med. 109 , 450–455 (2000).
Negrao, C. E. & Middlekauff, H. R. Adaptations in autonomic function during exercise training in heart failure. Heart Fail. Rev. 13 , 51–60 (2008).
Parati, G. et al. Clinical recommendations for high altitude exposure of individuals with pre-existing cardiovascular conditions: a joint statement by the European Society of Cardiology, the Council on Hypertension of the European Society of Cardiology, the European Society of Hypertension, the International Society of Mountain Medicine, the Italian Society of Hypertension and the Italian Society of Mountain Medicine. Eur. Heart J. 39 , 1546–1554 (2018).
Pratt, M. C. et al. Effect of angiotensin converting enzyme inhibitors on erythropoietin concentrations in healthy volunteers. Br. J. Clin. Pharmacol. 34 , 363–365 (1992).
Swenson, E. R. Carbonic anhydrase inhibitors and high altitude illnesses. Subcell. Biochem. 75 , 361–386 (2014).
Stewart, S., Keates, A. K., Redfern, A. & McMurray, J. J. V. Seasonal variations in cardiovascular disease. Nat. Rev. Cardiol. 14 , 654–664 (2017).
Stewart, S., McIntyre, K., Capewell, S. & McMurray, J. J. Heart failure in a cold climate. Seasonal variation in heart failure-related morbidity and mortality. J. Am. Coll. Cardiol. 39 , 760–766 (2002).
Hayward, J. M., Holmes, W. F. & Gooden, B. A. Cardiovascular responses in man to a stream of cold air. Cardiovasc. Res. 10 , 691–696 (1976).
Westheim, A. et al. Haemodynamic and neurohumoral effects of cold pressor test in severe heart failure. Clin. Physiol. 12 , 95–106 (1992).
Barnett, A. G., de Looper, M. & Fraser, J. F. The seasonality in heart failure deaths and total cardiovascular deaths. Aust. N. Z. J. Public Health 32 , 408–413 (2008).
Moholdt, T. Excess mortality at Christmas due to cardiovascular disease in the HUNT study prospective population-based cohort in Norway. BMC Public Health 21 , 549 (2021).
Schlagenhauf, P. et al. Sex and gender differences in travel-associated disease. Clin. Infect. Dis. 50 , 826–832 (2010).
McIntosh, I. B., Power, K. G. & Reed, J. M. Prevalence, intensity, and sex differences in travel related stressors. J. Travel Med. 3 , 96–102 (1996).
Taber, J. M., Leyva, B. & Persoskie, A. Why do people avoid medical care? A qualitative study using national data. J. Gen. Intern. Med. 30 , 290–297 (2015).
Aerospace Medical Association. Medical considerations for airline travel: anemia (ASMA, 2021).
Roig, E. et al. Disabling angina pectoris with normal coronary arteries in patients undergoing long-term hemodialysis. Am. J. Med. 71 , 431–434 (1981).
Brignole, M. et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur. Heart J. 34 , 2281–2329 (2013).
Dubner, S. et al. ISHNE/EHRA expert consensus on remote monitoring of cardiovascular implantable electronic devices (CIEDs). Ann. Noninvasive Electrocardiol. 17 , 36–56 (2012).
Slotwiner, D. et al. HRS Expert Consensus Statement on remote interrogation and monitoring for cardiovascular implantable electronic devices. Heart Rhythm 12 , e69–e100 (2015).
Simpson, C. et al. Canadian cardiovascular society consensus conference. Assessment of the cardiac patient for fitness to drive and fly – executive summary. Can. J. Cardiol. 20 , 1313–1323 (2004).
Google Scholar
Cassivi, S. D. et al. Safety of air travel in the immediate postoperative period after anatomic pulmonary resection. J. Thorac. Cardiovasc. Surg. 153 , 1191–1196.e1 (2017).
MyLVAD Foundation. 10 Tips for traveling with an LVAD. MyLVAD https://www.mylvad.com/patients-caregivers/discuss-connect/forums/1048-10-tips-traveling-lvad (2011).
Kupper, N., Denollet, J., Widdershoven, J. & Kop, W. J. Cardiovascular reactivity to mental stress and mortality in patients with heart failure. JACC Heart Fail. 3 , 373–382 (2015).
Strike, P. C. & Steptoe, A. A systematic review of mental stress-induced myocardial ischaemia. Eur. Heart J. 24 , 690e703 (2003).
Mullens, W. et al. The use of diuretics in heart failure with congestion - a position statement from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 21 , 137–155 (2019).
Greenleaf, J. E., Rehrer, N. J., Mohler, S. R., Quach, D. T. & Evans, D. G. Airline chair-rest deconditioning: induction of immobilisation thromboemboli? Sports Med. 34 , 705–725 (2004).
Greenleaf, J. E., Shvartz, E., Kravik, S. & Keil, I. C. Fluid shifts and endocrine responses during chair rest and water immersion in man. J. Appl. Physiol. 48 , 79–88 (1980).
Better, O. S. Impaired fluid and electrolyte balance in hot climates. Kidney Int. Suppl. 21 , S97–S101 (1987).
CAS PubMed Google Scholar
Riddle, M. S. et al. Guidelines for the prevention and treatment of travelers’ diarrhea: a graded expert panel report. J. Travel Med. 24 (Suppl. 2), S57–S74 (2017).
Steffen, R., Hill, D. R. & DuPont, H. L. JAMA patient page. Traveler’s diarrhea. JAMA 313 , 108 (2015).
Rosenstock, J. & Ferrannini, E. Euglycemic diabetic ketoacidosis: a predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Diabetes Care 38 , 1638–1642 (2015).
Fanola, C. L. et al. Incident heart failure and long-term risk for venous thromboembolism. J. Am. Coll. Cardiol. 75 , 148–158 (2020).
Trujillo-Santos, A. J., Jiménez-Puente, A. & Perea-Milla, E. Association between long travel and venous thromboembolic disease: a systematic review and meta-analysis of case-control studies. Ann. Hematol. 87 , 79–86 (2008).
Czuprynska, J. & Arya, R. Annotation: travel and thrombosis. Br. J. Haematol. 188 , 838–843 (2020).
Cannegieter, S. C., Doggen, C. J., van Houwelingen, H. C. & Rosendaal, F. R. Travel-related venous thrombosis: results from a large population-based case control study (MEGA study). PLoS Med. 3 , e307 (2006).
Kahn, S. R. et al. Prevention of VTE in nonsurgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141 (Suppl. 2), e195S–e226S (2012).
Xu, T. et al. Heart failure is associated with increased risk of long-term venous thromboembolism. Korean Circ. J. 51 , 766–780 (2021).
Schreijer, A. J., Cannegieter, S. C., Doggen, C. J. & Rosendaal, F. R. The effect of flight-related behaviour on the risk of venous thrombosis after air travel. Br. J. Haematol. 144 , 425–429 (2009).
Dusse, L. M. S., Silva, M. V. F., Freitas, L. G., Marcolino, M. S. & Carvalho, M. D. G. Economy class syndrome: what is it and who are the individuals at risk? Rev. Bras. Hematol. Hemoter. 39 , 349–353 (2017).
Hitos, K., Cannon, M., Cannon, S., Garth, S. & Fletcher, J. P. Effect of leg exercises on popliteal venous blood flow during prolonged immobility of seated subjects: implications for prevention of travel-related deep vein thrombosis. J. Thromb. Haemost. 5 , 1890–1895 (2007).
Clarke, M. J., Broderick, C., Hopewell, S., Juszczak, E. & Eisinga, A. Compression stockings for preventing deep vein thrombosis in airline passengers. Cochrane Database Syst. Rev. 9 , CD004002 (2016).
Cesarone, M. R. et al. Venous thrombosis from air travel: the LONFLIT3 study–prevention with aspirin vs low-molecular-weight heparin (LMWH) in high-risk subjects: a randomized trial. Angiology 53 , 1–6 (2002).
Graf, J., Stüben, U. & Pump, S. In-flight medical emergencies. Dtsch. Arztebl Int. 109 , 591–602 (2012).
PubMed PubMed Central Google Scholar
Goodwin, T. In-flight medical emergencies: an overview. BMJ 321 , 1338 (2000).
McDonagh, T. A. et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 42 , 3599–3726 (2021).
Seferovic, P. M. et al. Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 21 , 1169–1186 (2019).
Kalantar-Zadeh, K. & Fouque, D. Nutritional management of chronic kidney disease. N. Engl. J. Med. 377 , 1765–1776 (2017).
Hindricks, G. et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 42 , 373–498 (2021); erratum 42, 507 (2021); erratum 42, 546–547 (2021).
Tasnim, S., Tang, C., Musini, V. M. & Wright, J. M. Effect of alcohol on blood pressure. Cochrane Database Syst. Rev. 7 , CD012787 (2020).
Drucker, A. M. & Rosen, C. F. Drug-induced photosensitivity: culprit drugs, management and prevention. Drug Saf. 34 , 821–837 (2011).
Blakely, K. M., Drucker, A. M. & Rosen, C. F. Drug-induced photosensitivity-an update: culprit drugs, prevention and management. Drug Saf. 42 , 827–847 (2019).
US Food and Drug Administration. The Sun and your medicine (FDA, 2015).
Kolb, C. et al. Do airport metal detectors interfere with implantable pacemakers or cardioverter-defibrillators? J. Am. Coll. Cardiol. 41 , 2054–2059 (2003).
Copperman, Y., Zarfati, D. & Laniado, S. The effect of metal detector gates on implanted permanent pacemakers. Pacing Clin. Electrophysiol. 11 , 1386–1387 (1988).
Jilek, C. et al. Safety of screening procedures with hand-held metal detectors among patients with implanted cardiac rhythm devices: a cross-sectional analysis. Ann. Intern. Med. 155 , 587–592 (2011).
Download references
Acknowledgements
This Review is the result of a cooperation under the umbrella of the Study Group 10 (heart failure) of the German Cardiac Society. S.v.H. has received research funding from the German Center for Cardiovascular Research (DZHK). T.K. has received research funding from the German Heart Research Foundation and is supported by the German Research Foundation (Clinical Research Unit KFO311). R.W. has received research support from the German Center for Cardiovascular Research (DZHK).
Author information
Authors and affiliations.
Department of Cardiology and Pneumology, University of Göttingen Medical Center, Göttingen, Germany
Stephan von Haehling, Kristian Hellenkamp, Rolf Wachter & Gerd Hasenfuss
German Center for Cardiovascular Research (DZHK), Partner Site Göttingen, Göttingen, Germany
Stephan von Haehling, Rolf Wachter & Gerd Hasenfuss
Department of Internal Medicine II, University Hospital Regensburg, Regensburg, Germany
Christoph Birner
Department of Internal Medicine I, Klinikum St. Marien, Amberg, Germany
Institute of Gender in Medicine, Charité – Universitaetsmedizin Berlin, Corporate Member of Freie Universität Berlin and Berlin Institute of Health, Berlin, Germany
Elke Dworatzek
German Centre for Cardiovascular Research (DZHK), Partner Site Berlin, Berlin, Germany
Elke Dworatzek & Christoph Knosalla
Department of Internal Medicine I, University Hospital Würzburg, Würzburg, Germany
Stefan Frantz
Klinik für Innere Medizin, Kardiologie, Diabetologie and Nephrologie, Evangelisches Klinikum Bethel, Bielefeld, Germany
Carsten W. Israel
Department of Cardiology and Angiology, Hannover Medical School, Hannover, Germany
Tibor Kempf
Helios Klinikum Warburg, Idar–Oberstein, Germany
Hermann H. Klein
Department of Cardiothoracic and Vascular Surgery, German Heart Center Berlin, Berlin, Germany
Christoph Knosalla
Charité–Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humoldt–Universität zu Berlin and Berlin Institute of Health, Berlin, Germany
Klinik und Poliklinik für Kardiologie, Universitätsklinikum Leipzig, Leipzig, Germany
Ulrich Laufs & Rolf Wachter
Department of Cardiology, Angiology and Pneumology, Heidelberg University Hospital, Heidelberg, Germany
Philip Raake
German Center for Cardiovascular Research (DZHK), Partner Site Heidelberg/Mannheim, Heidelberg, Germany
You can also search for this author in PubMed Google Scholar
Contributions
S.v.H. wrote the article. All the authors researched data for the article, contributed to discussion of content, and reviewed and edited the manuscript before submission.
Corresponding author
Correspondence to Stephan von Haehling .
Ethics declarations
Competing interests.
S.v.H. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, Boehringer Ingelheim, BRAHMS, Chugai, Grünenthal, Helsinn, Hexal, Novartis, Pharmacosmos, Respicardia, Roche, Servier, Sorin, and Vifor and has received research funding from Amgen, Boehringer Ingelheim and IMI. T.K. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Novartis, Pharmacosmos, and Vifor and has received research support from Vifor. P.R. has been a paid consultant for and/or received honoraria payments from Abbott, AstraZeneca, Bayer, BDI, Biotronik, Conventus Congressmanagement & Marketing GmbH, CTI GmbH, Daiichi-Sankyo, Deutsche Gesellschaft für Kardiologie, Diaplan, Edwards, Elisabeth-KH Essen, Heart Institute GmbH, Herzzentrum Leipzig, Kelcon, Medizinische Ausstellungs- und Werbegesellschaft Wien, Medtronic, Novartis and Vifor. R.W. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, BMS, Boehringer Ingelheim, CVRx, Daiichi, Medtronic, Novartis, Pfizer, Pharmacosmos and Servier. R.W. has received research support from Boehringer Ingelheim, Bundesministerium für Bildung und Forschung, Deutsche Forschungsgemeinschaft, European Union and Medtronic. G.H. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, Berlin Chemie, Boehringer Ingelheim, Corvia, Impulse Dynamics, Novartis, Servier, Springer and Vifor. All other authors declare no competing interests.
Additional information
Peer review information.
Nature Reviews Cardiology thanks Biykem Bozkurt, Tiny Jaarsma and Simon Stewart for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
von Haehling, S., Birner, C., Dworatzek, E. et al. Travelling with heart failure: risk assessment and practical recommendations. Nat Rev Cardiol 19 , 302–313 (2022). https://doi.org/10.1038/s41569-021-00643-z
Download citation
Accepted : 01 November 2021
Published : 06 January 2022
Issue Date : May 2022
DOI : https://doi.org/10.1038/s41569-021-00643-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Heart failure with preserved ejection fraction: diagnosis, risk assessment, and treatment.
- Stephan von Haehling
- Birgit Assmus
- Johann Bauersachs
Clinical Research in Cardiology (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Risk Factors
- Managing High Blood Pressure
- High Blood Pressure Facts
- Measure Your Blood Pressure
- Hypertension Management Program (HMP) Toolkit
- Publication
- High Blood Pressure Communications Toolkit
- Rapid Evaluations of Telehealth Strategies to Address Hypertension
- Team-Based Care to Improve Blood Pressure Control
- High Blood Pressure Maps and Data Resources
- The Surgeon General's Call to Action to Control Hypertension
- Federal Hypertension Control Leadership Council (The Council)
- About Heart Disease
About High Blood Pressure
- About Stroke
- About Cholesterol
- High blood pressure, also called hypertension, is blood pressure that is higher than normal.
- High blood pressure usually has no warning signs or symptoms.
- High blood pressure usually develops over time.
Definition of blood pressure
Blood pressure is the pressure of blood pushing against the walls of your arteries. Arteries carry blood from your heart to other parts of your body.
What are normal blood pressure numbers?
A normal blood pressure level is less than 120/80 mmHg. 1
No matter your age, you can take steps each day to keep your blood pressure in a healthy range .
What is high blood pressure (hypertension)?
High blood pressure, also called hypertension, is blood pressure that is higher than normal. Your blood pressure changes throughout the day based on your activities. Having blood pressure consistently above normal may result in a diagnosis of high blood pressure (or hypertension).
The higher your blood pressure levels, the more risk you have for other health problems, such as heart disease , heart attack , and stroke .
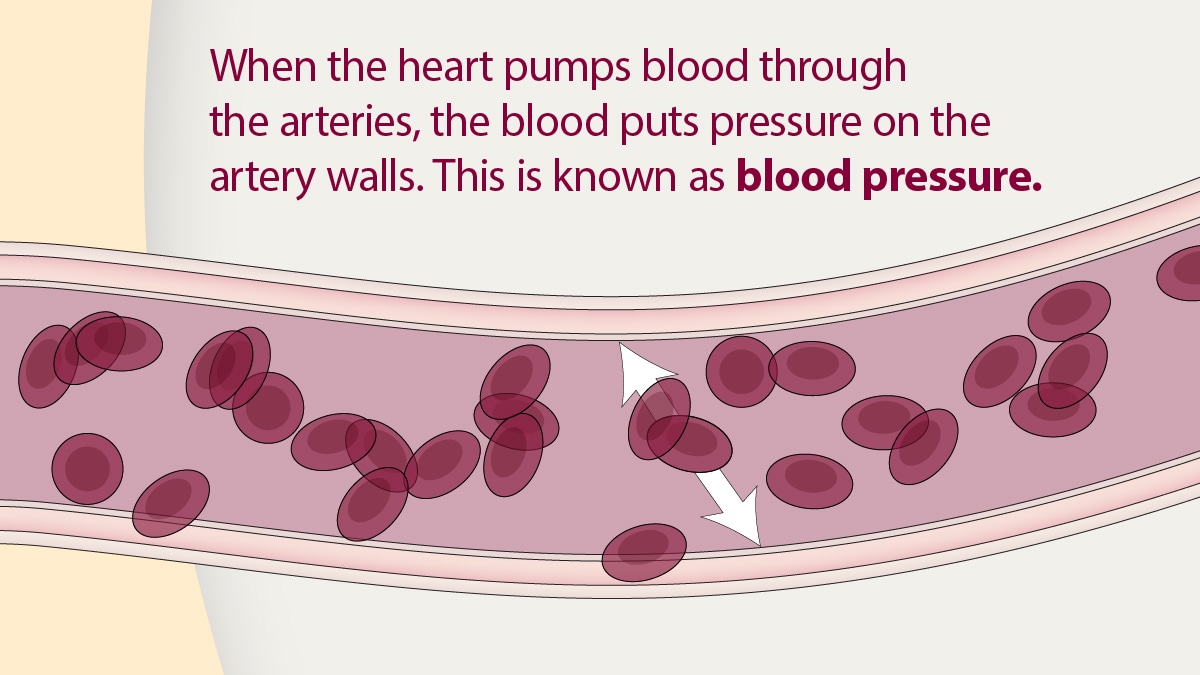
Your health care team can diagnose high blood pressure. They can also make treatment decisions by reviewing your systolic (first number) and diastolic (second number) blood pressure levels and comparing them to guidelines.
The guidelines used to diagnose high blood pressure may differ from one health care provider to another:
- Some health care professionals diagnose patients with high blood pressure if their blood pressure is consistently 140/90 mm Hg or higher. 2 This limit is based on a guideline released in 2003, as seen in the table below.
- Other health care professionals diagnose patients with high blood pressure if their blood pressure is consistently 130/80 mm Hg or higher. 1 This limit is based on a guideline released in 2017, as seen in the table below.
Blood pressure levels according to The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (2003 Guideline) 2
systolic: less than 120 mm Hg diastolic: less than 80 mm Hg
At risk (prehypertension)
systolic: 120–139 mm Hg diastolic: 80–89 mm Hg
High blood pressure (hypertension)
systolic: 140 mm Hg or higher diastolic: 90 mm Hg or higher
Blood pressure levels according to The American College of Cardiology/American Heart Association Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (2017 Guideline) 1
systolic: 120–129 mm Hg diastolic: less than 80 mm Hg
systolic: 130 mm Hg or higher diastolic: 80 mm Hg or higher
If you are diagnosed with high blood pressure, talk with your health care team about your blood pressure levels and how these levels affect your treatment plan.
Signs and symptoms
High blood pressure usually has no warning signs or symptoms, and many people do not know they have it. Measuring your blood pressure is the only way to know whether you have high blood pressure.
High blood pressure usually develops over time. It can happen because of unhealthy lifestyle choices, such as not getting enough regular physical activity. Certain health conditions , such as diabetes and having obesity, can also increase the risk for developing high blood pressure. High blood pressure can also happen during pregnancy .
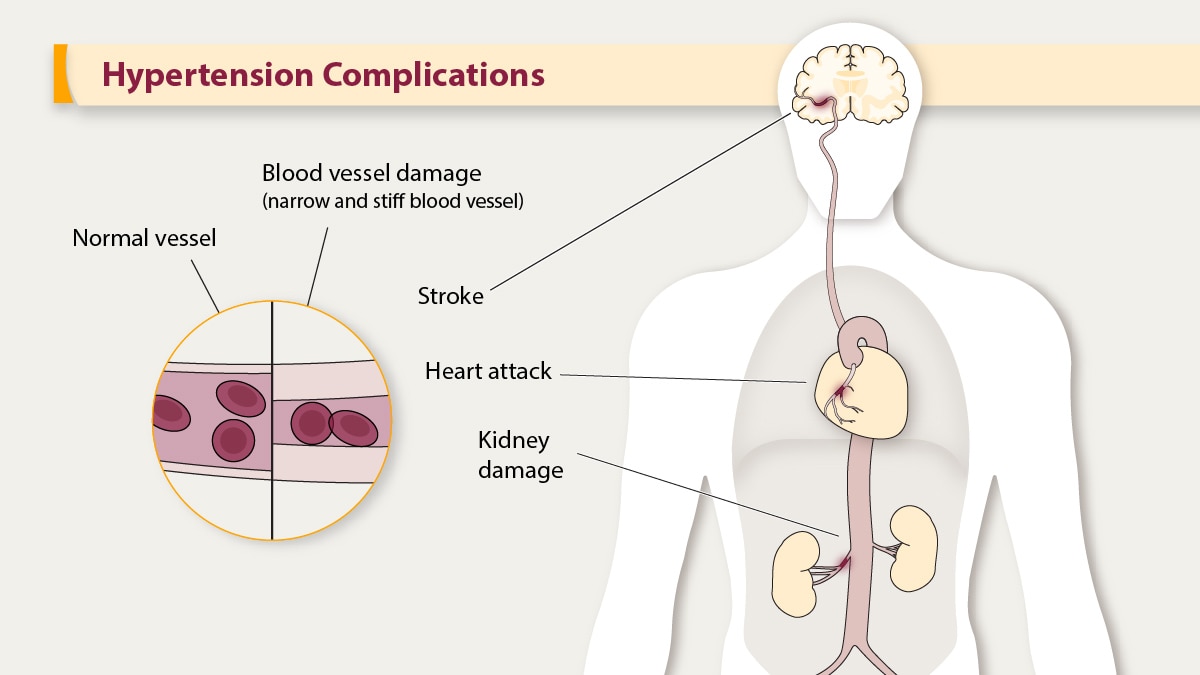
Potential problems having high blood pressure could casue
High blood pressure can damage your health in many ways. It can seriously hurt important organs like your heart, brain, kidneys, and eyes.
The good news is that, in most cases, you can manage your blood pressure to lower your risk for serious health problems.
Heart attack and heart disease
High blood pressure can damage your arteries by making them less elastic. This decreases the flow of blood and oxygen to your heart and leads to heart disease . In addition, decreased blood flow to the heart can cause:
- Chest pain, also called angina.
- Heart attack , which happens when the blood supply to your heart is blocked and heart muscle begins to die without enough oxygen. The longer the blood flow is blocked, the greater the damage to the heart.
- Heart failure , a condition that means your heart can't pump enough blood and oxygen to your other organs.
Stroke and brain problems
High blood pressure can cause the arteries that supply blood and oxygen to the brain to burst or be blocked, causing a stroke . Brain cells die during a stroke because they do not get enough oxygen. Stroke can cause serious disabilities in speech, movement, and other basic activities. A stroke can cause death.
Having high blood pressure, especially in midlife, is linked to having poorer cognitive function and dementia later in life. Learn more about the link between high blood pressure and dementia from the National Institutes of Health's Mind Your Risks ® campaign.
Kidney disease
Adults with diabetes, high blood pressure, or both have a higher risk of developing chronic kidney disease than those without these conditions.
Many people with high blood pressure can lower their blood pressure into a healthy range or keep their numbers in a healthy range by making lifestyle changes . Talk with your health care team about:
- Physical activity each week (about 30 minutes a day, 5 days a week)
- Not smoking
- Eating a healthy diet, including limiting sodium (salt) and alcohol
- Keeping a healthy weight
- Managing stress
Learn more about ways to manage and prevent high blood pressure.
In addition to making positive lifestyle changes, some people with high blood pressure need to take medicine to manage their blood pressure.
Talk with your health care team right away if:
- You think you have high blood pressure.
- If you've been told you have high blood pressure but do not have it under control.
By taking action to lower your blood pressure, you can help protect yourself against heart disease and stroke, also called cardiovascular disease (CVD).
- Whelton PK, Carey RM, Aronow, WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol . 2018;71(19):e127–e248.
- National High Blood Pressure Education Program. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure [PDF – 223K] . National Heart, Lung, and Blood Institute; 2003.
High Blood Pressure
High blood pressure increases the risk for heart disease and stroke, two leading causes of death for Americans.
For Everyone
Health care providers, public health.
- English English
- தமிழ் தமிழ்
- বাংলা বাংলা
- മലയാളം മലയാളം
- ગુજરાતી ગુજરાતી
- हिंदी हिंदी
- मराठी मराठी
- Business Business
- बिज़नेस बिज़नेस
- Insurance Insurance
The Financial Express
- RCB vs CSK Live Score
- Share Market Live
- Q4 Results 2024
- JEE Advanced 2024 Admit Card
- Mutual Funds
- Stock Market Stats
- Gold Rate Today
- Top Indices Performance
- Brandwagon Summit 2024
- Loksabha Election
- Budget 2024
- Stock Market Quotes
- Mutual Fund
- Stock Stats
- Top Gainers
- CaFE Invest
- Investing Abroad
- Gold Rate in India
- Silver Rate in India
- Petrol Rate in India
- Diesel Rate in India
- Express Mobility
- Banking & Finance
- Travel & Tourism
- Brand Wagon
- Entertainment
- Web Stories
- Auto Web Stories
- Infographics
- Today’s Paper
- International
- Edits & Columns
- Personal Finance Print
- PRIVACY POLICY
- TERMS AND CONDITIONS

World Hypertension Day 2024: Is hypertension curable? Experts answer
World hypertension day 2024: hypertension, often dubbed the “silent killer,” is a chronic medical condition where the blood pressure in the arteries is persistently elevated..

World Hypertension Day 2024: Hypertension is an extremely common condition and if not treated at the right time it can lead to serious complications. Every year, May 17 is observed as World Hypertension Day to raise awareness about this disease and its impact.
According to Prof. (Dr) D. Prabhakaran, MD, DM (Cardiology), MSc, FRCP, FNA, DSc (Honoris Causa).- Executive Director, Centre for Chronic Disease Control, India ’s young population, comprising 65% of those under 35, promises to propel the nation to the ranks of the world’s top economies by FY’28.

“However, amid this optimism lies a harsh trend – 27 million young adults grapple with hypertension, posing a formidable health challenge. Not only does hypertension account for a significant portion (40-45%) of CVD-related deaths, but it also escalates the risk of premature mortality and disability. Urgent collaborative action across various stakeholders is imperative to prioritize hypertension treatment through primary healthcare. Such efforts not only safeguard lives but can also shield India from an estimated economic loss of approximately $2.7 trillion by 2030 due to CVDs,” Dr. Prabhakaran said.

Dr. Manoj A. G, Consultant Physician on Practo told Financial Express.com that hypertension, often dubbed the “silent killer,” is a chronic medical condition where the blood pressure in the arteries is persistently elevated.
“Symptoms of hypertension are often subtle and can include headaches, shortness of breath, dizziness, chest pain, and nosebleeds, although many people experience no symptoms at all. Key risk factors for developing hypertension include a family history of high blood pressure, age (the risk increases as you get older), obesity, a sedentary lifestyle , tobacco use, excessive salt consumption, alcohol abuse, and chronic stress. Additionally, certain underlying conditions like diabetes and kidney disease can also elevate the risk,” Dr. Manoj said.
The hidden dangers of hypertension are significant. Uncontrolled high blood pressure can lead to serious health complications such as heart disease, stroke, kidney damage, and vision loss. It can also cause damage to the arteries, leading to atherosclerosis, which further increases the risk of cardiovascular diseases, he said.
“Given these risks, the importance of monitoring and managing high blood pressure cannot be overstated. Regular blood pressure checks help in early detection and timely intervention, reducing the risk of adverse health outcomes. Lifestyle modifications like the DASH diet, restricting salt intake, regular physical activity, quitting smoking, and limiting alcohol intake, alongside prescribed medications, can effectively manage and control high blood pressure,” he told Financial Express.com.
Lifestyle changes can help lower high blood pressure and can help anyone with hypertension. But is it curable?
According to most major guidelines, it is recommended that hypertension be diagnosed when a person’s systolic blood pressure (SBP) in the office or clinic is ≥140 mm Hg and/or their diastolic blood pressure (DBP) is ≥90 mm Hg following repeated examination.
“People older than 40 years old should have their blood pressure checked one time a year. The ages between 18 and 40 years old should get their blood pressure checked every three to five years unless they fall into the high-risk category,” Dr. Tushar Tayal, Lead Consultant, Department of Internal Medicine, CK Birla Hospital, Gurugram told Financial Express.com.
Hypertension is primarily a lifestyle disorder along with diabetes, obesity and metabolic syndrome. Genes likely play some role in high blood pressure and people with a family history of high blood pressure likely share common environments and other potential factors that increase their risk. Even if there are hereditary factors, the majority of the time BP can be kept under control with lifestyle measures.
These include:
- Reduced salt intake – salt intake in a hypertensive should be less than 2.5 gm per day or 1/2 teaspoon in the entire day
- High potassium diet – Ensure intake of 2 fruits and 3 vegetables every day which are rich in potassium which has a BP lowering effect
- Exercise – 30 min of daily exercise inclusive of cardio and strength training will keep BP under control
- Pranayam/yoga – 30 min of breathing exercise and meditation will reduce stress hormones and help in reducing BP
- Sleep – 7 hrs of sleep daily is essential for maintaining immunity and healthy body functions
- Optimal body weight – obesity itself is a risk factor for hypertension and losing excess body weight helps in bringing down the blood pressure.
“It is important to check BP and keep it under control ( with or without medication ) because Undiagnosed hypertension is a risk factor for stroke, heart attack, kidney damage, and eye damage. Hypertension is a Controllable disease and with proper lifestyle measures, BP can be kept in optimal range for prolonged periods,” Dr. Tayal said.
Is hypertension curable?
Hypertension, commonly known as high blood pressure, is a prevalent health issue affecting millions worldwide. According to Dr. Nishith Chandra – Principal Director, Interventional Cardiology, Fortis Escorts Heart Institute, Okhla Road, New Delhi, while it’s not typically “curable” in the traditional sense, it can be effectively managed and controlled through lifestyle changes and, in some cases, medication.
“Healthy lifestyle modifications play a crucial role in managing hypertension. This includes maintaining a balanced diet low in sodium, saturated fats, and cholesterol, while high in fruits, vegetables, and whole grains. Regular exercise, such as brisk walking or swimming, can also help lower blood pressure,” Dr. Chandra said.
Additionally, managing stress levels through relaxation techniques like meditation or deep breathing exercises can contribute to overall blood pressure control. Avoiding tobacco and limiting alcohol consumption are also essential factors in hypertension management.
He also informed that for some individuals with hypertension, medication may be necessary to control their blood pressure effectively. These medications work by targeting different mechanisms in the body to reduce blood pressure levels, he said.
“It’s important to note that while hypertension may not be “curable” in the traditional sense, effective management can significantly reduce the risk of complications such as heart disease, stroke, and kidney damage. Regular monitoring of blood pressure levels and working closely with healthcare professionals are essential for maintaining optimal health outcomes,” he said.
‘There is no permanent cure for high blood pressure’
High blood pressure is typically symptomless, which quietly damages the blood vessels and ultimately leads to serious health problems like stroke, heart attacks renal failure, etc.
“Although there is no permanent cure for high blood pressure, In some rare cases there are reversible causes of hypertension such as renal artery stenosis and also some rare tumors which can be treated to reverse hypertension,” Dr. Ashwani Mehta, Senior Consultant cardiologist, Sir Ganga Ram Hospital, New Delhi told Financial Express.com.
Also treating obstructive sleep apnea syndrome, where patients typically snore at night and have day time drowsiness can help patients in controlling the blood pressure, Dr. Mehta said.
The advantages of blood pressure medications are evident: They maintain blood pressure within healthy ranges, significantly diminishing the risk of heart disease, heart attack, and stroke.
“Generally, the risks associated with these medications are minimal. While typically requiring lifelong adherence, certain individuals can decrease or discontinue their usage by addressing modifiable factors contributing to high blood pressure (hypertension),” he highlighted.
Patients need to take the lifestyle changes that matter and take BP-lowering medications regularly as prescribed by their physicians.
“Certain healthy lifestyle changes, such as a low sodium diet and regular exercise which includes a daily walk of about 10,000 steps or physical activity of at least 150 minutes a week in the form of moderate-intensity aerobic activity, such as brisk walking, swimming, or sports can help. Another change that can reduce blood pressure are limiting alcohol. Managing stress and controlling weight and smoking can also reduce the risk associated with high blood pressure,” Dr. Mehta said.
Get live Share Market updates, Stock Market Quotes , and the latest India News and business news on Financial Express. Download the Financial Express App for the latest finance news.
Related News
An Air India Express flight made an emergency landing in Bengaluru after one of its engines caught fire. No injuries were reported as all passengers and crew were safely evacuated. The fire was extinguished upon landing and a full-scale emergency was declared. The flight was en route Kochi. An investigation will be conducted to determine the cause.
Photo Gallery
7 Kashmir: Freshly harvested strawberries! First fruit of the season is here – PHOTOS
5 RCB vs CSK Knockout: El Classico of IPL – In Photos
8 Uttarakhand: Here’s a glimpse of this year’s Char Dham yatra – PHOTOS
Latest News

Kinara Capital FY24 results: 9th consecutive year of profitability; PAT jumps 51%

Fintech firm Zeta launches UPI-linked digital credit service for banks | Here’s how this will work

Supreme Court deals major blow to bank employees! Interest-free loans declared ‘fringe benefits’, liable to be taxed

Loan transfer might cost you MORE than you think! Find out how to avoid hidden charges and save big

Banks deployed Rs 24.6 lakh crore credit to MSMEs in March: RBI data
Trending topics.
- IPO’s Open and Upcoming 5
- Stock Analysis
- Financial Literacy
- NSE Top Gainers 1780
- NSE Top Losers 693
- BSE Top Gainers 2767
- BSE Top Losers 1271
- NSE 52-Week High 0
- NSE 52-Week Low 0
- BSE 52-Week High 0
- BSE 52-Week Low 0
- NSE Price Shocker
- NSE Volume Shocker
- BSE Price Shocker
- BSE Volume Shocker
- NSE Sellers
- BSE Sellers
- Silver Rate Today
- Petrol Rate Today
- Diesel Rate Today
Students hope to share ‘Major’ joy of therapy dog with look-a-like plushes for all
FLASHER, N.D. ( KFYR /Gray News) - It’s no secret that students at Flasher High School love therapy K-9 Major Teddy Hugz when he comes to visit.
“When Tommy will let him go, and he’ll just run to a student or a specific teacher or room that he is familiar with and just kind of enlightens the whole school,” said freshman Brenna Eckroth.
However, the school’s resource officer and Major’s handler Deputy Tommy can’t be in all of the schools he serves at once.
That’s when an idea came to high school students Carrie, Ellie, and Brenna.
“We love Tommy, so it was fun to give back to what he has done for us,” said freshman Carrie LaDuke.
Through their FCCLA Club, they made puppy chow, and all the proceeds went to buying stuffed animals that look like their favorite classmate.

“Because it’s nice for the little kids to have someone here when Major is not here, that they can go to as a companion,” said sophomore Ellie Skretteberg.
They had enough money to give one to all the elementary school classrooms, the special education room, the library, and the music room. Deputy Tommy even received two to give to crime victims.
“It’s really satisfying knowing they have a part of Major and our agency to help through the day,” said Deputy Tommy.
The story doesn’t end there. Flasher’s Masonic Lodge heard about the initiative and also wanted to give back to a community that has helped them before.
“[We did it] because a couple of years ago, we needed shingles replaced on our lodge and we really didn’t have the money to do it. But through the community organizations and members of the community, we were able to do it,” said Alan Malm of the Masonic Lodge.
The Masonic Lodge bought all of the remaining dogs from Amazon to give to Deputy Tommy.
“It feels so great that more people love what we did and want to contribute to it,” said Ellie.
“I think we were surprised how expanded here and how far it has gone from our school. It just means more,” said Brenna.
Carrie, Ellie and Brenna say they can see the difference it’s made in Flasher.
“They also loved naming him. That was a big thing for them all to figure out what they were going to name their dogs. I heard really good feedback from it,” said Ellie.
Now the new dogs will go to students in New Salem.
“Major’s role in helping people and being able to do this and continue helping people is pretty awesome,” said Deputy Tommy.
The girls say they hope these dogs will help spread a positive message to make a “Major” difference in schools around the state.
Copyright 2024 KFYR via Gray Media Group, Inc. All rights reserved.

Man injured in north Laredo shooting dies from injuries, five people charged with murder

Update: 32-year-old man hospitalized following head-on collision in north Laredo

Structure fire breaks out in Laredo

Rep. Henry Cuellar’s staff leaves following indictment sources say

Border Patrol officials with ties to Laredo entrepreneur under investigation by federal agency
Latest news.

Biden will deliver Morehouse commencement address during a time of tumult on US college campuses

University’s beloved campus cat earns honorary doctorate in ‘litter-ature’

University's graduating class includes cat with honorary degree in 'litter-ature'

19-year-old finds silver lining after losing his arm in construction accident

19-year-old construction worker back on the job after losing his arm to accident
We use cookies to collect and analyse information on our site's performance and to enable the site to function. Cookies also allow us and our partners to show you relevant ads when you visit our site and other 3rd party websites, including social networks. You can choose to allow all cookies by clicking 'Allow all', or manage them individually by clicking 'Manage cookie preferences', where you will also find more information.
- Press releases
- bp expands mobility and convenience network completing the purchase of leading travel center operator, TravelCenters of America
bp-expands-mobility-and-convenience-network-completing-the-purchase-of-leading-travel-center-operator-travelcenters-of-america
- Adds a network of around 280 travel centers, strategically located on major highways across US; complementing bp’s US convenience and mobility business.
- Almost doubles bp’s global convenience gross margin.
- Brings growth opportunities for four of bp’s five transition growth engines including EV charging via bp pulse, convenience, biofuels/renewable natural gas (RNG) and, later, hydrogen.
- Adds EBITDA immediately, expected to grow to around $800m by 2025, underpinned by investment, integration value and synergies.

Today BP Products North America Inc., a wholly owned indirect subsidiary of BP p.l.c. (NYSE: bp), completed its $1.3 billion acquisition of TravelCenters of America Inc. (Nasdaq: TA), one of the country’s leading full-service travel center operators, marking a milestone for the US in the growth of bp’s strategic convenience and mobility business and welcoming thousands of additional employees into bp.
“We are thrilled to welcome the TravelCenters of America team to bp and give a turbo-boost to our convenience and mobility business in the US. Combining TA’s sites on US highways with our brilliant retail network off the highway immediately expands our offer and doubles our global convenience gross margin.”
“By integrating bp pulse, our fast-growing EV charging business, along with biofuels and renewable natural gas businesses – and in time, hydrogen – we can help America’s vital fleets and logistics companies decarbonize.”
Emma Delaney, executive vice president customers & products, bp
In February, bp announced it had agreed to acquire TA, subject to required approvals. Having received those approvals and with the transaction complete, TA’s strategically located network of highway sites complements bp’s existing predominantly off-highway convenience and mobility business in the US, enabling TA and bp to offer fleets and consumers a seamless nationwide service.
The transaction will provide options to expand and continue to develop convenience and mobility offers through four of bp’s five transition growth engines:
- EV charging
- convenience.
Convenience is one of five strategic transition growth engines that bp intends to grow rapidly through this decade. By 2030, bp aims for around half its annual investment to go into these transition growth engines; with around half of its anticipated cumulative $55-65 billion transition growth engine investment going into convenience, bioenergy and EV charging.
With the close of the acquisition, TravelCenters of America common shares have been converted into the right to receive $86 per share.
Additional information on the acquisition can be found in the agreement announcement .
Further information
bp press office, London: +44 7831 095541, +44 7919 217511, [email protected]
bp US press office: [email protected]
Cautionary statement
In order to utilize the ‘safe harbor’ provisions of the United States Private Securities Litigation Reform Act of 1995 (the ‘PSLRA’) and the general doctrine of cautionary statements, bp is providing the following cautionary statement.
This document contains certain forecasts, projections and forward-looking statements – that is, statements related to future, not past events and circumstances – with respect to the financial condition, results of operations and businesses of bp and certain of the plans and objectives of bp with respect to these items. These statements are generally, but not always, identified by the use of words such as ‘will’, ‘expects’, ‘is expected to’, ‘targets’, ‘aims’, ‘should’, ‘may’, ‘objective’, ‘is likely to’, ‘intends’, ‘believes’, ‘anticipates’, ‘plans’, ‘we see’ or similar expressions. By their nature, forward-looking statements involve risk and uncertainty because they relate to events and depend on circumstances that will or may occur in the future and are outside the control of bp. Actual results or outcomes, may differ materially from those expressed in such statements, depending on a variety of factors, including the risk factors discussed under “Risk factors” in bp’s Annual Report and Form 20-F 2022 as filed with the US Securities and Exchange Commission and in any of our more recent public reports.
Our most recent Annual Report and Form 20-F and other period filings are available on our website at www.bp.com or can be obtained from the SEC by calling 1-800-SEC-0330 or on its website at www.sec.gov .

VIDEO
COMMENTS
Air travel when you have high blood pressure could lead to certain complications. Understand the risks, and learn some tips to help you have a safe flight. ... Systemic hypertension at high ...
Summary. For most people, it is safe to fly with high blood pressure, but it is a good idea to consult a doctor before traveling. A person may have to carry their medication and move around as ...
The effects of high altitude may include nausea and headaches. However, the pressurization of airplane cabins usually prevents these uncomfortable side effects. Flying with high blood pressure is possible if high blood pressure is under control. Nonetheless, anyone with high blood pressure should take the necessary precautions for air travel.
RESPeRATE is the only non-drug, FDA-Cleared device for lowering blood pressure naturally. It is clinically proven, doctor recommended and has no side effects. RESPeRATE lowers blood pressure by relaxing constricted blood vessels which cause high blood pressure. RESPeRATE does so by harnessing the therapeutic power of slow-paced breathing with ...
Smoking. Not exercising enough. Drinking too much alcohol, coffee or other caffeine-based drinks. Eating too much salt and too few fruits and vegetables. Not getting enough sleep, or having poor quality sleep. Having a relative with high blood pressure. Aged over 65. Being of black African or black Caribbean descent.
Sitting immobile on long plane flights or car, train or bus rides can slightly increase a normal person's risk of blood clots in the legs, but associated medical issues usually contribute to it. If someone has peripheral artery disease (PAD) or a history of heart failure, the clot risk increases. Recent surgery, older age and catheters in a ...
At these heights, your blood works harder to deliver oxygen, causing blood pressure to rise. Therefore, when planning your trip, you may want to avoid destinations like: Colombia. China. Mexico. Peru. However, if you already booked your trip, don't panic: managing your blood pressure at high altitudes is possible.
The management of hypertension should be considered, both for the passengers and the flight crew. The main pathophysiological factor during a flight is altitude related decrease in oxygen saturation. Commercial airplanes fly at 30,000-40,000 feet (corresponding to 9,000-12,000 m) above the sea level.
Air travel is generally safe for heart patients, with appropriate precautions. If you have heart disease, you can fly safely as a passenger on an airplane, but you need to be aware of your risks and take necessary precautions. Heart conditions that can lead to health emergencies when flying include coronary artery disease (CAD), cardiac ...
Read this guide for up-to-date information and top tips for travelling with high-pressure. Freephone to get your quote on: Call Free 0800 848 8608. or. ... Before travelling with high blood pressure. Before you fly, consider visiting your doctor to discuss your travel plans - particularly if your blood pressure is unstable. ...
If you need to travel by plane, there are special issues you must deal with if you have high blood pressure. First, you must not count on being served low-salt food on the plane, though on many flights, you might be fed a meal or snack that includes an undressed salad or crudités. But while bringing your own food onto the plane is a good idea ...
High blood pressure, or hypertension, afflicts about 75 million people each year, according to the American Heart Association. With 195 million people flying domestically, according to Bureau of ...
Nine tips for traveling with high blood pressure. 1. Get to the airport early. Leave yourself plenty of time to check your bag, go through security, and get to your gate early. If you're stressed out about missing your flight, this can raise your blood pressure. 2.
Likewise, people with difficult-to-control blood pressure, or those visiting high-altitude areas for long periods of time, may need to carefully monitor blood pressure levels for any changes. Sudden cardiac death is the most frequent non-traumatic cause of death at altitude, according to the statement.
Remember to pack extra medicines to cover for any delays or loss. Bring your own food as airlines tend to provide snacks with added salt which can increase blood pressure levels. Avoid alcohol and any medication with a sedative effect - they can make you less active during a flight. Drink plenty of water.
Yes, you should. Medication for high blood pressure is usually taken daily, and when travelling make sure you have enough medication to last for the duration of your trip. It is a good idea to take a copy of your prescription with you, in case your medication gets lost and you need to get some more from a local chemist or doctor.
A. If you have high blood pressure but are otherwise healthy, your blood pressure is under control, and you take some precautions, a trip to the Rocky Mountains should be fine. To continue reading this article, you must log in.
Less than 120 over 80: Your blood pressure is normal. Between 120 over 80 and 140 over 90: Your blood pressure is higher than normal. 140 over 90 or higher: You have high blood pressure. You should consult your GP. If your blood pressure is higher than 120 over 80, seek medical advice before you travel.
Include contact information for your doctor. Most pulmonary hypertension medications come from a specialty pharmacy. Carry a card with the phone number of your specialty pharmacy in case you lose ...
Travel to high altitude locations that are >2,500 m above sea level triggers physiological acclimatization processes within the cardiocirculatory and pulmonary ... and high blood pressure 82,83 ...
There is no contraindication to air travel for patients with treated hypertension, as long as it is under satisfactory control and the patient is reminded to carry their medication with them on the flight. Uncontrolled hypertension is a contraindication to fly. Reference: 1) Civil Aviation Authority. Fitness to Fly (Accessed 1/8/19)
Likewise, people with difficult-to-control blood pressure, or those visiting high-altitude areas for long periods of time, may need to carefully monitor blood pressure levels for any changes. Sudden cardiac death is the most frequent non-traumatic cause of death at altitude, according to the statement.
High blood pressure can cause the arteries that supply blood and oxygen to the brain to burst or be blocked, causing a stroke. Brain cells die during a stroke because they do not get enough oxygen. Stroke can cause serious disabilities in speech, movement, and other basic activities. A stroke can cause death.
It empties your energy tank. Air pressure is lower at higher altitudes, which means your body takes in less oxygen. Airlines "pressurize" the air in the cabin, but not to sea-level pressures ...
World Hypertension Day 2024: Hypertension, often dubbed the "silent killer," is a chronic medical condition where the blood pressure in the arteries is persistently elevated.
FLASHER, N.D. (KFYR/Gray News) - It's no secret that students at Flasher High School love therapy K-9 Major Teddy Hugz when he comes to visit."When Tommy will let him go, and he'll just run ...
Today BP Products North America Inc., a wholly owned indirect subsidiary of BP p.l.c. (NYSE: bp), completed its $1.3 billion acquisition of TravelCenters of America Inc. (Nasdaq: TA), one of the country's leading full-service travel center operators, marking a milestone for the US in the growth of bp's strategic convenience and mobility business and welcoming thousands of additional ...