- Newsletters
- FAC Articles


Find-A-Code Articles, Published 2021, September 28
When is it proper to bill nurse visits using 99211.
by Christine Woolstenhulme, QMC QCC CMCS CPC CMRS Sep 28th, 2021 - Reviewed/Updated Aug 29th
When vaccines or injections are given in the office, coding can often get confusing; for example, is it correct to report a nurse visit using 99211 and an E/M office visit reporting 99202 ‑ 99215 and include injection fees with the vaccine product? In addition, the reporting of evaluation and management (E/M) during the same visit where vaccines are administered is not always understood. The answer depends on whether the provider performs a medically necessary and significant, separately identifiable E/M visit, in addition to the immunization administration.
CMS states, when a separately identifiable E/M service (which meets a higher complexity level than CPT code 99211 ) is performed, in addition to drug administration services, you should report the appropriate E/M CPT code reported with modifier -25. Documentation should support the level of E/M service billed. For an E/M service provided on the same day, a different diagnosis is not required.
It is incorrect to bill a 99211 when the provider provides an E/M service that meets a higher complexity level than CPT code 99211 , you must bill the higher complexity, and you cannot bill for two services in one day.
Charging for Nurse Visits
There are times when it is appropriate to report for a nurse visit using CPT code 99211 . The Incident-to rule applies when reporting this code, and services provided must be documented as medically necessary services, including the clinical history, clinical exam, making a clinical decision, and physician supervision.
- NOTE: A nurse visit is not paid if billed with a drug administration service such as chemotherapy or non-chemotherapy drug infusion code, including therapeutic or diagnostic injection codes. The reasoning is because diagnostic IV infusion or injection services typically require direct physician supervision, and using 99211 is reported by qualified healthcare professionals other than physicians.
08/29/2023 NOTE: (These CPT codes,90782, 90783, 90784, or 90788 were deleted in 2006, but still showing in CMS - Claims processing manual) When reporting CPT codes 90782, 90783, 90784, or 90788 , CPT code 99211 cannot be reported. In addition, it is improper billing to report a visit solely for an injection that meets the definition of the injection codes.
When the only reason for the visit is for the patient to receive an injection, payment may be made only for the injection (if it is covered). An office visit using 99211 would not be warranted where the services rendered did not constitute a regular office visit and a part of the plan of care and not at the patient's request.
Unlike other E/M codes 99202 - 99205 , and 99212 - 99215 , time alone cannot be used when reporting 99211 when selecting the appropriate code level for E/M services. Effective January 1, 2021, time was removed as an available code-selection criterion. The typical time spent on this code is five minutes.
Other visits billed with 99211
Several other visits may be reported using 99211 , and nurses are not the only staff that can report this code; medical Assistants and technicians are also included under non-physician.
Covid-19 Testing
According to CMS ; Physician offices can use CPT code 99211 when office clinical staff furnish assessment of symptoms and specimen collection for Covid-19 incident to the billing professionals services for both new and established patients. When the specimen collection is performed as part of another service or procedure, such as a higher-level visit furnished by the billing practitioner, that higher-level visit code should be billed. The specimen collection would not be separately payable.
Examples from CMS
The following are examples of when CPT 99211 might be used:
- Office visit for an established patient for blood pressure check and medication monitoring and advice. History, blood pressure recording, medications, and advice are documented, and the record establishes the necessity for the patient's visit.
- Office visit for an established patient for return to work certificate and advice (if allowed to be by other than the physician). Exam and recommendation are noted, and the Return to Work Certificate is completed, copied, and placed in the record.
- Office visit for an established patient on regular immunotherapy who developed wheezing, rash, and swollen arm after the last injection. Possible dose adjustments are discussed with the physician, and an injection is given. History, exam, dosage, and follow-up instructions are recorded.
- Office visit for an established patient's periodic methotrexate injection. Monitoring Lab tests, query signs and symptoms, obtain vital signs, repeat testing, and injection advised. All this information is recorded and reviewed by the physician. (Note that in this circumstance, if 99211 is billed, the injection code is not separately billable). An office visit for an established patient with a new or concerning bruise is checked by the nurse (whether or not the patient is taking anticoagulants), and the patient is advised on how to care for the bruise and what to be concerned about, and, if on anticoagulants, continuing or changing current dosage is advised. History, exam, dosage, and instructions are recorded and reviewed by the physician.
- Office visit for an established patient with atrial fibrillation who is taking anticoagulants and has no complaints . The patient is queried by the nurse, vital signs are obtained, the patient is observed for bruises and other problems, the prothrombin time is obtained, the physician is advised of prothrombin time and medication dose, and medication is continued at present dose with follow up prothrombin time in one month recommended. History, vital signs, exam, prothrombin time, INR, dosage, physician's decision, and follow-up instructions are recorded.
References/Resources
About christine woolstenhulme, qmc qcc cmcs cpc cmrs.
Christine Woolstenhulme, CPC, QCC, CMCS, CMRS, is a Certified coder and Medical Biller currently employed with Find-A-Code. Bringing over 30 years of insight, business knowledge, and innovation to the healthcare industry. Establishing a successful Medical Billing Company from 1994 to 2015, during this time, Christine has had the opportunity to learn all aspects of revenue cycle management while working with independent practitioners and in clinic settings. Christine was a VAR for AltaPoint EHR software sales, along with management positions and medical practice consulting. Understanding the complete patient engagement cycle and developing efficient processes to coordinate teams ensuring best practice standards in healthcare. Working with payers on coding and interpreting ACA policies according to state benchmarks and insurance filings and implementing company procedures and policies to coordinate teams and payer benefits.
When is it Proper to Bill Nurse Visits using 99211. (2021, September 28). Find-A-Code Articles. Retrieved from https://www.findacode.com/articles/nurse-visits-and-injections-36866.html
Article Tags (click on a tag to see related articles)
Thank you for choosing Find-A-Code, please Sign In to remove ads.


Are You Happy With Your Practice Collections ?
Holiday offers for you, helping physician groups to stay profitable.
Contact us today!
Streamline Legacy Accounts Receivable Resolution
Contact Now
Recover your $ which you have left on the table
Request a Quote now
2022 Coding Update for CPT 99211
While code descriptors are never big news, one key change to a low-level office/outpatient (E/M) service code descriptor that came into effect on January 1, 2022, could be a welcome change for your practice. The revision is the level one office/outpatient E/M code for established patients. In 2022, CPT 99211 descriptor reads as, office or other outpatient visits for the evaluation and management of an established patient that may not require the presence of a physician or other qualified health care professional. While the 2021 descriptor was, office or other outpatient visits for the evaluation and management of an established patient, that may not require the presence of a physician or other qualified health care professional. Usually, the presenting problem(s) are minimal.
The phrase ‘Usually, the presenting problem(s) are minimal’ has been deleted to bring the descriptor for CPT 99211 more in line with the rest of the office/outpatient evaluation and management (E/M) codes. With the phrase removal, 99211’s descriptor is now more synched with the other office/outpatient E/Ms: 99202 through 99215. This change eliminates a source of confusion as to what is a minimal problem and what is not. Even with the change, CPT 99211 still represents an E/M service provided by clinical staff as opposed to a physician or other qualified healthcare professional who may report higher levels of E/M services. Services described by 99211 must be medically necessary (i.e., clinically indicated) and be part of a plan of care by a physician or other qualified healthcare professional. This is why 99211 is not reportable for providing a service at a patient’s request rather than as part of an established plan of care.
Basic Guidelines for CPT 99211
The following guidelines can help you decide whether a service qualifies for 99211:
- The patient must be established. CPT 99211 cannot be reported for services provided to patients who are new to the physician.
- An E/M service must be provided. Generally, this means that the patient’s history is reviewed, a limited physical assessment is performed or some degree of decision-making occurs. 99211 would not be appropriate when a patient comes into the office just to pick up a routine prescription.
- Keep in mind that if another CPT code more accurately describes the service being provided, that code should be reported instead of 99211. For example, if a physician instructs a patient to come to the office to have blood drawn for routine labs, the nurse or lab technician should report CPT code 36415 (routine venipuncture) instead of 99211 since an E/M service was not required.
- The service must be separate from other services performed on the same day. For example, if a nurse provides instructions following a physician’s minor procedure or takes a patient’s vital signs prior to an encounter with the physician, 99211 should not be reported for these activities because they are considered part of the E/M service already being provided by the physician.
- The presence of a physician is not always required. Although physicians can report 99211, CPT’s intent with the code is to provide a mechanism to report services rendered by other individuals in the practice (such as a nurse or other clinical staff member). According to CPT, the staff member may communicate with the physician, but direct intervention by the physician is not required.
- Medicare’s requirements on this point are slightly different: While the physician’s presence is not required at every 99211 services involving a Medicare patient, the physician must have initiated the service as part of a continuing plan of care in which he or she will be an ongoing participant. For some insurance carriers, this means that the physician must see the patient at least every third visit. In addition, the physician must at least be in the office suite when each service is provided.
- No key components are required. Unlike other office visit E/M codes, such as 99212, which require at least two of three key components (problem-focused history, problem-focused examination, and straightforward medical decision making), the documentation of a 99211 visit does not have any specific key-component requirements. Rather, the note just needs to include sufficient information to support the reason for the encounter and E/M service and any relevant history, physical assessment, and plan of care. The date of service and the identity of the person providing the care should be noted along with any interaction with the supervising physician.
Improve Collections with CPT
Reporting CPT 99211 can bring additional revenue into your practice. Specific payment amounts will vary by payer, but the average unadjusted 2021 payment from Medicare for a 99211 service was $23.03. This means that only five 99211 encounters with Medicare patients in a week will result in over $5,000 per year for practice. Although this may not sound like a lot of money, it is easy revenue. Most practices already provide a number of 99211 services but fail to capture those charges. Remember, all services have a cost associated with them, and practices need to recoup as much of these costs as is legitimately possible. As mentioned above, physicians can report 99211, but it is intended to report services rendered by other individuals in the practice, such as a nurse or other staff member. Appropriately reporting 99211 services can also improve documentation in a practice. Staff members who are cognizant of billing guidelines tend to pay increased attention to documentation, which, in turn, can result in a more useful medical record for all providers involved in the care of the patient.
MedicalBillersandCoders (MBC) is a leading medical billing company providing complete revenue cycle solutions. We keep on sharing billing and coding updates as per various medical specialties. We hope you have received updated information to use CPT 99211 accurately. If you need any help in medical billing and coding for your practice, contact us at [email protected] / 888-357-3226
REQUEST A CALL BACK
Are you looking for more than one billing quotes?

Using and Documenting CPT Code 99211 Services Correctly

Popular Tasks
- Find a seminar or webinar
- Claims information
- View provider manual
- Clinical guidelines
- Provider portal
Neighborhood Care
- Cambria Heights
- East New York
- See All Locations
Using and Documenting CPT Code 99211 Services Correctly
CPT ® code 99211 is defined by the 2011 CPT Standard Edition manual as:
" Office or other outpatient visit for the evaluation and management of an established patient that may not require the presence of a physician. Usually, the presenting problem(s) are minimal. Typically, 5 minutes are spent performing or supervising these services."
Using code 99211 to report a low-level evaluation and management (E/M) service Code 99211 describes a face-to-face encounter with a patient consisting of elements of both evaluation (requiring documentation of a clinically relevant and necessary exchange of information) and management (providing patient care that influences, for example, medical decision making or patient education). Documentation must be legible and include the identity and credentials of the servicing provider.
Using code 99211 to bill an 'incident to' service When Code 99211 is billed as an “incident to” service, the physician’s service may be performed by ancillary staff and billed as if the physician personally performed the service. Documentation should include the identity and credentials of the supervising physician and the staff that provided the service. Notes should indicate the degree of the physician’s involvement and document the link between the services of the two providers.
All 99211 services that don’t document or demonstrate that an E/M service was performed and necessary will be denied upon review.
Code 99211 should not be used by physician or staff to bill for:
- Administering routine medications by physician or staff whether or not an injection or infusion code is submitted separately on the claim
- Checking blood pressure when the information obtained does not lead to management of a condition or illness
- Drawing blood for laboratory analysis or for a complete blood count panel, or when performing other diagnostic tests whether or not a claim for the venipuncture or other diagnostic study test is submitted separately
- Faxing medical records
- Making telephone calls to patients to report lab results or to reschedule patient procedures
- Performing diagnostic or therapeutic procedures (especially when the procedure is otherwise usually not covered/not reimbursed, or payment is bundled with reimbursement for another service) whether or not the procedure code is submitted on the claim separately
- Recording lab results in medical records
- Reporting vaccines
- Writing prescriptions (new or refill) when no other evaluation and management is needed or performed
ALSO OF INTEREST

- Provider Manual
- Claims Corner
- Clinical Corner
- Provider Resources
- News and Updates
- Provider Toolkit
- Network Information
- Legal Information
Access the EmblemHealth Portal
- Accessibility Statement
- Privacy & Security Policies
- Nondiscrimination Policy
Language Assistance:
© 2023 EmblemHealth. All Rights Reserved.
Any information provided on this Website is for informational purposes only. It is not medical advice and should not be substituted for regular consultation with your health care provider. If you have any concerns about your health, please contact your health care provider's office.
Also, this information is not intended to imply that services or treatments described in the information are covered benefits under your plan. Please refer to your Membership Agreement, Certificate of Coverage, Benefit Summary, or other plan documents for specific information about your benefits coverage.
Back to Top

99211 CPT Code (2023) | Description, Guidelines, Reimbursement, Modifiers & Examples
The 99211 CPT code may be used for established patients and is defined as those treated by the provider (or another member of the same medical group and specialty in the last three years. You can’t use 99211 for a new patient . When it comes to 99211, the established-patient rule is crucial.
Medicare uses the concept of incident-to-services, which states that an initial course of treatment initiates with the help of a provider who provided direct, professional service to that patient before giving the 99211 CPT code services.
At the time of an appointment, the supervising provider must be in the office suite to submit the code 99211 to specific payers (including Medicare). There is no need to have a billing provider in the patient’s room or to conduct face-to-face services for this provider.
The supervising provider does not need to be the one who wrote the care plan. If you use 99211 CPT code services “incident to,” you may note the professional who gave it and the doctor who oversaw it.
An “incident to” treatment will document the supervising physician’s engagement in the patient’s care in some form, such as by using one of the following:
- It’s critical to emphasize the nature of the doctor’s participation, whether they much or how to care
- Evidence from previous service dates suggests a close link between them.
Medicare has looked into a few incidents where the code 99211 may enter incorrectly. Upon examination, all 99211 activities for which proper documents do not prove that an E/M service may perform will reject as defined in this document.
Appointments for established patients may require the attendance of a physician or other competent healthcare provider, or they may not necessitate their presence at all. Code 99211 specifies an “outpatient visit for the evaluation and care of an established patient that may not require the presence of a physician,” as CPT defines.
According to CPT’s findings, 5 minutes may spend conducting or supervising these services. It is a small problem if it does not demand the presence of a physician or other competent healthcare professional, but the therapy administers under their supervision.
American Medical Association: “If the physician or other qualified health care professional’s time may spend overseeing clinical employees who conduct the face–to–face services in an encounter, use 99211 CPT code.”
99211 CPT Code | Description
According to CPT, there are two types of established patients: those with a history of receiving technical advice from one practitioner and those without.
For the 99211 CPT code, Medicare uses “incidental services,” and established patients are critical. A non-physician practitioner performs services unrelated to the patient’s primary care (e.g., RN). Providing the 99211 services was a byproduct of the provider’s larger long-term care strategy.
CPT® code 99211 is defined as follows in the 2011 CPT Standard Edition handbook:
“It is common for minor issues to cause the visit. It usually takes less than five minutes to provide or monitor these tasks”.
Evaluating and managing a patient in person include documenting clinically relevant and essential information exchange.
For the documentation to be understandable, it must include information about the service provider, including their name and qualifications. For “incident to” services, an auxiliary staff member may favor the physician, and the physician’s charge will reflect that.
It is essential to identify and credential the doctor who supervised the treatment and the medical professionals who performed it. There will be no acceptance of any service that does not show or prove that an E/M service was completed and is necessary.
Regular drugs are provided by doctors and staff members regardless of what an injection or infusion code is stated separately on the claim.
99211 CPT code will use by clinicians or labor to bill for the following items:
- Blood pressure may check to see if the information gained helps control the disease.
- Payment for blood samples may obtain, or a similar diagnostic research test will submit separately from a claim for blood collection for laboratory examination, a complete blood cell screen, or other diagnostic tests.
- Diagnoses and treatments that aren’t generally covered or reimbursed (especially when payment may couple with reimbursement for another service) can perform.
Billing Guidelines
Two of the most significant recorded portions of all resolved office patient charge codes define the suitable administration level (99211-99215). In contrast, new patients’ consideration experiences in the office must meet the requirements of the three most frequently raised parts described above (99201-99205).
Only the top two-thirds of sections should be able to establish whether or not CPT® 99213 warrants further study. The following test may design to assess your knowledge of the prerequisites necessary to pass the CPT 99213 exam.
Eye-to-eye contact is essential in all E/M events, as it always has been. Codes for outpatient centers allow Medicare to bill for episodes the administration may provide by someone other than the doctor.
Depending on the situation’s specifics, the doctor may be able to bill for the whole amount. The administration billed the incident to the doctor’s supplier number. It’s a medical coding number, 99213. As a whole, the issue’s history.
Only 1-3 elements may need the historical context of the current illness (HPI) or the status of three ongoing restorative conditions (HPI). Therapeutic, social, and familial histories may require for admission.
Preventative care includes Pap Smears , which detect abnormalities in the cervical tissue. Visit the office (99211 CPT code), and 95115-95117 are incompatible (allergen immunotherapy). Mutually exclusive services are not eligible for separate reimbursement.
Preventive and routine doctor’s visits will consist of this category. Counseling and care coordination are essential in determining eligibility for E/M services if it accounts for more than half of the physician’s patient and family contact (in the office or other outpatient environment).
99211 CPT code for outpatient care may provide in a clinic or another outpatient facility to established patients who do not take place in the presence of a clinician or other licensed health care practitioner.
Problems presented are typically minimal. The average time to provide or monitor these services is five minutes. Billing instructions instruct that the bill one unit for each visit.
How To Use Modifiers With The 99211 CPT Code
Only established office visits (99211-99215) billed with modifier -25 are payable with treatments when there are two separate diagnoses on the claim and the billing expert is a dermatologist.
E&M services invoiced with Current Procedural Terminology (CPT®) code 99211 and modifier 25 on or after March 16, 2020, will be denied reimbursement if they bill alone or with another procedure code on the same day the service was performed.
For a low-level E&M visit that does not need the presence of a physician or the recording of essential components, CPT code 99211 may use to bill for the history, examination, and physician prescription. Modifier 25 mandates the medical facility service to document all crucial details.
In this case, just the CPT code 99211 with modifier 25 will reject. We will amend our reimbursement policy for evaluation and management services to reflect this change.
E/M service code 99211 may not compensate for diagnostic and therapeutic purposes. The procedure’s definition of “major” does not include this low service level code. Hence it will not give in addition to the procedure code.
Drug administration services, such as chemotherapy or non-chemotherapy drug infusion, should not be billed with Procedure Code 99211, and carriers should alert providers (effective January 1, 2004).
On November 14, 2004, the FDA added a therapeutic or diagnostic injection code to its policy as part of the Clinician Fee Schedule Final Rule. At this point (January 1, 2005).
Medically essential, significant, and distinct E/M services (that meet a higher level of complexity than Procedure 99211 CPT code) may perform in addition to one administration service, and E/M Procedure codes will report with modifier -25.
Documentation is required to prove the level of E/M service charged. If an E/M service will provide on the same day, a new diagnosis is unnecessary. Having a physician present for an outpatient appointment for an established patient’s evaluation and management does not need their presence.
These services take five minutes to provide or monitor, costing between $25 and $40 per hour. Code 99211 office or outpatient appointments for existing patients do not require the presence of a physician or other registered health care practitioner.

Reimbursement
In cases where the operation is not otherwise covered/reimbursed, or payment may bundle, whether or not a single procedure code can submit on the claim for clinical procedures. In 2021, Medicare will pay $23.03 for this code.
Inappropriate Usage
Don’t use CPT 99211 to bill Medicare for phone calls to patients.
Don’t report CPT 99211 to bill Medicare solely for writing prescriptions (new or refill) when no other evaluation and management is necessary or performed.
Don’t use the 99211 CPT code to bill Medicare for blood pressure checks when the information obtained does not lead to managing a condition or illness.
Don’t report CPT 99211 to bill Medicare when drawing blood for laboratory analysis or when performing other diagnostic tests, whether a venipuncture or other diagnostic study test is submitted separately.
Don’t use CPT 99211 to bill Medicare when drawing blood for laboratory analysis for anti-coagulation monitoring and no face-to-face counseling occurs with the beneficiary, even if a results later that day are called to the beneficiary.
Don’t report the 99211 CPT code for face to face counseling that is provided without a medical need for such counseling; i.e., provided solely because the patient comes for laboratory testing.
Don’t report CPT 99211 to bill Medicare routinely when administering medications whether or not an injection (or infusion) code is submitted separately.
Billing Examples
Below are billing examples for the 99211 CPT code.
Please arrive at the office of a long-term orthodontics patient who complains of a wire irritating their face and asks that you check it out. orthodontists and maxillofacial surgeons
During an allergy vaccine injection, a 20-year-old female patient observes by a nurse for any reaction signs. (Otolaryngology/Head and Neck Surgery)
A 45-year-old man with chronic renal failure may see at the office for the supply of erythropoietin. (Nephrology)
Patient: A Peace Corps volunteer visits the office and asks for proof that her third molar will remove. She is already an established patient. Dentists and Maxillofacial Surgeons
Treatment of an established female patient, 69 years old, by removing some antibiotic gauze from an infected wound site. (Plastic surgery)
Office visit for an 82-year-old female, established patient for a monthly B12 injection with documented Vitamin B12 deficiency. (Geriatrics/Internal Medicine/Family Medicine)
Office visit for a 50-year-old male, established patient, to remove uncomplicated facial sutures. (Plastic Surgery)
Office visit for an established patient who lost a prescription for lichen planus; returned for new copy. (Dermatology)
Office visit for an established patient undergoing orthodontics who complains of a wire irritating his/her cheek and asks you to check it. (Oral & Maxillofacial Surgery)
Office visit for a 50-year-old female, an established patient, seen for her gold injection by the nurse. (Rheumatology)
Similar Posts
Cpt codes for cellular regeneration, evaluation study and ablation procedures.
Below is a list summarizing the CPT codes for cellular regeneration, evaluation study, and ablation procedures. CPT Code 0489T CPT 0489T describes the harvesting, isolation, preparation, incubation, removal, determination of concentration, and dilution of autologous adipose-derived regenerative cells for scleroderma in the hands. CPT Code 0490T CPT 0490T describes autologous adipose-derived regenerative cell therapy for…

New EHR Attestation Deadline for Eligible Professionals
CMS is extending the deadline for eligible professionals (EPs) to attest to meaningful use for the Medicare Electronic Health Record (EHR) Incentive Program 2013 reporting year from 11:59 pm ET on February 28, 2014 to 11:59 pm ET March 31, 2014. In addition, CMS is offering assistance to eligible hospitals that may have experienced difficulty…
How To Use CPT Code 27560
CPT 27560 describes the closed treatment of patellar dislocation without anesthesia. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 27560? CPT 27560 can be used to describe the closed treatment of patellar dislocation without anesthesia. This code is…
How To Use CPT Code 36571
CPT 36571 describes the insertion of a peripherally inserted central venous access device (PICC) with a subcutaneous port in patients who are five years of age or older. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 36571? CPT…
How To Use CPT Code 0167U
CPT 0167U describes a specific laboratory test known as the AdexusDx® hCG Test from NOWDiagnostics. This article will cover the official description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, and examples of CPT code 0167U. 1. What is CPT Code 0167U? CPT 0167U is a unique code that represents the AdexusDx®…
How To Use CPT Code 55801
CPT 55801 describes the excision procedure on the prostate gland through an incision in the perineum. This article will cover the description, official description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 55801? CPT 55801 is used to describe a surgical excision procedure on…
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
What Services Are Included in the Immunization Administration Codes?
- Relative Values of Immunization Codes*
What Additional Services Are Required to Appropriately Report 99211?
What are the documentation requirements for 99211, coding information from cpt and the cms, coding examples, vignette #1, vignette #2, vignette #3, when is it appropriate to report 99211 during immunization administration.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
American Academy of Pediatrics Committee on Coding and Nomenclature; When Is It Appropriate to Report 99211 During Immunization Administration?. AAP Pediatric Coding Newsletter April 2005; 2005 (2): No Pagination Specified. 10.1542/pcco_book014_document002
Download citation file:
- Ris (Zotero)
- Reference Manager
Code 99211 should not be reported for every nurse-only vaccine administration patient encounter. Rather, careful consideration needs to be given concerning the significance and medical necessity for such a visit.
When vaccines are given in the pediatric office, questions often arise concerning the reporting of evaluation and management (E/M) services performed during the same visit as the administration of vaccines. The answer always depends on whether the provider performs a medically necessary, significant, separately identifiable E/M service in addition to the immunization administration. If such a service is performed, an E/M code is reported, most likely from the 99201–99215 code family (office or other outpatient service), in addition to the appropriate code for immunization administration ( 90465–90468 or 90471–90474 ) and the code for the vaccine product(s). In these cases, payers may require modifier -25 (significant, separately identifiable E/M service performed by the same physician on the same day of the procedure or other service) to be appended to the E/M code to distinguish it from the actual administration of the vaccine.
The identification of a significant, separately identifiable service for E/M codes usually involves the performance and documentation of the key components (ie, history, physical examination, and medical decision making) or time. However, 99211 is unique among E/M codes in that it has no key component requirements. The Physicians’ Current Procedural Terminology (CPT ® ) descriptor for code 99211 states, “Office or other outpatient visit for the [E/M] of an established patient that may not require the presence of a physician. Usually, the presenting problem(s) are minimal. Typically, 5 minutes are spent performing or supervising these services.” Therefore, how this concept is defined when the E/M code in question is 99211 needs further clarification.
To address this issue, it becomes important to determine the following:
What services are included in the immunization administration codes?
What additional services are required to appropriately report 99211?
What are the documentation requirements for 99211?
The following services are included in the immunization administration CPT codes:
Administrative staff services such as making the appointment, preparing the patient chart, billing for the service, and filing the chart
Clinical staff services such as greeting the patient, taking routine vital signs, obtaining a vaccine history of past reactions and contraindications, presenting a Vaccine Information Statement (VIS) and answering routine vaccine questions, preparing and administering the vaccine with chart documentation, and observing for any immediate reaction
The relative value units of injectable immunization administration codes have been significantly increased for 2005. This accounts for the fact that many of the services that were previously reported separately with code 99211 are now included in the immunization administration codes.
The immunization administration codes are valued on the Medicare physician fee schedule (Resource-Based Relative Value Scale [RBRVS]) as shown in Table 1 .
* CPT , Physicians’ Current Procedural Terminology ; RVUs = relative value units.
† Medicare 2005 conversion factor = $37.8975. Sample conversion: for 90465 , 0.49 RVUs x $37.8975 = $18.57.
‡ The Centers for Medicare and Medicaid Services considers oral/intranasal immunization administration to be “self-administered” and therefore has not published RVUs for these codes. The American Academy of Pediatrics is working to get RVUs published for codes 90467, 90468, 90473 , and 90474.
The E/M service must exceed those services included in the immunization administration codes. In addition, the following 2 principles must be kept in mind:
The service must be medically necessary.
The service must be separate and significant from the immunization administration.
When the provider (usually the nurse) evaluates, manages, and documents the significant and separate complaint(s) or problem(s), the additional reporting of 99211 is justified. In such circumstances, the nurse typically conducts a brief history and record review, along with a physical assessment (eg, indicated vital signs and observations), and provides patient education by helping the family or patient manage the problem encountered. These nursing activities are all directly related to the significant, separate complaint and unrelated to the actual vaccine administration.
All reported E/M codes must meet documentation requirements as outlined in CPT guidelines or the Centers for Medicare and Medicaid Services (CMS) documentation guidelines. For most of the E/M services physicians perform, this means that some designated combination of the key components of history, physical examination, and medical decision making must be met and clearly documented. Alternatively, if more than 50% of the time spent during the E/M service is in counseling or coordinating care, time becomes the key or controlling factor in selecting a code.
Code 99211 is the one E/M service typically provided by the nurse and not the physician. As such, its documentation requirements differ. There are no required key components typical of the physician services noted previously. Furthermore, the typical time published in CPT for 99211 is 5 minutes. The American Academy of Pediatrics (AAP) encourages documenting the date of service and reason for the visit, a brief history of any significant problems evaluated or managed, any examination elements (eg, vital signs, appearance of a rash), a brief assessment and/or plan along with any counseling or patient education done, and signatures of the nurse and supervising physician.
While not required, it may help payers better understand the medical necessity of the nurse E/M service if, when appropriate, it is linked to a different International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code than the one used for the vaccine given. Encounter documentation should be a separate entry from the charting of the vaccine itself (ie, product, lot number, site and method, and VIS date, which usually are all recorded on the immunization history sheet). Each practice should consider developing protocols and progress note templates for vaccine services.
Finally, if the nurse provides the 99211 visit, it is reported under the physician’s name and tax ID number, making it inherently an incident to service. In such situations, it is a service restricted to established patients and requires the supervising physician’s direct supervision , which is defined by the CMS as the physician being physically present in the office suite (not in the patient’s room) and immediately available to provide assistance. Most nurse E/M services are carried out under a protocol of orders developed by the physician for the particular service and should be fully documented in the record. As always, the physician supervising the care should sign the chart entry.
The American Medical Association provided some instruction on reporting 99211 at the time of immunization administration in its October 1999 CPT Assistant. CPT reaffirms the nature of a reportable E/M service as significant and separate from the immunization administration itself.
The CMS also provides some direction for reporting 99211 for visits in which only the nurse sees the patient and gives an injection. The CMS notes that it is not correct to report an E/M service if the nurse services are only related directly to the injection itself. For 2005, the CMS has significantly increased its fee for immunization administration, providing reimbursement for the typical activities of the nurse as listed herein, under immunization administration. While private payers generally will follow the CMS lead in such coding guidance, it should be noted that some do not use Medicare RBRVS; these payers have their own reporting guidelines and payment policies for nurse visits. As in other coding areas, pediatricians may need to query payers when developing office policies on reporting nurse services and be careful to review the explanation of benefits returned from all payers after these claims are processed.
A 7-month-old girl visits your office to be immunized against influenza and is seen only by your nurse. The nurse takes a brief history and learns the infant has a cough without change in appetite, sleep, or activity level. The nurse takes vital signs, assesses that the infant has no contraindications to getting the vaccine, and discusses the management of the respiratory problem with the parent. Additionally, the nurse documents that the patient meets the current guidelines for vaccination and has no contraindications to the immunization per the Centers for Disease Control and Prevention (CDC) guidelines. Next, the nurse reviews the VIS with the parent and obtains consent for the im-munization. The nurse then administers the influenza vaccine.
The encounter would be reported as follows:
An example of written documentation for this 99211 encounter follows (the actual vaccine data with lot number, site or route, and VIS date are recorded on a separate immunization record):
“The patient is here for the influenza vaccine. Parent reports a cough for several days without any fever. Patient is eating well, and there has been no wheezing or rapid breathing. Her temperature is 98.7ºF and respiratory rate is 38 breaths per minute—she appears well. The symptomatic treatment of the cough per protocol was discussed and the parent was instructed to call or return if the problem worsened.
“She has no allergies to foods or history of reactions to past vaccines. The risks and potential side effects of the influenza vaccine were discussed after the VIS was given, and the parent was informed of the correct dosage of an antipyretic should fever or fussiness occur afterwards. An influenza vaccine was given.
“K. Brooks, LPN/R. Dunn, MD (signatures/date)”
A 5-year-old is brought in by a parent for a catch-up measles-mumps-rubella (MMR) vaccine. The parent says the child is fine and has already been counseled on the vaccine and has no concerns. The nurse proceeds to review the vaccine history, present the VIS, and receive an order for the vaccine from the physician. The nurse then administers and documents the vaccine. In this situation, the service is only vaccine related and no significant or separate E/M service is provided. Therefore, the only services reported are the immunization administration and vaccine product codes.
A 4-month-old patient had an illness with high fever at her preventive medicine visit 2 weeks ago, and now returns to see your nurse for her second hepatitis B vaccine. The nurse performs an interval history, finding the symptoms from the earlier illness have resolved. The nurse then confirms that the infant is afebrile by taking the infant’s temperature and makes the observation that the infant is playful. After assessing that the patient is currently in good health, the nurse confirms that there are no contraindications to the immunization per CDC guidelines. Next, the nurse reviews the VIS with the parent and antipyretic dosage for weight and gets the parent’s consent for the immunization. The nurse then administers the hepatitis B vaccine, observes for immediate reactions, and schedules the third hepatitis B immunization visit for 2 months later.
This encounter would be reported as follows:
“The patient is here for a missed hepatitis vaccine and has had no fever for 7 days, is eating again, and seems to be well per parent. Past vaccines have been well tolerated. Her temperature now is 98.7ºF and she appears well. The risk and potential side effects of the hepatitis vaccine were discussed after the VIS was given and the parent was informed of the correct dosage of an antipyretic should fever or fussiness occur afterwards. The night call system was explained and the access number given.
Some payers may inappropriately deny claims that link code 99211 to a V ICD-9-CM code. Neither CPT nor ICD-9-CM guidelines prohibit such reporting when the ICD-9-CM code reported is the most specific one available to describe the patient encounter (see Table 2 ). Furthermore, CPT guidelines clearly outline the requirements for reporting a given level of E/M code. If the key components of history, physical examination, and medical decision making or time requirements (when greater than 50% of the visit is spent counseling or coordinating care) are met for a given code, the physician is correct in the reporting of that code. CPT guidelines do not make the reporting of a certain level of E/M code contingent on the patient exhibiting certain symptoms or falling under a particular diagnosis. CPT guidelines correctly recognize that there can be considerable variation in the treatment of a patient with a particular diagnosis and that it is inappropriate to validate the legitimacy of a reported E/M code by the presence of a certain diagnosis(es). Claims adjudication processes that prohibit the reporting of V ICD-9-CM codes with anything other than preventive medicine services CPT codes are inconsistent with CPT and ICD-9-CM guidelines and counterintuitive to the continuum of care that can be provided for a patient with a given diagnosis. It also should be noted that the office or other outpatient services CPT codes (99201–99215) are not limited to sick visits only. Therefore, it is appropriate to report V or any other ICD-9-CM codes that most appropriately reflect the reason for the encounter with the office or other outpatient services codes.
For additional resources and attachments, visit http://www.aap.org/moc/reimburse/codingrbrvsresources.htm . Questions? Please contact the AAP Division of Health Care Finance and Practice at [email protected] .
This document was originally prepared for AAP members on the AAP Member Center Web site ( http://www.aap.org/moc) .
Recipient(s) will receive an email with a link to 'When Is It Appropriate to Report 99211 During Immunization Administration?' and will not need an account to access the content.
Subject: When Is It Appropriate to Report 99211 During Immunization Administration?
(Optional message may have a maximum of 1000 characters.)
Citing articles via
Email alerts.
Advertising Disclaimer »
Affiliations
- CEU Quizzes
- Coding Hotline
- Online ISSN 1934-5143
- Print ISSN 1934-5135
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account

Knowing the rules can help practices receive payments that better reflect the work of the whole health care team.
BETSY NICOLETTI, MS, CPC
Fam Pract Manag. 2024;31(3):9-14
Author disclosure: no relevant financial relationships.
Medical services are usually billed by the individual who performs the service. However, Medicare has two exceptions — “incident to” and “shared services.” These two rules essentially allow physicians to bill for care provided by clinicians and staff who work with them as if the physicians had done it themselves. They're similar rules, but with key differences.
Incident-to services are performed in physician offices or patients' homes, while shared services are performed in facilities such as hospitals or nursing homes. Incident-to services can be performed by either non-physician clinicians (NPCs) or clinical staff as part of the billing physician's professional services, while shared services must be performed by two clinicians (physicians or NPCs) who each could have billed the service on their own. (See “ Incident-to vs. shared services comparison .”)
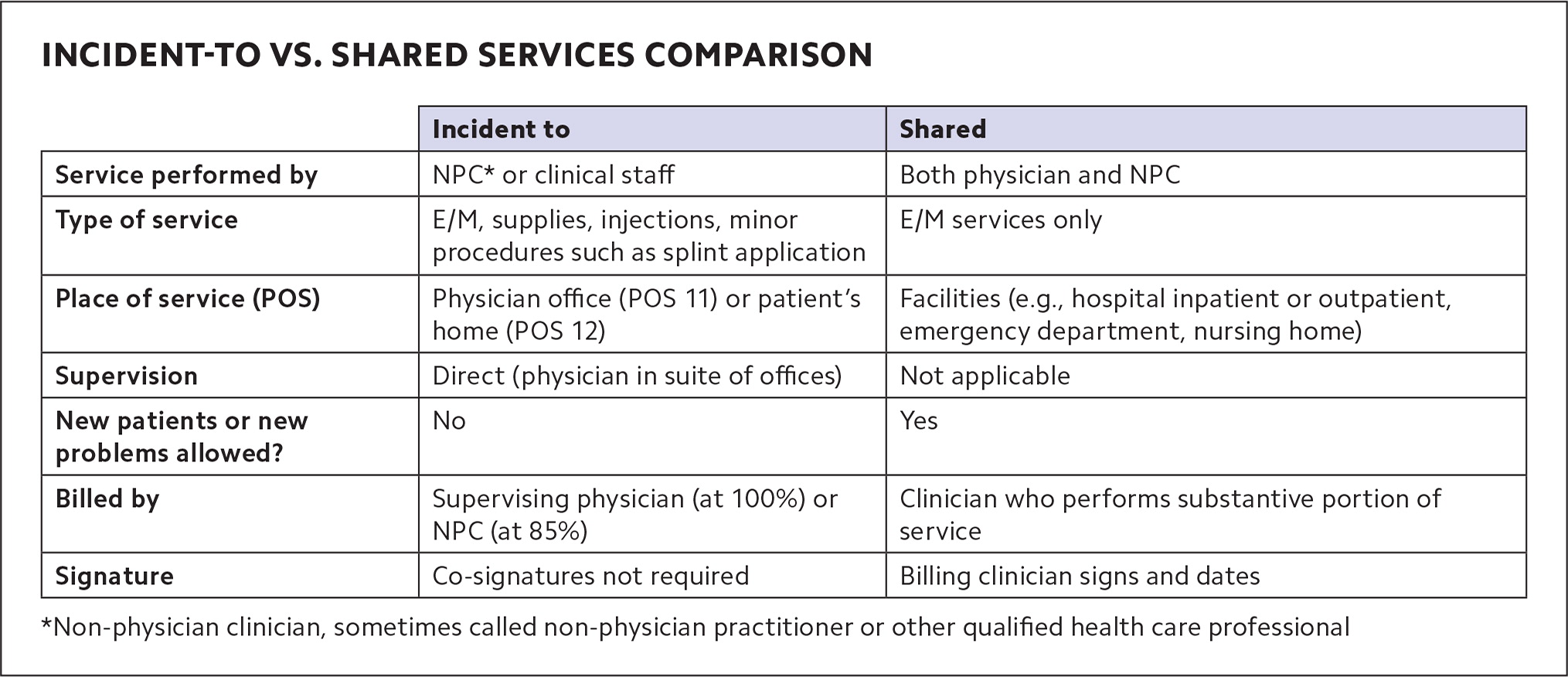
In either case, though, if the physician is billing, Medicare pays the full physician fee schedule rate, while services billed by NPCs are paid at 85% of that. Some private insurers also allow incident-to billing and shared services billing under rules similar to Medicare's, but this varies by payer.
Shared services rules have changed recently, as CPT has published new definitions (which Medicare has largely adopted, for now). The requirements for incident-to billing haven't changed, but they can be confusing, and because family physicians tend to use incident-to billing more often, a refresher is useful. This article provides that refresher on incident-to billing, as well as an explanation of the changes to shared services billing, and has a set of questions and answers with specific scenarios to help physicians understand when and how to use each of them.
Medicare allows supervising physicians to bill for services that other members of the health care team provide in office or home settings (“incident-to” billing) and bill for services they provide jointly with other clinicians in facility settings (“shared services”).
Some private payers also allow incident-to billing and shared services billing, and CPT has released definitions for shared services.
Shared services are billed by the physician or other clinician who performed the “substantive portion” of the E/M visit, which is easier to determine when using total time.
INCIDENT-TO REFRESHER
Incident-to rules allow a supervising physician to report services performed by NPCs or auxiliary clinical staff as if the physician personally provided them. NPCs are most often physician assistants or nurse practitioners. They're sometimes called “other qualified health care professionals” (QHPs)” or “non-physician practitioners” (NPPs), but in this article we'll refer to them as NPCs. Clinical staff are most often medical assistants or nurses, but could include other professionals who work under physicians' supervision (see “ Definitions ”). Billing for incident-to services under the supervising physician's name and National Provider Identifier (NPI) results in the full reimbursement rate.
DEFINITIONS
Non-physician clinicians (NPCs) or non-physician practitioners (NPPs): Physician assistants and a variety of advance practice registered nurses (e.g., clinical nurse specialists, certified nurse midwives, nurse practitioners, and certified registered nurse anesthetists) who are allowed to bill Medicare directly.
Other qualified health care professional: According to CPT, “A physician or other qualified health care professional is an individual who by education, training, licensure/regulation, and facility privileging (when applicable) performs a professional service within his/her scope of practice and independently reports a professional service. These professionals are distinct from clinical staff.” This includes the NPCs/NPPs above, but also other professionals such as physical therapists and clinical social workers.
Clinical staff member: According to CPT , this is “a person who works under the supervision of a physician or other qualified health care professional and who is allowed by law, regulation, and facility policy to perform or assist in the performance of a specified professional service.” This includes medical assistants and nurses.
NPCs may also use incident-to billing for services clinical staff provide under their supervision. As noted, though, Medicare will pay a lesser rate (85% of the physician fee schedule amount) for incident-to services billed using the NPC's name and NPI on the claim form.
Incident-to services include evaluation and management (E/M) and other services and supplies commonly furnished in medical practices, such as applying a splint, doing an injection, or checking blood pressure at a nurse visit. Incident-to billing does not apply to services with their own statutory benefit categories (i.e., groups of services health plans are legally required to cover), including wellness visits, clinical diagnostic tests, and pneumococcal, influenza, and hepatitis B vaccines.
To bill for a service that an NPC performed under the physician's NPI (at the full physician rate), these requirements must be met:
• The service must be part of a physician's plan of care . The physician sees the patient at a prior encounter and establishes the plan of care. After that, the NPC may see the patient as part of the physician's treatment. (If a subsequent E/M service can be performed entirely by clinical staff, rather than an NPC, the supervising physician may still bill for it as an incident-to service at the full physician rate using E/M code 99211 — the lowest level of E/M. Higher level E/M services must be performed by an NPC or physician.) E/M services for new patients, or new problems for existing patients, aren't eligible for incident-to billing because they are not part of the physician's preexisting plan of care. If an NPC provides these services, they must bill for them under their own NPI (at the 85% rate).
• The service requires direct supervision . The physician, or the physician's covering partner, is in the suite of offices (or patient's home) and immediately able to assist if needed when the NPC performs the service. Medicare rules are generally interpreted as requiring the supervising physician to be in the same or a similar specialty as the NPC performing the service, although the Centers for Medicare & Medicaid Services (CMS) doesn't specifically say this. Likewise, CMS does not specifically define supervision beyond the physician being “in the suite of offices,” but some payers interpret it to mean not separated by a set of stairs or elevator.
• The NPC must be an expense to the practice , either employed, leased, or contracted.
• The physician must stay involved in the plan of care , but CMS does not describe exactly what this entails. It could mean alternating visits with the NPC or periodically seeing the patient. Simply signing off on the record alone is less compelling as documentation, and there is no Medicare requirement for co-signature. NPCs can provide documentation that supports incident-to billing by noting in their assessment that the visit was part of the physician's plan of care and that the physician was in the office. But CMS does not specifically require this.
• The NPC must be enrolled in Medicare , whether billing directly or incident to the physician, according to U.S. Department of Health and Human Services guidance. 1
SHARED SERVICES
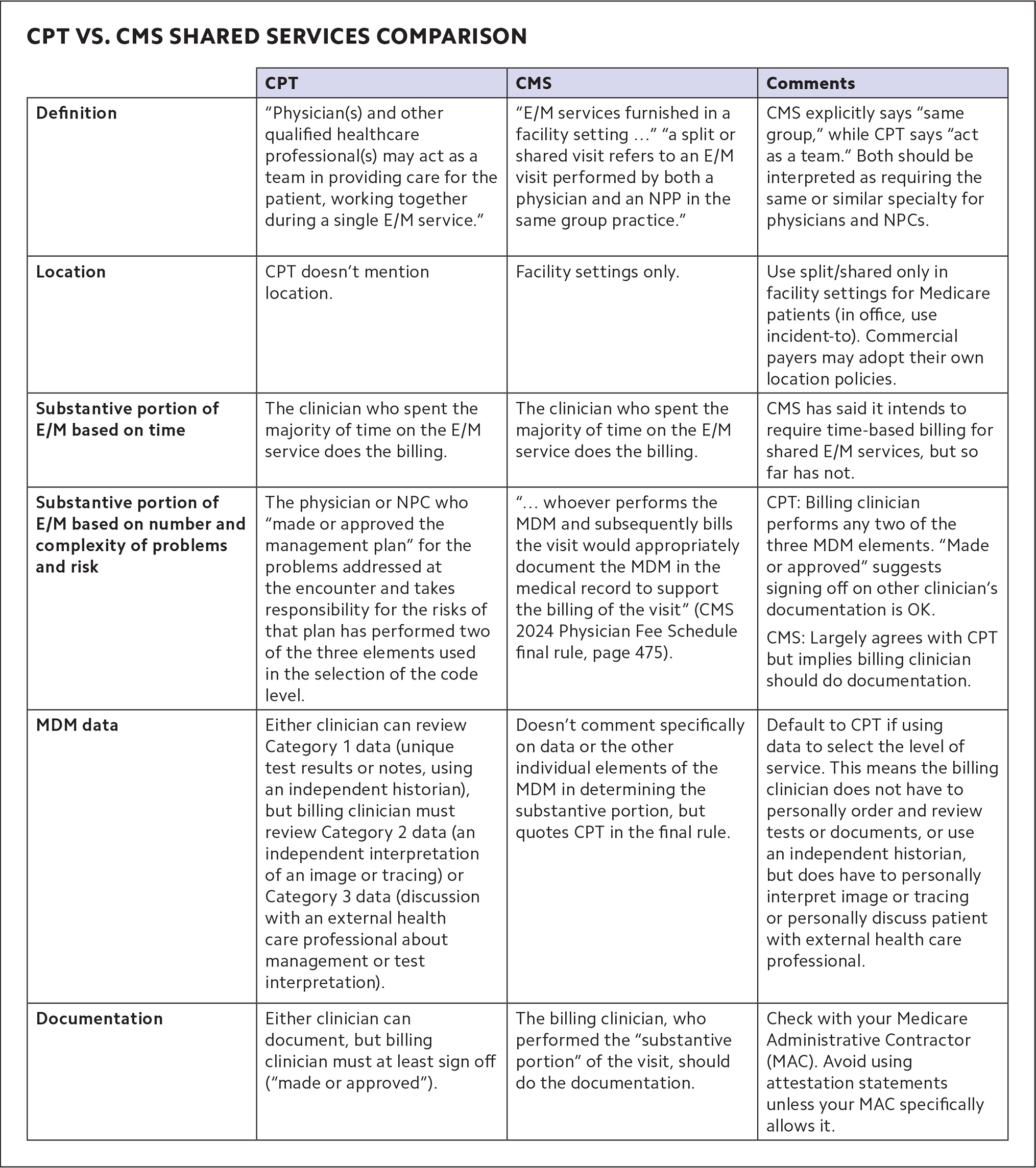
Until recently, only Medicare defined shared services. But CPT added its own definition in 2021 and expanded it in 2024. (See “ CPT vs. CMS shared services comparison .")
Shared services are E/M services that a physician and NPC perform jointly in a facility setting, such as inpatient and outpatient hospital buildings, emergency departments, and nursing homes. Shared services may not be performed in physician offices that are not part of a facility setting. The place of service (POS) code is key to shared services billing. 2 For example, hospital outpatient clinics that use POS 19 (on campus) or 22 (off campus) can bill for shared services, whereas physicians' offices that use POS 11 cannot. (It's the opposite with incident-to services, which can be billed with POS 11, but not POS 19 or 22.)
Both clinicians must be enrolled in Medicare and able to perform E/M services on their own (a physician may not share E/M services with a social worker or dietitian, for example, because those professionals don't have E/M in their scope of practice). 3
To bill for E/M as a shared service, both clinicians must participate in the patient's care on the same calendar day. The identity of both clinicians must be included in the encounter note, but only the billing clinician is required to sign and date the medical record. That clinician then submits the claim using HCPCS modifier FS (“split [or shared] evaluation and management visit”) for Medicare.
Remember that when the physician bills for the shared service, Medicare pays 100% of the physician fee schedule allowance, but when an NPC bills, it results in payment of only 85%. So, it makes sense to bill under the physician's NPI when possible. But under both Medicare and CPT rules, physicians may only do this if they perform the “substantive portion” of the service.
Billing based on time . If you're billing for E/M based on total time, determining who provided the substantive portion of the visit is pretty straightforward: The clinician who accounted for more than half the visit's total time (face-to-face and non-face-to-face time combined) performed the substantive portion of the service. Thus, both clinicians should document their own time, and if the physician's time is greater than half, the service should be billed under the physician's NPI. The only complicating factor with time-based coding is that if the physician and other clinician meet to discuss the patient, or see the patient together, only one of them can count those minutes — they can't double-count them.
Billing based on MDM . If you're using medical decision making (MDM) to code an E/M service, determining who performed the substantive portion is significantly more complicated. There's no quick and clear way to do it, but here is some guidance based on both CPT and CMS rules.
MDM is defined by three elements: the number and complexity of problems addressed, the amount and/or complexity of data reviewed and analyzed, and the risk of morbidity and/or mortality from additional diagnostic testing or treatment. In 2024, CPT added this instruction: “performance of a substantive part of the MDM requires that the physician(s) or other QHP(s) who made or approved the management plan for the number and complexity of problems addressed at the encounter take responsibility for that plan with its inherent risk of complications and/or morbidity or mortality of patient management. By doing so, a physician or other QHP has performed two of the three elements used in the selection of the code level based on MDM. If a practice codes the visit based on medical decision-making (MDM), the practitioner who performs the problems addressed and risk portions of the visit reports the service.” 4
The key takeaways are this:
The physician or NPC who evaluates the problems and determines and takes on the risk of the additional testing and treatment of those problems (two of the three MDM elements) meets the “substantive portion” threshold to qualify as the billing clinician.
CPT states that the billing clinician “made or approved the management plan.” It does not state that the billing clinician must personally document the plan.
There is one twist. If you use data to select the level of E/M service and include Category 2 data (an independent interpretation of an image or tracing) or Category 3 data (discussion with an external health care professional about management or test interpretation), the billing clinician must perform that portion of the service. 4 Category 1 data (ordering and/or reviewing unique test results, reviewing notes, or using an independent historian) does not need to be performed by the billing clinician because this work is included in the formulation of the diagnosis and plan.
Because of the complicated nature of determining who should be the billing clinician using MDM, CMS has said that in the future it intends to require that clinicians only use time to determine who performed the substantive portion of shared services. But CMS delayed that change for the third year in a row in its 2024 Physician Fee Schedule final rule, instead saying it would follow the new CPT definition for now.
CMS also said this about shared services: “Although we continue to believe there can be instances where MDM is not easily attributed to a single physician or NPP when the work is shared, we expect that whoever performs the MDM and subsequently bills the visit would appropriately document the MDM in the medical record to support the billing of the visit.” 5
CMS does not explicitly say what the billing physician needs to document and what the NPP (or NPC) could document instead. Therefore, although CPT's guidance seems to indicate that an attestation statement is acceptable (“made or approved the management plan”), it would be prudent for physicians to personally document MDM when billing Medicare for shared services under their NPI.
PAYMENTS THAT BETTER REFLECT THE WHOLE HEALTH CARE TEAM
Clearly, the rules governing incident-to billing and shared services billing are not always simple. But the list of questions and answers should help clarify some common scenarios.
Having a basic understanding of when shared services and incident-to rules apply allows physicians to receive payments that better reflect the actual work their practices are doing, especially as team-based care increases.
Q: Dr. Taylor sees a patient for hypertension and sets a plan for the patient to return to see the nurse practitioner (NP) to titrate the medication in two weeks. When the patient comes back to see the NP, Dr. Taylor is out of the office, but her partner Dr. Jackson is in the office. Do we bill this latest visit under Dr. Taylor or Dr. Jackson?
A: Dr. Jackson. Bill under the supervising physician who is in the office and able to provide assistance if needed.
Q: A physician sees an established patient for an acute problem, a sprained ankle. Six months later, the patient slips and re-sprains the ankle and the practice's physician assistant (PA) sees the patient. Can the physician bill this as an incident-to service?
A: No, this acute condition is a new problem and should be billed by the PA.
Q: Can you bill incident to if using time to determine the level of evaluation and management?
A: Yes. You can bill incident to if using time or medical decision making.
Q: If a physician and an advance practice registered nurse (APRN) are billing for a shared service E/M visit based on time, do each of them need to document their time?
A: Yes. The clinician who accounted for more than 50% of the time bills for the service, so both the physician and the APRN must document their time. (They can't double-count time if they both see the patient together or meet to discuss the patient.)
Q: Working in an outpatient hospital department, a physician and PA each perform part of an office/other outpatient visit. It is follow up for an urgent care visit over the weekend. The patient has an acute, uncomplicated condition, and a prescription medicine is given for cough control. The physician personally interprets the chest x-ray from the urgent care visit. Under the shared services rules, who should report the E/M service and what is the correct level of service?
A: Two of the three medical decision-making elements are moderate: amount and complexity of data (independent interpretation) and risk (prescription drug management). It is, therefore, a level-4 E/M visit. The physician performed the independent interpretation of data and, therefore, may bill for the visit.
Q: Can we bill for shared services for nursing facility visits?
A: Yes. Skilled nursing visits that use place of service 31 qualify because that is considered a facility location. But nursing facility services in place of service 32 (mostly rehab providers) do not because that is considered a non-facility location. Also, shared services may not be performed for visits mandated to be done by a physician.
Advanced practice registered nurses, anesthesiologist assistants, and physician assistants. Centers for Medicare & Medicaid Services (CMS) Medicare Learning Network. MLN901623; March 2022.
Place of service code set. CMS. Updated September 2023. Accessed March 13, 2024. https://www.cms.gov/medicare/coding-billing/place-of-service-codes/code-sets
Medicare Claims Processing Manual, Ch. 12, Sec. 30.6.18A. CMS 100-04; rev. 12461. Jan. 18, 2024. Accessed March 14, 2024. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf
CPT 2024 Professional Edition . American Medical Association; 2023.
CMS-1784-F. CMS. Nov. 16, 2023. Accessed March 14, 2024. https://www.cms.gov/medicare/medicare-fee-service-payment/physicianfeesched/pfs-federal-regulation-notices/cms-1784-f
Continue Reading
More in FPM
More in pubmed.
Copyright © 2024 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

IMAGES
VIDEO
COMMENTS
Six keys to coding 99211 visits. Using CPT code 99211 can boost your practice's revenue and improve documentation. The following guidelines can help you decide whether a service qualifies: 1 ...
Whenever you report 99211, the provider should document the reason for the visit, along with any other pertinent details. Also, make sure you have the date of service, the reason for the visit, proof that the nurse performed the service per the physician's order, and the nurse's legible signature. Tip 2: Be Familiar With 99211 Components.
Unlike other E/M codes 99202-99205, and 99212-99215, time alone cannot be used when reporting 99211 when selecting the appropriate code level for E/M services. Effective January 1, 2021, time was removed as an available code-selection criterion. The typical time spent on this code is five minutes. Other visits billed with 99211.
One change to 99211 in 2021 has to do with time. Previously, the code descriptor stated, "Typically, 5 minutes are spent performing or supervising these services.". For dates of service on or after Jan. 1, 2021, you cannot bill 99211 based on time alone, as you can for the rest of the office visit codes. A nurse can document the amount of ...
Using CPT code 99211 can boost your practice's revenue and improve documentation. The requirements for most evaluation and management (E/M) codes have gotten more precise over the years. However ...
Check your nurse's credentials and payer incident-to rules before billing this E/M service. By Karla M. Hurraw, CPC, CCS-P CPT® 99211 Office or other outpatient visit for the evaluation and management of an established patient that may not require the presence of a physician or other qualified health care professional.Usually, the presenting problem(s) are minimal.
Questions continue to be raised about the appropriate billing of code 99211. Can this level of service be reported by a physician? Would it be appropriate to report a nurse visit when, for example, the nurse administers vaccines or an antibiotic, performs a strep test, obtains blood, reads a purified protein derivative (PPD), or performs a weight check?The Current Procedural Terminology (CPT ...
The 99211 CPT code can be billed for visits that do not require the presence of a physician or other qualified health care professional. Skip to content. Sales: 888-357-3226. ... For example, if a nurse provides instructions following a physician's minor procedure or takes a patient's vital signs prior to an encounter with the physician ...
If you are not sure it is worth the effort to bill for a 99211, consider that a nursing visit for a depo-progesterone shot can generate a charge of approximately $150 (nursing visit 99211=$30 ...
Using and Documenting CPT Code 99211 Services Correctly. CPT ® code 99211 is defined by the 2011 CPT Standard Edition manual as: "Office or other outpatient visit for the evaluation and management of an established patient that may not require the presence of a physician.Usually, the presenting problem(s) are minimal. Typically, 5 minutes are spent performing or supervising these services."
Summary of Major E/M Revisions for 2021: Office or Other Outpatient Services. •Extensive E/M guideline additions, revisions, and restructuring •Deletion of code 99201 and revision of codes 99202-99215. o Codes 99201 and 99202 currently both require straightforward MDM. •Components for code selection:
99211 and Incident To. CPT 99211 is an office or other outpatient visit for the Evaluation and Management (E&M) of an established patient that may not require the presence of a physician. Usually the presenting problem is minimal. Typically, five minutes are spent performing or supervising these services.
For prolonged total time in addition to office or other outpatient services (ie, 99205, 99215) on the same date of service without direct patient contact, use 99417. Codes 99358, 99359 may also be used for prolonged services on a date other than the date of a face-to face encounter. ama-assn.org. (312) 464-5000.
Visit the office (99211 CPT code), and 95115-95117 are incompatible (allergen immunotherapy). Mutually exclusive services are not eligible for separate reimbursement. ... During an allergy vaccine injection, a 20-year-old female patient observes by a nurse for any reaction signs. (Otolaryngology/Head and Neck Surgery) Example 3.
On October 1, 2021, the Centers for Medicare & Medicaid Services (CMS) changed a procedure-to-procedure edit from modifier indicator 0 to 1. After joint work between CMS and the American Academy of Pediatrics, CMS agreed to this change to allow for reporting of code 99211 if the patient presents for a nurse-only vaccine encounter and also requires a COVID-19 test.
There must be face-to-face contact to report 99211. For example, if a nurse returns a patient's call and gives instructions over the phone, you can't submit 99211 for reimbursement. Don't underestimate the importance of documentation. Documentation is essential when requesting reimbursement for 99211 visits.
practice, such as a nurse or other staff member. • Unlike other office visit E/M codes, a 99211 office ... tion of a 99211 visit does not have any specific key-component requirements. Rather, the
Nursing Facility Services codes 99304-99310, 99315, 99316, Home or Residence Services codes 99341, 99342, 99344, 99345, 99347-99350 ... For 99211 and 99281, the face-to-face services may be performed by clinical staff.) ... such as office visits, hospital inpatient or observation care visits, and consultations. Most of the categories are ...
99202-99205, 99211*, 99212- 99215 ... Subsequent nursing facility care services (limit 1 telemedicine visit every 30 days) 99307- 99310 Transitional care management services . 99495, 99496 Advanced Care Planning . 99497-99498 Prolonged service in the office/outpatient setting requiring direct patient contact ...
Code 99211 should not be reported for every nurse-only vaccine administration patient encounter. Rather, careful consideration needs to be given concerning the significance and medical necessity for such a visit.When vaccines are given in the pediatric office, questions often arise concerning the reporting of evaluation and management (E/M) services performed during the same visit as the ...
Sync Office E/M Codes. CPT® 2022 changes the descriptor for 99211 (Office or other outpatient visit for the evaluation and management of an established patient that may not require the presence of a physician or other qualified health care professional) by dropping the phrase "Usually, the presenting problem (s) are minimal.".
have been valued to include the work and practice expenses of CPT code 99211 (Evaluation and Management (E&M) service, office or other outpatient visit, established patient, level I). Although CPT code 99211 is not reportable with chemotherapy and non-chemotherapy drug/substance administration HCPCS/CPT codes, other non-facility-
Incident-to services include evaluation and management (E/M) and other services and supplies commonly furnished in medical practices, such as applying a splint, doing an injection, or checking ...