

The Patient Journey: What it is and Why it Matters

- Share on Facebook
- Share on Twitter
- Share on LinkedIn
- Share on Email
Healthcare is under enormous pressure today.
Patient expectations about their service and experience have changed over the years. Patients have more choices about their care, and they’re more empowered with information about what they want their care experience to be. They expect you to interact with them on their terms, not yours. And with COVID-19 turning so much of our lives digital, this trend has only accelerated.
Having a robust marketing automation approach is critical to addressing these challenges in today’s environment. Meeting — and exceeding — patient expectations comes down to managing your patient’s engagement journey.
How can patient journeys improve care?
What patient journeys can do is turn the healthcare experience from a primarily reactive experience to a proactive one.
By building out journeys for your patient personas, you can close gaps in care, establishing robust preventative routines that ultimately help your patients stay as healthy as possible for as long as possible.
Engaging consumers and patients where they are builds trust and confidence that keeps patients in the system and encourages them to refer their friends and family to your practice. According to the Beryl Institute , 70% of patients will share a positive experience with others. But your bigger risk is that 76% will share a negative one. And with a negative experience, 43% of patients won’t go back to that provider, with 37% finding a different doctor altogether.
What is the patient journey?
A patient journey represents the entire sequence of events that a patient experiences within a given healthcare system or across providers, from scheduling an appointment for a regular checkup to receiving treatment for an illness or injury.
A patient journey is an ongoing process that incorporates all parts of the healthcare ecosystem, from hospitals to physicians, specialty care, and outpatient therapy.
While it is easy to think about a patient’s journey as those interactions you have with them before, during, and after an appointment, there are actually many other touchpoints that drive their overall journey. A comprehensive patient engagement strategy touches on all aspects of a patient’s relationship with a healthcare provider, including:
- Onboarding and Access
- Diagnosis and Treatment
- Adherence to Lifestyle or Behavioral Changes
- Ongoing and Proactive Health (Wellness)
- Referrals and Loyalty
How do I create the patient engagement journey?
Every single interaction with a patient is part of the patient engagement journey and a moment of truth for the health system or provider to add value.
In today’s value-based healthcare world, having that personalized experience is more important than ever. A patient engagement journey organizes those communication touchpoints and ensures you’re delivering the right information at the right time to the right person, and leveraging the appropriate communication channel. Millennials and Generation Z, for example, may be more likely to prefer a text, email, or chat to a phone call.
It’s about knowing your patients’ preferences — like that they prefer to be texted during the day while they’re at work or if they prefer an office vs. telehealth visit — and what’s going to make it easier for them, like sending automatic reminders the week and day before an appointment.
Whether it’s making sure you follow up with cardiac patients about weighing themselves daily after surgery to catch any water retention issues or asking colonoscopy patients whether or not they’ve been following post surgery protocols after discharge, it’s about continuity of care once a patient leaves the office or hospital so they have a quality outcome. From there, patients can more proactively drive their own wellness plan.
Here are important areas to focus on when creating your patient engagement journey:
Establish your patient personas
You need to know the different types of patients that are coming into your organization. You want to figure out:
- What are the most relevant needs of your patients?
- What are their communication and care preferences?
- How do they want to engage with you?
- What information do you already know about them?
To be able to craft the best possible patient experience, you first have to know more about your patients.
For example, there’s a well-known healthcare persona out there called the “Medical Mom” (which can, of course, be any individual taking care of themselves, their kids, their spouses, and may also be the caretaker for aging parents).
Let’s say this individual has three children, and they book annual physicals at their pediatrician, which happens to have offices in the same building as their own primary care physician. Wouldn’t it be nice if the office sent them one email reminder to schedule all five appointments, rather than five different emails? And when they do call, scheduling those appointments back-to-back so everyone is in and out in one afternoon?
A spreadsheet is not going to be able to do that for you. Collecting and managing the data required to drive complex, interconnected patient journeys requires more than a spreadsheet. In order to succeed, you’ll need to pay close attention to the entire patient lifecycle.
Understand the entire patient lifecycle
An appointment reminder is a great start to engaging a patient, but it’s just one event in an ongoing patient lifecycle that begins with preventative care and includes diagnostics, delivery of care, and post-operations.
For example, how many patients show up for routine blood work at their physician office and you find out they haven’t fasted for the appropriate amount of time? Sending a patient home is frustrating for them and it’s frustrating for you. If the appointment is at 2:00 PM, then that appointment reminder should have been sent at dinnertime the previous evening, reminding them that they can’t eat anything after a 6:00 AM breakfast the next morning.
You’ll want to tailor your communications based on whether the patient is new or existing, what their preferences are, and whether they have any specific or chronic health issues. From there, you need to…
Understand the moments of truth
The healthcare system is complicated, even for those who have been a part of it for decades. The key to building a great foundation for your patient engagement strategy is to put yourself in a typical patient’s shoes. Most patients don’t engage with the healthcare industry unless they’re feeling sick. That means they’re rarely at their best, and they’re not only anxious about getting better, but about the costs associated with that.
The best healthcare providers understand the moments of truth — opportunities for a positive touchpoint that can alleviate their stress and anxiety and help them get on the road to recovery. Every time you interact with a patient is an opportunity for a moment of truth, whether that be in person or via other channels of communication. It’s not only about establishing accurate moments of truth, but capitalizing on them.
It’s up to you to understand the places people need to be, how you want to communicate to them, and make every one of those touchpoints a positive experience. It doesn’t matter whether they’re physically in your office or not. Your patient engagement journey is what guides your patients to making the best possible decisions on their care so they get better.
The easier you make it for them to engage with you, the higher quality their care will be. Ultimately, you want your patients to be evangelists for your services based on their positive experiences. To do that, you’ll need to…
Get the data you need
Your patients expect personalization.
Personalization in healthcare used to mean created tailored treatment plans and clinical protocols. That’s still important, but patients expect more personalization around the entire experience, from access to communication to quality outcomes. It’s like turning on a light switch in your home: a patient just expects the light to turn on.
Personalization today means being able to see at-a-glance a patient’s healthcare record, communication preferences, and social determinants that may be impacting their overall health to give you a 360-degree picture .
To do this, you need more than clinical data.
You may have patients that constantly miss their appointments. By storing questions that go beyond health risks — say, that they’re a smoker — but to understand that they don’t have a car to get to the appointment in the first place is becoming a more important part of the process. Part of empathetic, compassionate care is understanding these environmental factors that can help patients get the care they need, whether that’s calling a Senior Shuttle, caregiver, or arranging a telehealth appointment instead.
Once you have the data, you can…
Encourage referrals and loyalty
The first place people look for a new doctor isn’t the Internet. It’s their friends and family. In an ideal world, every patient you have should be able to say, “Oh, I loved my experience with…”
Doing that starts with the technology you have. Before a patient ever comes in for treatment, you need to make sure they have a seamless experience that builds trust and encourages referrals and loyalty.
How do I get started with patient journey mapping?
It’s time to move away from the mindset to simply fill the top of the funnel with as many new potential patients and contacts with caregivers as possible. While this is still a requirement, it is just as crucial for organizations to get better at managing and growing relationships at every phase of the patient journey. Providers must engage with consumers in the marketplace to introduce them to their services of course, but it is of growing importance that they offer support throughout the entire diagnostic and treatment process.
As a Salesforce Platinum Partner with deep industry expertise, we have created a Foundation for Patient Engagement package — a complete strategy that starts with Health Cloud and facilitates a 360-degree view of the patient , as well as a comprehensive communication strategy, CTI integration, and the use cases driving patient acquisition, engagement, and loyalty.
Learn more about building your patient journey with Silverline.
From the Blog More articles about Provider

Provider Personalization in Healthcare: 6 Keys To Successful Patient Experiences

Provider Prioritize Patient Experiences with EHR CRM Integration

Provider The Future of AI for Healthcare Providers
We don't support internet explorer.
Please use Chrome, Safari, Firefox, or Edge to view this site.
Instant insights, infinite possibilities
Patient journey 101: Definition, benefits, and strategies
Last updated
22 August 2023
Reviewed by
Melissa Udekwu, BSN., RN., LNC
Today’s patients are highly informed and empowered. They know they have choices in their healthcare, which can put healthcare providers under a lot of pressure to provide solutions and meet their patients’ expectations.
- What is the patient journey?
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end.
A patient’s journey begins before they even walk through the doors of a doctor’s office or hospital. It may start when they research symptoms, treatment options, and healthcare providers. It can include referrals from friends, information found on social media, or advertisements. Before a patient enters a healthcare setting, they will call to schedule an appointment or book one online. The ease of this process can be key to patient satisfaction .
The patient journey continues through consultation, where they meet the potential caregiver. That portion of the journey includes interactions with a doctor and support staff, how long they wait to be seen, and the steps taken for diagnosis and treatment.
The patient’s post-care journey includes follow-ups from the healthcare provider, post-treatment care, and billing. For example, if the patient has questions about post-surgery care or how to read their invoice, how quickly their questions are answered and their problems resolved will impact their satisfaction.
Mapping the patient journey helps healthcare providers improve patient satisfaction at every step of the way. By collecting data at each stage and conducting an in-depth analysis, providers can identify patient concerns and make the necessary improvements to meet their patient satisfaction goals.
What is another name for the patient journey?
The term “patient funnel” describes the journey patients take from first learning about a healthcare provider or healthcare product to actually making an appointment or purchase. This “funnel” can be applied to any type of business, describing the stages a customer goes through to obtain a service.
Get a demo from a Dovetail expert
Our team can give you a demo, help you choose the right plan and ensure you get the most out of Dovetail.

- Understanding the stages of the patient journey
Each stage of the patient journey is essential to a positive patient experience . Gathering and analyzing data can alert healthcare providers to potential issues throughout the journey.
Data collection at each of the following stages will give healthcare providers the information they need to make the necessary improvements:
1. Awareness
Awareness is where the patient journey begins. This is when they first research symptoms and identify the need to see a medical professional.
They may consider at-home remedies and get advice from friends, social media, or websites. Once they identify the need for a healthcare provider, they continue their research via review sites, advertising campaigns, and seeking referrals from friends and family.
Determining the way patients become aware they need healthcare and the sources they use for research is important. The data collected at this stage could suggest your organization has an insufficient social media presence, inadequate advertising, or a website in need of an update.
To remedy these shortcomings, you might consider adding informational blogs to your website, performing a social media analysis, or closely monitoring customer reviews.
This stage in the patient journey is where the patient schedules services with the healthcare provider.
This engagement is essential for acquiring new patients and retaining current patients. Patients will contact you in several ways to schedule an appointment or get information. Most will call on the first attempt to schedule an appointment.
This is a crucial touchpoint in the journey. A new patient may become frustrated and move on if they find it difficult to access your services or are placed on hold for a long period or transferred numerous times.
Patient engagement occurs in other ways, such as your online patient portal, text messages, and emails. Your patients may interact differently, so it’s important to gather data that represents their preferred means of communication. Work to make the improvements required to correct access issues and ensure efficient communication.
The care stage can include everything from your patient’s interaction with the front desk to how long they have to wait in the examination room to see a doctor.
Check-in, check-out, admissions, discharge, billing, and of course, the actual visit with the healthcare provider are other touchpoints in the care stage.
There are a couple of ways to gather and analyze this data. Most organizations choose to analyze it holistically, even if it’s collected separately. For example, you might gather data about the patient’s interaction with the front desk, the clinical visit, and the discharge process, but you may want to analyze the care segment as a whole.
4. Treatment
Treatment may be administered in the office. For example, a patient diagnosed with hypertension may have medication prescribed. That medication is the treatment. Gathering information at this stage is critical to see how your patient views the healthcare provider’s follow-up or responses to inquiries.
In most cases, treatment extends beyond the initial clinical visit. For example, a patient might require additional tests to get a diagnosis. Providing the next steps to a patient in a timely manner and letting them know the test results is crucial to patient satisfaction .
5. Long term
A satisfied patient results in a long-term relationship and referrals to friends and family. Most of the data collected at this stage will be positive since the patient is continuing to use your services.
Gathering data after the treatment stage allows you to expand on the qualities that keep patients returning for your services in the long term.
- Benefits of patient journey mapping
The patient benefits from their healthcare provider understanding their journey and taking steps to improve it. Healthcare providers also reap several benefits, including the following:
1. Efficient patient care
When they understand the patient journey, healthcare providers can provide care more efficiently and spend less time and money on unnecessary, unwanted communications.
2. Proactive patient care
Proactive patient care is aimed at preventing rather than treating disease. For example, women who are over a certain age should have an annual mammogram, smokers may be tested for lung disease, and elderly women may need a bone density study. These preventative measures can help keep disease at bay, improve health outcomes, and build trust with patients.
3. Value-based patient care
Patients don’t want to feel they are being charged unfairly for their healthcare. Focusing on the individual patient promotes satisfaction and yields positive outcomes.
The Center for Medicare and Medicaid Services (CMS) has issued recent guidelines for participants that help offset the costs of high-quality care through a reward system.
4. Retention and referrals
Patients who are happy with their journey will keep returning for healthcare, and happy patients equal voluntary referrals. Many providers offer rewards to incentify referrals.
- How to get started with patient journey mapping
Follow the steps below to start the patient journey mapping process:
Establish your patient personas
Journey mapping is a great way to identify your patient’s characteristics so that their experience can be further enhanced.
Some of the following determinations can help you pinpoint your patient’s persona and establish protocols to provide a better service:
How do your patients prefer to communicate? Are they more comfortable with phone calls, texts, or other methods?
How are most patients finding your services? Are they being referred by friends or family members, or are they seeing advertisements?
Would the patient prefer in-person communication or telecommunication?
What are the patient’s expectations of care?
This data can be complex and widespread, but it can give you the information you need to more effectively and efficiently communicate with your patients.
Understand the entire patient lifecycle
Each patient is unique. Understanding the patient lifecycle can avoid confusion and miscommunication.
To positively engage the patient, you’ll need to gather data not only about communication methods but where they are in the patient journey, their health issue, and their familiarity with the healthcare provider’s procedures and treatment options.
Understand the moments of truth
With a few exceptions, most people seek healthcare services when they are ill or have a healthcare issue. These situations can cause patients to feel stressed and anxious. It’s these moments of interaction where compassion, knowledge, and understanding can provide relief and reassurance.
When patients see their healthcare provider, they are looking for solutions to problems. It’s the provider’s opportunity to identify these moments of truth and capitalize on them.
Get the data you need
Healthcare providers can collect vast amounts of data from patients, but the data collected rarely goes far enough in analyzing and determining solutions.
Your patients have high expectations regarding personalized treatment based on data. They want personalized, easy access to medical information and records, responsive treatments and follow-up, and communication in their preferred format.
You need more than clinical data to give patients what they want. You also need personal data that sets each patient apart and ensures a tailored experience.
For example, it might be challenging for parents of small children to contact the clinic and schedule appointments at certain times of the day. As a healthcare provider, you’ll need to be aware of the best times to contact this individual and offer simple methods for scheduling appointments.
Another example is patients with physical disabilities. You can take steps to improve their access to and experience at the healthcare facility.
Encourage referrals and loyalty
Although engagement on social media and online forums is becoming more and more common, the best way for new patients to find you is through referrals. Referrals stem from satisfactory experiences and trust.
Should you be using a customer insights hub?
Do you want to discover previous research faster?
Do you share your research findings with others?
Do you analyze patient research?
Start for free today, add your research, and get to key insights faster
Editor’s picks
Last updated: 23 August 2023
Last updated: 8 August 2023
Last updated: 2 August 2023
Last updated: 10 August 2023
Last updated: 11 September 2023
Last updated: 31 July 2023
Last updated: 16 August 2023
Last updated: 22 August 2023
Last updated: 25 November 2023
Latest articles
Related topics, .css-je19u9{-webkit-align-items:flex-end;-webkit-box-align:flex-end;-ms-flex-align:flex-end;align-items:flex-end;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-flex-direction:row;-ms-flex-direction:row;flex-direction:row;-webkit-box-flex-wrap:wrap;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;-webkit-box-pack:center;-ms-flex-pack:center;-webkit-justify-content:center;justify-content:center;row-gap:0;text-align:center;max-width:671px;}@media (max-width: 1079px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}}@media (max-width: 799px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}} decide what to .css-1kiodld{max-height:56px;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}@media (max-width: 1079px){.css-1kiodld{display:none;}} build next, decide what to build next, log in or sign up.
Get started for free
- Skip to main content
- Skip to primary sidebar
- Skip to footer
- QuestionPro

- Solutions Industries Gaming Automotive Sports and events Education Government Travel & Hospitality Financial Services Healthcare Cannabis Technology Use Case AskWhy Communities Audience Contactless surveys Mobile LivePolls Member Experience GDPR Positive People Science 360 Feedback Surveys
- Resources Blog eBooks Survey Templates Case Studies Training Help center
Patient Journey Mapping: What it is, Benefits and 5 Steps to Do it

In the rapidly evolving landscape of healthcare, patient-centered care has emerged as a crucial paradigm shift. As hospitals strive to deliver exceptional patient experiences and improve outcomes, understanding the patient journey has become paramount.
A customer journey map is a powerful tool that shares patients’ path from their first encounter with a healthcare facility to their final discharge. By visualizing this complex expedition, hospitals can gain invaluable insights into patient needs, pain points, and opportunities for enhancement, thereby revolutionizing the delivery of care.
The following article delves into the significance of patient journey maps for hospitals and their importance in optimizing patient experiences, streamlining processes, and ultimately elevating the standard of healthcare.
What is a Patient Journey Map?
A patient journey is a methodology that enables the analysis of a healthcare provider’s processes and value chain but from the patient’s viewpoint. This includes their possible solutions, pain points, emotions, touchpoints and user actions throughout the journey.
The patient journey map employs visual representation to gain deeper insights into how patients engage with a healthcare facility throughout their care journey. This unique approach is an evolution of the customer journey map , tailored specifically to the healthcare context. By employing this method, healthcare providers can unravel the intricacies of patient interactions, uncovering valuable information to enhance the quality of care provided.
The concept of the Patient Journey Map mirrors that of the Customer Journey Map, seeking to uncover areas of enhancement in patient care across various healthcare providers, including hospitals, fertility centers, and more.
Just as a skilled cartographer carefully crafts a map to navigate uncharted territories, patient journey maps chart the course of a patient’s experience, revealing hidden insights, unveiling opportunities for improvement, and ultimately guiding healthcare providers toward a destination of unparalleled patient satisfaction .
What are the benefits of implementing a Patient Journey Map?
Engaging in the patient journey proves immensely valuable as it enables us to provide patients with an optimal experience, meeting the very expectations that arise when seeking healthcare services.
The emotional aspect tied to the Patient Journey Map can be profoundly impactful, considering the inherent uncertainties often associated with visiting a healthcare facility.
Considering the unique personalities, fears, behaviors, and attitudes of different patient archetypes play a pivotal role in creating a tailored and pleasant experience for them. Thus, the patient journey map becomes a valuable tool benefiting both patients and healthcare service providers.
● Enhanced Communication with Patients:
By understanding the patient journey, healthcare providers can establish effective and continuous communication throughout the entire care process, addressing any doubts or uncertainties. Keeping patients well-informed and updated through appropriate channels reinforces the quality of care provided.
● Elimination of Blind Spots:
Clear comprehension of each stage of the patient journey helps bridge the gaps between patients and services. From the initial appointment request to discharge and follow-up, identifying and addressing potential blind spots ensures consistent and satisfactory solutions tailored to each patient’s unique situation.
● Streamlined Resolution of Pain Points:
Mapping the patient journey and defining archetypes enables a deeper understanding of patient concerns, particularly identifying which aspects of the service have the most negative impact. Pain points such as waiting times, unclear explanations, lack of empathy, or impersonalized treatments can be simplified and resolved more effectively.
Learn About: Complaint Resolution
● Process Optimization:
A well-defined patient journey optimizes workflow and allows for more efficient handling of all processes. Staff members become better equipped to anticipate and address patient issues promptly, offering alternatives that instill confidence and satisfaction.
● Continuous Improvement:
Implementing a Patient Experience model involves measuring patient experiences through a feedback system . Continuously updating the database with relevant information about patient journeys and their experiences leads to ongoing improvement in response times, customer service processes, and overall service quality .
What is a Patient Persona?
The patient persona represents an imaginary profile that encapsulates potential patients’ needs, goals, illnesses, conditions, emotions, behaviors, and knowledge.
By creating patient personas, healthcare providers can enhance the accuracy and anticipation of care and diagnosis processes, ultimately improving the experience of individuals seeking healthcare services.
5 Steps to Build Your Own Patient Journey Map
1. define the experience to map:.
Before diving into the Patient Journey Map, it is crucial to determine the specific experience you intend to outline. By establishing your objectives and identifying the type of information you seek to gather and how it will be utilized, you can ensure a more efficient mapping process right from the start.
2. Identify your Ideal Patient:
The majority of data used to construct the customer patient care journey will come directly from patient-clients. Thus, a key step is identifying the patient persona, which can be singular or multiple. You must decide whether the map will encompass various patient profiles or if separate maps will be created for each target patient.
To create the patient persona(s), gather feedback directly from patients and analyze their behaviors and data. Pose questions such as:
- What initially led the patient to seek your services?
- Which competitors did they research?
- How did they discover your website or company?
- What factors differentiated your brand from others? What influenced their decision (or lack thereof) to choose your services?
- What are their expectations when interacting with your company?
- Can they articulate what they appreciate about your company and what frustrates them?
- Have they ever contacted customer service? If so, how was their experience?
Once you have defined the patient persona(s), you can identify the distinct stages of the customer journey when engaging with your company.
3. Divide the Phases of the Customer Journey:
Throughout the customer-patient care journey, patient-clients progress through several discernible stages.
Phase #1: Pre-Visit
● DISCOVERY:
The patient journey initiates with a phase characterized by learning and concern. Patients embark on their healthcare journey upon recognizing a need or developing a concern related to a health issue.
For instance, if an individual experiences symptoms associated with being overweight, they may begin researching options for scheduling an appointment with a medical specialist. At this point, potential patients discover their specific needs and commence the process of investigating suitable solutions. They may turn to the internet, seek recommendations from friends and family, or explore other avenues. During this stage, it is recommended healthcare systems should provide educational support to aid individuals on their journey of understanding.
● CONSIDERATION:
Following their research, patients reach the consideration stage, having discovered your service. At this point, they possess some knowledge about your healthcare facility’s location and offerings, leading them to believe it could meet their needs. However, patients have also explored your competitors and are contemplating multiple options.
During the consideration stage, potential patients meticulously assess the information they come across, including service descriptions, pricing, contact pages, online inquiries, and reviews. They also evaluate the ease of accessing relevant information before scheduling an appointment and the availability of operating hours, among other factors.
Phase #3: Visit
● APPOINTMENT & ENGAGEMENT:
Having gathered sufficient information and progressed through the consideration phase, the patient ultimately chooses your service. This marks their first contact with the health center, which can occur in person, over the phone, via chat, email, or other means of communication.
During this stage, the patient schedules their appointment. The company must streamline the application process and maintain effective and proactive communication. It is crucial for this phase to be completed without complications.
● SERVICE DELIVERY:
Within the visit phase is the service delivery stage, where patients interact with various service providers at the health center. From the moment the patient enters the premises, the company must ensure an exceptional service experience.
Service delivery encompasses multiple micro-moments, necessitating comprehensive attention throughout the entire journey. Every interaction matters, from the reception care and waiting times to the core service itself—meeting the patient’s objective of being evaluated by a doctor or specialist.
Phase #3: After the Visit
● RETENTION:
The Patient journey doesn’t conclude after the initial visit. A crucial third phase occurs post-encounter, where efforts should be dedicated to fostering patient retention and encouraging their return for subsequent visits. Building strategies that monitor the patient experience is essential in designing loyalty programs to ensure patients return for future services.
● RECOMMENDATION:
Part of the post-visit phase involves patient recommendations, which heavily depend on the overall patient journey experience provided by the company. If patients have had a positive service encounter, they are likely to recommend it to others, benefiting your business.
However, it is important to remember that negative experiences are equally shared, and if patients are dissatisfied, they may spread negative feedback.
Promptly addressing any negative comments is crucial to resolving issues and preventing unfavorable recommendations.
Phase #4: Identify Touchpoints
An additional vital step in mapping the customer-patient care journey is identifying the various touchpoints between the patient and the healthcare facility. These interactions occur at different stages throughout the patient journey, and understanding these touchpoints aids in developing strategies that facilitate effective communication.
- Seeking information about healthcare centers: discovering the existence of the healthcare provider and the services it offers.
Investigation:
- Reviewing patient-client feedback: researching comments and feedback from other patients about their visit experiences at the health center.
- Exploring promotions: searching for economic benefits such as discounts, promotions, and bundled service packages.
Acquisition :
- Appointment Request: Contact or visit the health center to schedule an appointment.
- Provision of Personal Data: The health center will request personal information to finalize the appointment booking.
- Appointment Confirmation: After providing the required data, the appointment for the agreed date and time is confirmed.
- Patient Reception: The patient arrives at the health center at their scheduled appointment time.
- Waiting Room: The staff guides the patient to the designated waiting area.
- Consultation: The patient’s turn to be attended by the specialist.
- Payment: The process of settling the payment for the service, which may occur at any point during the service phase, depending on the health center’s policies.
- Patient Recommendations: Patients offer positive or negative feedback about the health center and its services.
- Loyalty Program: Incentives such as offers, promotions, discounts, or a points system to encourage future visits.
Recommendation:
- Complaint: If the patient has had a negative experience, they may file a complaint with the health center.
- Online Reviews: Patients share comments or criticisms about the service by posting reviews on the internet.
4. Identify Contact Channels
Patients engage with the health center through various channels throughout the patient journey. These channels, such as the health center itself, can be physical or online, including social media, email, applications, websites, and online forms.
Identifying the most utilized contact channels at each stage of the customer-patient care journey is crucial. This allows for the development of tailored strategies for each channel, meeting patient expectations at each phase.
Working on the patient journey is crucial for healthcare providers to deliver a high-quality experience to patients. By mapping their interactions, providers gain a deeper understanding of their patient personas, allowing them better to comprehend patient needs, desires, and circumstances to provide the desired care.
You can explore Patient Experience Software to measure your patient journey. QuestionPro published a blog about it very recently!
Patient Journey Map Example
To better understand what a Patient Journey Map is, we have created this fictitious example using one of the most reputable medical institutions in the healthcare sector, the Massachusetts General Hospital, as a reference.
In this example, we have included some generic touchpoints that are usually the most common in the interaction between a hospital and a patient.
Through this example, it would be possible to visualize the points of interaction between both parties and the perception that patients have of them, which can be positive or negative. This serves as a clear indicator for making adjustments and learning from what has been done well.
The Office of Patient Experience plays a vital role in facilitating initiatives to assess and enhance the quality of care experienced by patients and their families. They are responsible for evaluating each of these touchpoints and ensuring that appropriate actions are taken.
The Mass General Hospital is a benchmark not only in terms of service level but also in the implementation of methodologies and actions that guarantee the satisfaction of their patients. A clear example of this can be seen in the results of their annual HCAHPS survey, where they score above the national average in various aspects.
Willingness to Recommend Hospital Scores below show the percentage of patients who would “definitely recommend” Mass General to their friends and family.
To see the complete study, we invite you to visit their website and learn about it.
More Examples of Patient Journey Maps
Seeking inspiration to craft your own Patient Journey Map? Your search ends here!
Explore a collection of remarkable examples from top-notch brands, unveiling their initiatives that delight customers and foster loyalty.
Get set to revolutionize your own Patient Journey!
Mass General Hospital is renowned for providing exceptional care and taking special care in understanding the perspective of its patients. They achieve this through different tools, such as satisfaction surveys, internal and external feedback, and HCAHPS surveys .
Mayo Clinic is characterized by its focus on patient satisfaction and its extensive technical deployment to gather user and prospect feedback.
Cleveland Clinic is often ranked among the best hospitals in the United States. This recognition is not only due to its incredible facilities, global expansion, and well-prepared staff but also because of its remarkable focus on the experience they provide to its patients and clients.
Singapore General Hospital is one of the largest and oldest hospitals in Singapore. It has been a major healthcare institution providing a wide range of medical services and treatments since 1821.
Johns Hopkins Medicine has long recognized the significance of a positive patient and family experience during hospitalization, which is why they maintain a specific focus on patient satisfaction to achieve an optimal experience.
How can you enhance your Patient Journey Map based on your acquired knowledge?
The insights and recommendations shared above are likely to have sparked ideas about the potential impact of these initiatives across various industries, not just healthcare.
The first crucial step is to embrace a customer-centric approach, keeping their needs and expectations at the forefront. By doing so, the actions you take will have a meaningful impact on your customers and yield multiple benefits for your business.
At QuestionPro, we offer a range of tools and features specifically designed to help you achieve this objective.
QuestionPro SuiteCX is a Customer Journey Mapping Software that simplifies the process of creating your customer journey.
With a vast selection of templates and the ability to personalize user/buyer personas while incorporating your own data, you can conduct precise visual analyses at every touchpoint throughout your patient journey.
Start delighting your customers today!
MORE LIKE THIS
Change Management Questions: How to Design & Ask Questions
Sep 23, 2024
Top 5 Change Management Models to Transform Your Organization
Sep 20, 2024

Customer Reviews: How to Ask and Easy Ways to Get Them
Sep 19, 2024
Raw Data: What it is + How to Process It
Sep 18, 2024
Other categories
- Academic Research
- Artificial Intelligence
- Assessments
- Brand Awareness
- Case Studies
- Communities
- Consumer Insights
- Customer effort score
- Customer Engagement
- Customer Experience
- Customer Loyalty
- Customer Research
- Customer Satisfaction
- Employee Benefits
- Employee Engagement
- Employee Retention
- Friday Five
- General Data Protection Regulation
- Insights Hub
- Life@QuestionPro
- Market Research
- Mobile diaries
- Mobile Surveys
- New Features
- Online Communities
- Question Types
- Questionnaire
- QuestionPro Products
- Release Notes
- Research Tools and Apps
- Revenue at Risk
- Survey Templates
- Training Tips
- Tuesday CX Thoughts (TCXT)
- Uncategorized
- What’s Coming Up
- Workforce Intelligence
- 10 min read
What is Patient Journey: Comprehensive Guide for 2024
Key takeaways.
Patient Journey Definition: The patient journey encompasses the entire healthcare experience, from initial contact to ongoing care and follow-up, and is crucial for meeting patient needs effectively.
Patient Journey vs. Patient Experience: While the patient journey includes all interactions within the healthcare system, the patient experience focuses on the quality of these interactions and overall satisfaction.
Stages of the Patient Journey:
Awareness: Patients recognize their healthcare needs and seek information.
Consideration: Patients evaluate options and decide on a course of action, influenced by referrals and provider reputation.
Acquisition/Access: Involves scheduling appointments and obtaining necessary information, with a focus on price transparency and patient outreach.
Service Delivery/Care Delivery: Direct interactions with healthcare professionals, from check-in to discharge, impact the patient's trust and satisfaction.
Ongoing Care and Patient Loyalty: Continuous care and engagement foster patient loyalty and improve health outcomes.
Creating a High-Quality Patient Engagement Journey:
Establish patient personas to tailor services.
Track and monitor patient activity for proactive engagement.
Develop integrated patient units for seamless care.
Encourage referrals and loyalty through positive engagement.
Patient Journey Mapping: Essential for understanding and improving the patient experience by identifying gaps and optimizing care at each touchpoint.
An Overview of the Patient Journey
The patient journey is a term that describes the entire experience a patient has within the healthcare system.
This includes every interaction a patient has with healthcare organizations, from the initial point of contact to ongoing care and follow-up. Understanding the patient journey is important if you want to meet patient needs effectively.
When we look at the patient journey, it's essential to view it as a healthcare journey encompassing various stages and touchpoints.
This overall journey involves multiple parts of the healthcare process, all working together within a healthcare system. The healthcare landscape today is complex, and understanding the patient journey within this context helps improve the patient experience and outcomes .
Each patient journey is unique, but common elements can be identified. Organizations can better address patient needs when they examine the view of the patient throughout their interactions with healthcare providers.
This approach ensures that all parts of the healthcare system are aligned to provide the best possible care, reflecting the importance of understanding the patient journey in today's healthcare landscape.
Patient Journey vs. Patient Experience
The patient journey and patient experience are often discussed together, but they are not the same. The patient journey refers to the entire continuum of care, including every touchpoint a patient encounters within the healthcare system. This journey encompasses all events that a patient experiences, from initial contact to follow-up care.
On the other hand, patient experience focuses on the individual’s experience during these touchpoints. It's about the quality of interactions and the overall satisfaction with the care received.
A single encounter can significantly impact the patient's perception, but it is the sum of these encounters that shapes the overall healthcare experience.
Providing the best possible patient experience requires attention to each touchpoint in the patient journey. This approach ensures that patients feel valued and cared for throughout their entire continuum of care.
You should aim to understand and improve both the patient journey and patient experience so that they can create a more positive and effective healthcare experience for all patients.
Stages of the Patient Journey

These five stages of the patient's healthcare journey encompass the entire sequence of events a patient experiences.
From initial awareness to specialty care , each stage plays a crucial role in shaping patients' service and experience. Understanding these stages will help you deliver more personalized and effective care.
The awareness stage of the patient journey is where patient engagement begins. At this point, patients start to recognize their healthcare needs and seek information .
Healthcare providers play a crucial role in patient engagement during this phase. This patient engagement journey often starts with early education and awareness efforts , helping patients understand their conditions and symptoms.
Engaging consumers effectively in the awareness stage requires you to provide clear and accessible information. This helps patients make informed decisions about their health and begin their journey with confidence.
Consideration
In the consideration stage , patients evaluate their options and decide on the best course of action. Referrals from trusted sources are significant at this point, as they guide patients in their healthcare provider search. Referral texts are a popular and successful way to remind patient of the referral and to book an appointment. Meeting patient expectations is vital to ensure they feel confident in their choices.
During this stage, patients look into specific conditions and symptoms, considering factors such as scheduling an appointment and the overall reputation of healthcare providers.
Healthcare organizations need to provide detailed and accessible information to facilitate this decision-making process, ensuring patients feel supported and informed.
Acquisition/Access
During the acquisition and access stage of the patient journey, several critical elements come into play. Scheduling an appointment is often the first step.
This process can be facilitated through an automated text appointment message with a link to a patient portal , which allows for easy online booking and management. Many healthcare organizations also use a call center to handle appointments and provide necessary information to patients. Some healthcare facilities leverage HIPAA-compliant appointment text messaging to increase inbound calls and improve patient appointment volume.
Outreach efforts are essential in patient acquisition. These efforts ensure patients have the right information at the right time, aiding them in making informed decisions about their care.
Price transparency is another crucial aspect, as it helps patients understand the costs associated with receiving treatment for an illness, making the healthcare system more accessible and less daunting.
Service Delivery/Care Delivery
The service delivery or care delivery stage focuses on the patient's direct interaction with healthcare professionals. A positive care experience is vital, and it begins with the check-in and check-out processes , which should be smooth and efficient.
Interaction with healthcare professionals , including physician interaction, plays a significant role in building trust and confidence.
The discharge process must be clear and well-managed to ensure patients understand their next steps and any follow-up care needed. Billing should be straightforward and transparent to avoid any confusion or stress.
Addressing conditions and symptoms effectively is crucial in this stage, as is managing any illness or injury the patient is facing.
Ongoing Care and Patient Loyalty
Ongoing care is crucial for maintaining patient loyalty. This involves more than just regular check-ups; it includes wellness and care management tailored to individual needs .
Effective ongoing care and communication can lead to improved patient retention, as patients who feel well-cared for are more likely to stay with their healthcare provider.
Patient loyalty is built by engaging patients throughout the entire care process. This means addressing social determinants of health and focusing on population health strategies . By being proactive, you can anticipate and meet patient needs more effectively.
Preventative care is an essential component of ongoing care. It helps to keep patients healthy and reduces the need for more intensive treatments later.
In today’s healthcare environment, fostering patient engagement isn’t just a goal; it’s a necessity . Engaging patients as long as possible is more important than ever for achieving positive health outcomes and ensuring patient loyalty.
You must recognize that ongoing care and patient loyalty go hand in hand . They need to focus on these areas so that they can enhance the patient experience and improve overall health outcomes.
This approach is particularly important in today’s healthcare landscape, where patient expectations are higher and competition among healthcare organizations is fierce.
Creating a High-Quality Patient Engagement Journey

Crafting a solid patient engagement strategy is key to ensuring patients have a positive experience. When care providers prioritize giving the best healthcare, they build trust and improve patient satisfaction.
Establishing Patient Personas
Creating patient personas is a crucial step in understanding and addressing the diverse needs of patients. Only then can providers tailor their services to meet specific patient requirements.
This involves gathering detailed information about patients to form a comprehensive understanding.
This understanding patient approach helps in predicting patient behavior, preferences, and needs, ensuring a more personalized and effective patient engagement journey.
Tracking and Monitoring Patient Activity
Effective patient engagement requires continuous tracking and monitoring of patient activity . Identifying each touchpoint in the patient journey will allow you to understand critical moments of truth that significantly impact patient satisfaction.
Utilizing tools like healthcare CRM and analytics , providers can gather and analyze data to gain valuable insights. This data-driven approach ensures that healthcare organizations can respond proactively to patient needs, improving the overall patient experience.
Developing Integrated Patient Units
Healthcare organizations must strive to create integrated patient units that provide seamless care across the entire healthcare system or across providers. This integration ensures that patients receive consistent and coordinated care throughout their healthcare journey.
A well-integrated healthcare ecosystem supports value-based care , which focuses on providing high-quality care while controlling costs.
To achieve this, healthcare providers need to collaborate closely , sharing information and resources to enhance patient outcomes.
By fostering a cooperative environment, healthcare organizations can better address patient needs, improve efficiency, and deliver a more cohesive patient experience.
Encouraging Referrals and Loyalty
Building loyalty among patients is essential for long-term success in the healthcare industry. Encouraging patient engagement through various touchpoints can lead to increased referrals and patient retention. This supportive environment fosters trust and confidence.
Strategies to increase patient referrals and loyalty include personalized communication, consistent follow-up, and ensuring patients feel valued and heard.
Engaging patients throughout their healthcare journey not only improves their experience but also encourages them to recommend the healthcare provider to others, driving patient growth and satisfaction.
Patient Journey Mapping

Mapping patient journeys is essential for understanding the complete experience within the health system. To improve care, we need to understand the entire patient journey, from initial contact to ongoing care.
This approach helps identify gaps and optimize the patient experience throughout the healthcare process.
Benefits of Patient Journey Mapping
Mapping the patient journey is a valuable process that provides insights into how patients interact with healthcare organizations throughout their overall journey.
Patient journey maps provide a deeper understanding of the patient’s experience. This helps identify key touchpoints along the journey where improvements can be made.
Patient journey maps reveal critical moments in the patient's experience, allowing organizations to address gaps and enhance service delivery.
Understanding the patient’s perspective through this mapping process is essential for improving patient satisfaction and optimizing care.
Steps to Map the Patient Journey
To effectively map the patient journey, start by gathering the right data . This involves collecting information on each step of the patient’s journey, from initial contact through ongoing care.
Once you have the data, the next step is to understand the data . Analyze the touchpoints along the patient’s journey to identify patterns and areas for improvement.
Finally, take action based on your findings . Implement changes that address identified issues and enhance the overall patient experience.
Leveraging Patient Journey Data
Healthcare organizations can greatly benefit from leveraging patient journey data. By examining and utilizing this data, they can improve various aspects of patient care and operational efficiency.
Personalized Patient Experiences
Effective patient engagement is crucial for enhancing the patient experience. By analyzing patient journey data, you can create personalized patient experiences .
This means delivering the right information at the right time, tailored to individual patient needs and preferences.
Personalized patient experiences foster a stronger connection between patients and healthcare providers, leading to better health outcomes and increased patient satisfaction.
Improved Communication
Understanding patient expectations and patient needs is essential for improving communication within the healthcare system. Patient journey data can help you deliver information at the right time , ensuring that patients receive timely and relevant updates about their care.
This improved communication builds trust and ensures that patients feel informed and supported throughout their healthcare journey. When you understand the patient’s perspective, you can address their concerns more effectively.
Identifying Opportunities for Aftercare
Aftercare is an often overlooked part of the patient journey, focusing on ongoing care that continues after initial treatment. Being proactive in this stage means addressing patient needs before they become issues.
Preventative care plays a significant role in aftercare, ensuring patients maintain their health and avoid future complications.
Incorporating preventative care into aftercare strategies allows you to support patients continuously. This approach not only addresses immediate health concerns but also promotes long-term wellness.
When you put the emphasis on ongoing care, your organization can help patients manage their conditions and lead healthier lives.
Understanding and implementing effective aftercare requires a proactive mindset. You need to anticipate potential health challenges and intervene early.
This method helps in reducing hospital readmissions and improving overall patient satisfaction. Aftercare is not just about responding to issues as they arise; it's about preventing them through comprehensive, continuous care.
How Patient Journeys Improve Care

Understanding the patient journey can have tangible benefits for healthcare. When you focus on the patient journey, you can enhance patient satisfaction by ensuring each interaction is as smooth and supportive as possible.
This approach helps in identifying and addressing gaps in care , which is necessary for improving health outcomes.
Streamlining healthcare processes is another significant aspect of understanding the patient journey. When you map out each step, you can eliminate inefficiencies and make the system more responsive to patient needs. This not only improves the overall quality of care but also helps in driving patient engagement.
Today, focusing on the patient journey contributes to providing consistent care . By continuously assessing and refining the journey, you can ensure that patients receive appropriate care, leading to better health outcomes and improved patient satisfaction . This approach creates a more effective and patient-centered healthcare system.
Getting Started with Patient Journey Mapping
To begin patient journey mapping, you need to follow practical steps to ensure a comprehensive understanding of the patient experience.
According to a recent study , implementing value-based approaches in patient journey mapping can significantly enhance patient outcomes and satisfaction.
First, it's crucial to gather all relevant data from various touchpoints within the healthcare system. This involves using tools and technologies designed for healthcare CRM (Customer Relationship Management) to track and analyze patient interactions.
Healthcare marketers play a vital role in this process by providing insights into patient behavior and preferences.
Next, you should utilize these tools and technologies to create detailed patient journey maps . These maps help identify gaps in care and areas for improvement, allowing for a more personalized and efficient patient experience.
If you follow these practical steps and leverage the right tools, you’ll effectively map the patient journey, leading to better patient outcomes and a more cohesive healthcare experience.
Improve Your Patient Journey with Two-Way Texting
Revolutionize the patient journey for your healthcare institution with Dialog Health’s two-way texting solution .
Enhance every stage of the patient journey with seamless, HIPAA-compliant communication. From appointment reminders to personalized follow-up care, ensure your patients feel supported and informed.
Take the Next Step Towards Better Patient Engagement Today!
Request a Demo to see how our platform can transform your healthcare communication and boost patient satisfaction.
RELATED POSTS

24 Latest Healthcare Texting Statistics Decision-Makers Must Know for 2025

Ultimate Guide to Patient Access KPIs for Healthcare Organizations for 2025

Patient Relationship Management: Full Guide for Healthcare Organizations
Patient Journey Mapping: What it is and Why it Matters

How can healthcare organizations make every stage of the patient journey better?
How was your last experience in a healthcare facility? Think about every step of that patient care journey - the phone calls, in person meetings, wait times, communication and all of the healthcare professional/ patient interactions. It’s a lot.
Healthcare organizations are working diligently to improve patient satisfaction and quality of care by asking, “How can we make the patient experience better?” But that’s no mean feat, trying to capture the multitude of challenges patients face when navigating a healthcare journey. That makes improving it even more difficult.
A first, fundamental step to improving patient experience is understanding what that experience looks like today. This is where patient journey mapping comes into play. You can use patient journey maps to understand the highs and lows, pain points and gaps to begin pinpointing which interventions will be most impactful. Then you can assess which changes you have the power to make.
As a result, you’ll be better able to manage your patient’s journey, improve care pathways and meet—and exceed—patient expectations, needs, and wants.
What is Patient Journey Mapping?
Patient journey mapping works to identify and understand the details of all patient touchpoints within a specific healthcare experience. It helps you visualize the process patients go through to receive care, complete a treatment plan, and/or reach a desired outcome. When done correctly, patient journey maps make it easier for you to identify pain points, discover opportunities and re-align treatment and care approaches across the entire healthcare system.
What makes up a patient’s journey?
A patient’s journey represents the entire sequence of events or touchpoints that a patient experiences within a given health system, with a specific provider, or within a specific facility. These touchpoints are either virtual or in-person. They range from the mundane to the nerve-wracking or life-changing. They comprise events from scheduling an appointment online to reviewing post-surgery instructions with a doctor.
It’s key for healthcare professionals and clinicians to recognize the patient journey extends well beyond the most obvious in-person interactions at a treatment facility. The patient journey happens before, during and after a healthcare service: pre-visit, during-visit, and post-visit. These include but are not limited to:
- Finding the right service or practitioner
- Scheduling an appointment
- Submitting a list of current medications
- Arriving at the medical facility
- Identifying where to check-in.
These experiences can instil a sense of reassurance or unease before a patient even receives care. In essence, they set the tone and expectations for the physical visit. A frustrating or confusing experience during the pre-visit stage will impact the emotional state of the patient and family for the rest of their interactions.
During-visit
- Checking in at the front desk
- Waiting in the lobby to be called
- Discussion with nurses before speaking to a doctor
- Family waiting for updates in the lobby during a procedure
- Care from doctor and staff.
There are an infinite number of touchpoints during the delivery of healthcare. Each one will have a different level of impact on the patient’s experience.
- Post-care instructions at hospital
- Hospital discharge process
- Completing a patient feedback survey
- Paying for the medical treatment
- Post-surgery calls or online messages from the nurse or doctor.
The patient experience after a hospital visit plays a vital role in either reinforcing a positive experience or mitigating a negative one. Actions such as post-appointment follow-ups extend the care relationship and may help the likelihood of the patient sticking to the treatment plan
All these individual touchpoints are crucial to understand. Altogether, these positive and negative experiences — no matter how big or small — comprise the patient journey.
Who are the stakeholders?
The healthcare ecosystem is complex, involving multiple stakeholders and a wide range of internal and external factors, including:
- People (patients, their families and caregivers, doctors, nurses, administration, parking attendants, volunteers)
- Technology and systems (online registration, parking tickets, surgery updates, mobile app, website, social media)
- Facilities (hospital campus navigation, parking availability, building accessibility).
Investigation of all players and systems involved is essential to seeing the multidimensional layers impacting the experience. To do this, patient journey maps should include the perspectives of patients, providers, and staff - and those perspectives must be of the same journey. Often, an interaction that occurs from one point of view will show only one reality. However, further investigation will show the many contributing factors across the care delivery process. This is only apparent by examining multiple perspectives.
Once you understand the entire journey, with pain points, you’ll be able to identify patterns across patient personas and different demographics, and any gaps within the healthcare process. You can then begin asking important questions like:
- Which moments are most painful?
- Why do they happen?
- What must we change in order to improve the experience?
- Who must we impact?
- Which do we have the power to change?
Benefits of patient journey mapping
Patient journey mapping provides the opportunity to turn the healthcare experience from a primarily reactive experience to a proactive one. By building out care journeys for your patients, you can close any gaps in provision and establish robust preventative routines that ultimately help your patients stay healthier for as long as possible. Engaging consumers and patients based on where they are and what they want, builds trust and confidence. That retains patients in your system and encourages them to make friends and family referrals.
But how does the process work?
- Streamline patient processes and workflows: upgrading the usability and functionality of online patient portals, websites and mobile apps can put more control in the patients’ hands, increasing patient flow and cutting operational expenses.
- Increase staff efficiency : enhancing internal online tools and creating automation within systems can assist hospital staff in implementing protocols and schedules and help them anticipate and solve problems more easily. It can help to align the expected service delivery with the actual one.
- Clear routes and direction across medical facilities: hospitals can be incredibly complicated to navigate - whether it’s using the right entrance, finding parking or making your way to the cafeteria for a snack. Improving signage, making visible pathways, and using landmarks to help orient users can help patients and families readily access the resources they need.
- Improve communication between patients and providers: exchanging patient information and coordinating care can be a challenge for providers and a frustration for patients. This misalignment can be due to silos within organizations, incompatible technology systems or many other factors. Working to bridge the appropriate organizational or technological gap can help alleviate stress and anxiety.
- Develop seamless and timely patient and family updates: waiting while a family member is in surgery or communicating with a doctor to secure care for a child is typically an extremely stressful process. Families wait anxiously for updates which can be infrequent and lacking detail. Implementing a seamless system for families to communicate directly and receive regular updates, through an app or text, can help ease these pain points.
- Better ‘in-between visit’ care and check-ins with patients and families: communication between patients, including families and caregivers and providers can feel ‘hit or miss.’ Patients may be scrambling to answer phone calls or missing phone calls only to find themselves unable to get hold of the provider when they call back. Alternatively, providers are challenged to communicate critical information to a wide range of patients. Establishing better communication systems can improve patient engagement, build the patient’s confidence in the care they receive, and ease the care provider’s job.
In short, we’re talking happier patients who experience better communication and levels of empathy at every stage of the patient journey.
What tools and methods are used for creating a patient journey map in healthcare?
There are many ways to undertake patient journey mapping, but doing it well isn’t always as simple as it may seem. It’s not a single exercise, moving from A to B. It’s more complex, involving a series of tools.
Our team at Highland has helped a lot of our clients create their first journey map . Grab a bunch of sticky notes and pens to start your map. Our process tends to go like this:
- Chart the course -work out what you want to achieve (your goal); determine whose journey you’re mapping, the start and end points; create the persona(s); think about what the stages of the journey may be.
- Prepare to interview - list your potential questions being mindful that you want the interviewee to recount events rather than share opinions. Schedule interviews with a tool like Calendly. Look into other available data (such as patient feedback).
- Interviews and coding - we interview in pairs so that one can speak whilst the other takes notes. With permission, record the interviews. Afterwards, code the responses according to thoughts, actions, experience etc. We use a simple Google Sheet to do this.
- Building blocks - go through the interviews and notes. Start mapping. Use a specific color of sticky note for each Building Block and add points to the wall in their themes.
- Identify opportunities - “mine” the wall for opportunities, presenting ideas to the team. Together, prioritise the top three or four to tackle.
Repeat this whole process with another persona or goal to examine.
Explore this journey mapping process in more detail
The outcome of this process should be that healthcare professionals can look after patients better. Using patient data collection to underpin your decision-making can transform your organization’s culture to one of continuous improvement. By referring constantly to patient data, you can identify the key areas to amend and improve to better the patient experience. Satisfied customers, those who’ve experienced a near seamless patient journey, will rate your facility highly and they’ll be more likely to generate new referrals.
Improve your customer experience with Highland Solutions’ help
You may know your healthcare facility like the back of your hand, but you only know it from your informed perspective. Getting a 360º view of the patient experience is the first step to improving it. A huge challenge for healthcare leaders like you is to recognize, understand and address the fact that the overall experience is created by the cumulative interactions across the various touchpoints in the healthcare journey: pre-visit, during-visit, and post-visit.
Despite years of expertise, it’s easy for healthcare providers and leaders to develop blind spots for persistent issues in the care process. Partnering with a knowledgeable research team to conduct patient journey mapping will bring expertise and a fresh perspective to your quality of care. It’s not only about uncovering in-depth insights via patient journey maps, but also translating them into actionable strategies to help you bridge any gaps between current and emerging patient needs and the present state of your healthcare organization.
Once on the right track, you’ll be enabled to manage and grow relationships at every stage of the patient journey. The more patient-centric you become, the better experience you build, reaching a higher quality of patient care, patient retention and loyalty, and improved health outcomes and overall well-being.
Get in touch to find out more about how we can help you with patient journey mapping
“Working with Highland is a really powerful experience for a company to be able to gain insights. To have real conversations with patients unlocks new pathways, ones that may be uncomfortable and uncover change, but they empower you to move forward in a way that feels really constructive.”
Chris Whitworth, Vice President, Treatment
Download “The Essential Guide to Launching a Digital Product for Experts & Expert Firms”

The Patient Journey: A Roadmap to Wellness

In an era when patients are empowered to be as active in the healthcare field as possible, their collective voice resonates louder than ever. They actively engage in their healthcare, asking questions and asserting their right to access medical records. While their confidence grows, let’s not overlook the courage it takes to make that initial call—an outreach driven by a bodily concern.
Throughout their healthcare journey, patients often feel outside their comfort zone. It’s crucial to mindfully navigate this, carefully shaping responses to their queries. Healthcare’s increasing priority is evident, with over 60% of patients deeming wait times dreadful. They scrutinize their experiences with healthcare providers, realizing the impact on their well-being.
Research underscores the financial aspect; practices with “excellent” HCAHPS patient ratings boast a 4.7% net margin compared to 1.8% for “low” ratings. This underscores the importance of mapping the patient’s journey. As this practice gains momentum, consider it an opportunity to inspire, motivate, and create a transformative experience. Each interaction is a chance to instill confidence, provide comfort, and contribute positively to their path to optimal health.
What is a “patient journey”?
The term ‘patient journey’ describes the overall experience individuals encounter when interacting with a medical practice, whether as newcomers or established patients. It spans from their initial awareness through various touchpoints, such as word-of-mouth referrals or online searches, to the culmination of their engagement, such as leaving an online review.

Analyzing the patient journey is pivotal for a comprehensive diagnostic approach, as it reveals potential obstacles and roadblocks. To deliver an unparalleled patient experience, medical practices must grasp patient needs and preferences at each stage. Building trust is paramount, emphasizing the medical staff’s dedication to preserving patient well-being. Effective communication becomes a linchpin in elevating the patient experience , ensuring a seamless journey that fosters confidence, satisfaction, and overall health.
Which stages make up the Patient Journey?
Stage 1: discovery.
The patient’s journey begins with awareness. By self-assessing conditions and symptoms, patients initiate their healthcare quest through online searches, review sites, marketing efforts, networking, or community events. As they encounter your touchpoints—your website, call center, and ads—the journey officially starts. Ensure a robust online presence with SEO-friendly content and an optimized Google Business Profile, as 94% of patients rely on online reviews .
Stage 2: Exploration
In the consideration phase, patients weigh options based on referrals, location, insurance, accessibility, and reviews. Challenges arise if reaching the provider proves difficult. Craft patient personas for preferred communication methods, using strategies like email marketing , targeted ads, and AI chatbots to ease the decision-making process and distinguish your brand.
Stage 3: Engagement
The acquisition stage marks the patient’s decision to schedule an appointment. Direct interactions occur through phone calls, patient portals, social media, emails, and SMS. Challenges include difficulty finding appointment links, lengthy wait times, and extensive paperwork. Implement digital solutions like patient scheduling software to streamline bookings and enhance patient satisfaction .

Stage 4: Care Experience
Experienced care delivery is the focal point where traditional patient satisfaction is gauged. The emphasis shifts from online presence to quality of care. Administering treatment and meeting expectations become crucial. Utilize tools like billing or patient management software, CRM platforms, and review solicitation software to ensure top-notch care, effective data management, and feedback collection.
Stage 5: Continuous Care and Loyalty
In the ongoing care phase, retaining patients becomes pivotal. Prioritize improved communication, engage between visits, streamline appointments with digital solutions, manage your online reputation proactively, and exhibit excellent bedside manners. Personalize aftercare, track interactions, and build strong physician-patient relationships. Optimize patient experiences for better outcomes and heightened satisfaction.
Journey Mapping for Practice Growth: Why Is It Crucial?
Navigating the intricate realm of healthcare, patient journey mapping emerges as a cornerstone for medical practitioners. In the ever-evolving landscape, understanding the nuances of the patient journey becomes pivotal for sustainable practice growth. By delving into the patient journey from the outset, starting with the pivotal moment when individuals identify their health concerns, practitioners can strategically align their approach. Patient journey mapping serves as a powerful tool, offering insights that contribute to informed decision-making and ensuring each step of the patient’s path is crafted to be as pleasant as possible.
Key Importance of Patient Journey Mapping:
- Informed Decision-Making: Patient journey mapping provides a comprehensive understanding of the decision-making process, empowering patients with relevant and accurate information.
- Barriers Identification and Removal: Analysis of the patient journey allows practitioners to pinpoint and address obstacles, contributing to a smoother healthcare experience.
- Enhanced Patient Experience: Crafted interventions at each stage provide a positive patient experience, aligning interactions with individual needs and expectations.
- Practice Growth through Patient-Centric Care: Prioritizing patient journey mapping demonstrates a commitment to patient-centric care, cultivating satisfaction, loyalty, and organic practice growth .
Today, patient journey mapping isn’t just a tool; it’s a strategic approach that positions healthcare providers to adapt, evolve, and excel in delivering patient-focused care. Embracing patient journey mapping is not just about understanding; it’s about action, ensuring that every patient’s journey is a testament to the commitment to excellence in healthcare delivery.

Questions can help you build your patient’s journey map:
Question: How much does your patient know about his or her health situation? Tip: This question will help you decide your potential patients’ level of knowledge about their health situation. Is your patient well-researched?
Question: What should your prospective patients know about their situation? Tip: You can make your patients learn about their health issues by providing resources or educational material. Your patients must get a basic understanding of their illness, symptoms, and ways to address them. This process will also be helpful in establishing you as a trusted source.
Question: How severe is the illness? Is the patient feeling comfortable or in distress? Tip: Your patient may expect immediate answers or resolution if he or she is in distress. This conversation will allow you to understand the stages of illness, symptoms, emotional needs, if any, and points of pain.
Question: Is your patient scared, or in pain? Tip: Your patient could be feeling vulnerable, overwhelmed, uncertain, urgent, or hopeful.Your patient may want to know specifically how his or her health concern will be addressed.

Question: What is your patient expecting from the treatment plan? Tip: Most patients will expect an explanation or an understanding of their health issue. The most common expectation is relief or control of persisting symptoms or discomfort, and the most common disappointing outcome is being told not much can be done. Many patients expect further medical investigations and changes to the existing medication.
This conversation may make your patient feel hopeful and confident. You can help him or her get back to a normal life by reducing pain and worry.
These five questions can play a significant role in bringing your potential patient to life. By asking these questions, you can gauge your patient’s heart and mind. These questions may also help you make thoughtful decisions about the channels, touchpoints, and milestones that are most relevant to your patient’s current state and future outcome.
Patient Journey Analysis: A Maximizing Approach
Patient journey mapping is a pivotal strategic process for capturing and communicating patient interactions. This practice, when executed effectively, establishes a foundation for seamless patient experiences, fosters empowerment for both patients and physicians, and yields valuable insights for informed decisions. Key Tips for Patient Interactions:
Create Patient Personas:
- Understand patients as individuals with unique lives.
- Develop personas based on factors like gender, age, ethnicity, and lifestyle.
- Visualize the patient’s journey within the broader context of their daily lives.
Respect Without Judgment:
- Confirm assumptions and avoid unwarranted judgments.
- Recognize diverse internet usage across age groups.
- Tailor engagement strategies to different demographic preferences.
Acknowledge Caregiver Importance:
- Recognize the crucial role of unpaid caregivers.
- Address the unique stressors and concerns of caregivers.
- Tailor healthcare marketing efforts to support caregivers on their journey.
Simplify Communication:
- Avoid technical jargon in patient communication.
- Address health literacy concerns by simplifying information.
- Focus on a broad audience, considering varied levels of medical understanding.
Navigating the dynamic field of healthcare marketing, these concise yet powerful strategies underscore the importance of both patient journey mapping and the customer’s healthcare journey. They ensure personalized, respectful, and accessible interactions at every stage. By giving precedence to patient personas, embracing diverse internet usage, recognizing the pivotal role of caregivers, and simplifying communication, a collective effort is made to improve the overall patient experience and fortify the foundation of a robust healthcare practice.
Recent Posts

Sharon Mason Parker
Sharon has spent 25 years building teams and developing people to work together to help improve the client experience in the markets we serve. This ultimately benefits both customers and staff equally. Sharing best practices and ideas helps clients and team members envision new alternatives, which is quite fulfilling when positive change results. Sharon enjoys working closely with clients to understand the true drivers that are affecting their business environment. By engaging clients in meaningful exploration of their goals and challenges, she often discovers that an issue they asked for help in solving is merely a symptom of something else or something greater. Solving the real issue through truly listening and not just addressing the symptoms helps create true partnerships with clients.
Have you Assessed your Practice’s Potential to Acquire more Patients?

Most Popular Posts
- 5-Step Guide To Creating An Action Plan That Helps You Achieve Goals
- 3 Plastic Surgery SEO Tactics That Work Every Single Time
- How to Emerge Successfully from the Recession
- How to Measure Your Practice’s Email Marketing Campaign Success
- Practice Builders’ Strategic Growth and Marketing Workshop- Philadelphia
Thank you for subscribing to our Weekly Tips. We are sure that you will find them very valuable
Mail not sent due to some internal issue. Please try again.
Email already exist. Please try again with diffrent email address.
Animated Modal with Header and Footer
Have you diagnosed your practice health lately, get a complimentary your practice.
Calculates the ROI of investing in our queuing and self-service solutions Learn More
Unlock the full potential of our solutions!

- What is Patient Experience & Why It Is Importance ?
A Comprehensive Guide to Patient Journey Mapping
- Author: Wavetec
- Published: January 26, 2024
Is regulating patient experience at your healthcare service a challenging task? If your patients leave the hospital unsatisfied with the service, we have a solution for you!
Patient journey mapping is vital in understanding your patient’s experience at every step of interaction with the hospital, whether virtual or physical. This allows you to empathize with your patients, facilitate their experience, and contribute in uncertain and stressful times.
Parallel to the patient’s journey, healthcare systems face increasing challenges in patient management, regulating space constraints, limiting healthcare providers, and budgeting. By mapping the patient journey , you can pinpoint the shortfalls in your management services, improve facilities, and increase patient turnout.
The patient journey map must be curated in detail, accounting for various touchpoints and patient perceptions. The most accurate method of measuring healthcare quality is pairing patient journey maps with patient satisfaction scores, such as the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAPHPS) and a Net Promoter Score (NPS) .
Higher scores speak volumes about your healthcare services, increase patient retention, and promise returns.
What is Patient Journey Mapping?
Patient Journey Mapping is a strategic tool in healthcare that visually illustrates the entire patient experience, from initial contact to post-treatment follow-up. It involves mapping out key touchpoints and stages, such as appointment scheduling, diagnosis, treatment, and aftercare.
This process allows healthcare providers to understand the patient’s pathway through the healthcare system comprehensively.
Amidst the changing landscape of the healthcare industry, patients look for service providers that offer a personalized experience. Besides renowned healthcare providers, patients look for a human-centric environment that provides timely and efficient services.
Moreover, modern consumer requirements demand a digital transformation of healthcare services.
Healthcare managers can use patient journey maps to visualize the blind spots and pain points in a patient’s experience. A distinguished healthcare service sees journey mapping as a powerful tool that tells about a patient’s well-being and connects care providers with their emotional journeys.
You can make your practices to be more empathetic and make a difficult journey seamless.
The Benefits of Patient Journey Mapping
Investing in patient experience mapping carries benefits for both parties, care providers and patients. We have highlighted some benefits of journey mapping below:
Improved patient communication
Identifying unaddressed patient issues helps build a connection with the patient. Keeping them at the model’s center and informing them of changes before their visit reduces frustration and confusion.
Continuous patient care
With a streamlined workflow, staff members and care providers can remove uncertainties from a patient’s care journey. An integrated healthcare system removes loopholes, such as overbooked appointments, which otherwise lead to negative patient feelings.
Personalized care
Given the nature of the treatment plans and services offered by the healthcare industry, a one-shoe-fits-all theory does not apply to the consumers. By integrating patient data with business models, you can provide a customized experience to the patients.
Turn-out increases when patients receive automated appointment reminders and physician availability updates.
Improved Efficiency
Patient journey maps identify the demand for time management and sensitivity in healthcare. Feasibility arrangements such as pre-booking appointments, receiving digital laboratory reports, and online consultations boost patient satisfaction.
Patient retention and profitability
Patient feedback is crucial to introducing or revising policies, growth opportunities, and consistent revenues.

Seamless Patient Journey
With our intuitive interface, patients can easily register, check-in, and monitor their queue status. This reduces their anxiety, improves their overall experience, and fosters a positive perception of your healthcare facility.
7 Key Stages in the Patient Journey
Patient journey mapping differs for each hospital or clinic, depending on the care level. Most tertiary care hospitals identify three key stages when patients experience mapping .
Touchpoints of each step may differ slightly in pregnancies, emergency services, and outpatient departments.
Let’s read about the details of each stage below:
1. Awareness:
- This stage often begins with recognizing symptoms, changes in health, or routine checkups revealing potential issues.
- Patients may notice something is amiss, prompting them to seek further information or professional advice.
2. Consideration:
- Information gathering kicks into high gear. Patients may research their symptoms, explore potential causes, and consider various treatment options.
- Seeking advice from healthcare professionals, friends, or family members becomes a key part of this stage.
3. Decision:
- Armed with information, patients make decisions about their course of action. This could involve choosing a specific healthcare provider, deciding on a treatment plan, or committing to lifestyle changes.
- The decision-making process may also involve discussions with healthcare professionals to ensure alignment with the patient’s values and preferences.
4. Engagement:
- This is the active phase, where patients interact with healthcare providers, undergo diagnostic tests, and initiate the chosen treatment plan.
- Open communication between the patient and the healthcare team is crucial during this stage to address concerns, clarify expectations, and ensure a collaborative approach.
5. Treatment and Recovery:
- The chosen treatment plan is implemented, whether it’s medication, surgery, therapy, or a combination of interventions.
- Recovery involves monitoring progress, managing potential side effects, and adapting the treatment plan as needed.
6. Follow-Up and Maintenance:
- Post-treatment, patients often enter a phase of follow-up care. This can include regular check-ups, monitoring for recurrence, and adjusting treatment plans as necessary.
- Lifestyle changes and ongoing self-care may be emphasized to maintain health and prevent future issues.
7. End-of-Life Care (if applicable):
- In cases of terminal illness, this stage involves compassionate and supportive care. Palliative care aims to enhance quality of life, manage symptoms, and provide emotional and spiritual support.
- This stage emphasizes open communication about end-of-life preferences and ensures a dignified and comfortable experience for the patient and their loved ones.
Analyzing the Patient Journey Map
Once you have designed a patient journey map for your service, the correct way of utilizing the maps is to identify the pain points. Next, we enlist and discuss some common hurdles patients face that delay prompt care, including internal and external factors or barriers to healthcare.
1- Pre-visit
- The patient feels anxious about the medical condition.
- The website needs more information about the healthcare facility to make patients satisfied. Your website must be SEO-friendly and listed on Google to regulate patient management.
- During this stage, missed phone calls and confusing appointment scheduling tasks lead to care provision delays.
- Limited communication with consultants before visiting
2- At the healthcare facility
- Filling out the pre-appointment questionnaire is time-consuming and makes patients uneasy.
- Lengthy waiting times and mismanaged queues for appointments reduces patient satisfaction. Patients waiting at the facility can be guided using digital signage that communicates announcements, turns, and navigates around the healthcare facility.
- Explaining old symptoms and information to the same care provider at every visit frustrates patients.
3- Post-treatment plan
- Billing and initiating the hospital discharge process is often tedious.
- Receiving feedback from patients to measure patient satisfaction.
- Unable to monitor the patient at home and set up follow-up appointments creates mistrust between the patient and the doctor.
Gain valuable insights
Leverage our healthcare queue management system’s data to make informed decisions to improve the patient experience. We have seen up to a 35% increase in patient satisfaction.
Patient Journey Mapping Template
We have designed templates of patient journey maps to help you make the best one for your hospital system. As shown in the samples, patients visiting different departments have specific touchpoints. For example, a patient scheduling his appointment for the outpatient department will research the clinic and the primary caregiver.

However, the primary concern for patients requiring urgent care will be prompt ambulance services and treatment. Despite the differences, all patient journey maps are based on three key stages: pre-hospital care, in-hospital care, and post-treatment plans.

Patient Journey Improvement Solutions
If you want to enhance patient flow management and boost patient satisfaction at your hospital, we recommend using pre-engineered solutions. There are many ways to improve the quality of service you provide to your patients.
One such solution is the Wavetec patient flow system. Adopting a digital healthcare system can optimize patient-doctor interaction and improve investment returns.
We have put together the most impactful solutions your facility can sign-up for each stage of the patient journey map. Here’s what they are:
- Online appointment and booking
- Queue management – People counting, WhatsApp Queuing, Queue management applications, Digital Signage
- Patient application
- Self-check-in kiosks
- Integrated manager dashboards and analytics
- Customer feedback reports
- Curbside pickups
Let’s learn about each solution and how it will benefit your healthcare center.
1. Simplify Online Appointment Booking

Before visiting the facility, patients can schedule online appointments and ticketing on the website or patient application with their preferred physician. This service allows your patients to book seamlessly, check-in and receive wait time or canceled appointment notifications. Satisfying your customer before they arrive mitigates their already-high worry levels.
2. Patient Management

Waiting in queues for examination rooms and healthcare providers is a major source of concern for patients. You can reduce perceived wait times by giving patients a virtual waiting room. This can be done by signing up for WhatsApp Queuing and the Queue Management Mobile App. These services give patients virtual tickets and wait time notifications, allowing them to manage time effectively.

Walk-in patients and patients with pre-booked appointments can also use automated, self-service kiosks at the facility to check in or reschedule appointments. Patients can scan the displayed QR code or use biometrics technology to receive tickets via SMS, Email or WhatsApp.
You can manage the patient count in the waiting area using a real-time counter and digital signage . This helps emergency case patients to navigate the hospital without confusion.
3. Promoting Patient Satisfaction
Many patients must visit the healthcare facility multiple times to collect laboratory reports, prescriptions, and medications. You can facilitate this tedious process by providing delivery and curbside pickup options. This regulates unnecessary traffic at your hospital and saves time for patients.

Investing in Patient Applications is a great marketing tool and a one-stop solution to patient worries. Individuals can learn more about your facility’s services, access laboratory reports, initiate billing, and receive updates and reminder notifications. This is particularly useful in conducting telehealth rotations with expecting mothers and palliative care patients who cannot visit the facility often.
4. Patient Feedback

Receiving your consumer’s feedback and solving their queries ensures a successful approach to patient journey mapping. Wavetec has designed a customer feedback solution to measure customer satisfaction and follow up on your staff’s performance.
Additionally, you can get a management portal for the hospital staff and care providers. This can be integrated with patient data to give healthcare providers complete information.
Softwares such as Spectra include dashboard analytics and reports on the performance of each department to help you identify the shortfalls. This will help you build a congregated team that runs operations smoothly in the patient’s best interest.
Studies have shown that facilities using solution experience up to a 50% decrease in missed appointments, optimizing resource utilization and increasing revenue.
The modern healthcare system requires providers to be more involved in providing a seamless patient experience. In this blog, we highlight the role of patient journey mapping to help you identify touchpoints in a patient’s journey. Before, during, and after treatment, it is crucial to comprehend the patient’s viewpoint to ensure proper care.
Patient journey solutions are, therefore, integral in distinguishing your healthcare facility. Investing in patient applications, queue management software, receiving customer feedback, and analyzing it is vital in improving your standing.
Adopt our solutions, transform the healthcare industry, and make your approach more empathetic!
- No translations available for this page
- Case studies
- Expert advice
Patient journey mapping: what it is, its benefits, and how to do it
We've all been patients at some point, but our journeys were not the same. Patient journey mapping holds the key to unraveling this mystery, providing a strategic lens into the diverse pathways individuals tread throughout their healthcare experiences.
In this article, we'll explore the pivotal role of patient journey mapping in the healthcare industry, uncovering its profound benefits for both providers and patients. From amplifying patient satisfaction to streamlining operational processes, the impact is transformative.
But how does one embark on this journey of understanding and improvement? We'll guide you through the essential steps and considerations, offering insights into the art of crafting a meaningful healthcare patient journey map.
Join us as we peel back the layers of patient experience journey mapping. This powerful tool not only illuminates the complexities of healthcare but also empowers providers to reshape and enhance the patient experience.
- 1.1 Difference from other customer journeys
- 2 Patient journey mapping benefits
- 3 Patient journey stages
- 4.1 Clinical journey maps
- 4.2 Service delivery maps
- 4.3 Digital journey maps
- 4.4 Chronic disease management maps
- 4.5 Emergency care journey maps
- 4.6 Pediatric patient journey maps
- 4.7 Palliative care maps
- 5 How to do patient journey mapping?
- 6.1 Patient-centered care
- 6.2 Streamlined access to care
- 6.3 Effective communication
- 6.4 Education and empowerment
- 6.5 Care coordination
- 6.6 Technology integration
- 6.7 Feedback and continuous improvement
- 6.8 Cultural competency
- 6.9 Emotional support
- 6.10 Efficient billing and financial assistance
- 7 Templates
- 8 Wrapping up

What is a patient journey?

A patient journey is the entire process a person goes through when seeking and receiving a healthcare service. It covers everything from first noticing symptoms or realizing the need for care and medical attention to finally resolving the health issue. The journey involves patient interactions with healthcare professionals, diagnostic procedures, treatment activities, and follow-up care.
Mapping and understanding the patient journey can help boost the quality of hospital care and improve patient satisfaction. By pinpointing challenges, patient communication gaps, and areas for enhancement, care providers can refine their services to better cater to patients' needs. It also contributes to promoting patient-centered care, shifting the focus beyond just treating diseases to considering the overall well-being and experience of the patient.
Difference from other customer journeys
While the concept of patient journey mapping is similar to customer journey mapping , there are unique aspects specific to the healthcare domain. This is how a patient journey differs from any other customer journey:
- Emotional intensity. Health-related experiences often involve heightened emotions, including fear, anxiety, uncertainty, a sense of losing control, and a dependence on others. The emotional aspect is more pronounced in patient journeys compared to customer journeys in most industries.
- Complexity and uncertainty. Healthcare journeys often involve multiple stakeholders, various diagnostic and treatment options, and inherent uncertainties. Navigating these complexities requires a different approach compared to more straightforward consumer experiences. Comparing buying eyeglasses online and visiting a doctor — both are experiences, but how different they are!
- Regulatory and ethical considerations. Healthcare is heavily regulated, and ethical considerations play a significant role there. Patient journeys must align with regulatory standards and ethical principles that other industries don’t have.

- Clinical decision points. Patient journeys involve critical clinical decision points, such as diagnosis and treatment choices. These decisions not only impact the patient's health but also influence the overall trajectory of the journey.
- Care continuum. Patient journeys often extend beyond a single episode of care. They may involve long-term management, follow-up appointments, and ongoing support, creating a continuous care continuum.
- Interdisciplinary collaboration. Healthcare is often delivered by a team of professionals from different disciplines. The patient journey may involve collaboration among physicians, nurses, specialists, and other healthcare providers.
Patient journey mapping benefits

Mapping a patient journey offers a range of benefits that contribute to improving the overall quality of healthcare delivery. Here are some key advantages:
- Visualization of the entire patient journey helps healthcare providers identify critical patient journey touchpoints that impact patient satisfaction and experience and require immediate attention. By paying more attention to these touchpoints, you ensure a more positive overall journey.
- Gaps in care and challenges are highlighted among healthcare professionals. Addressing these issues ensures a more seamless and collaborative approach to patient care.
- Pain points and barriers become evident, enabling healthcare providers to proactively address issues that may hinder effective care delivery.
- Understanding individual patient journeys allows for more personalized ongoing care plans. Tailoring interventions to specific needs and preferences improves patient engagement and outcomes.
- By mapping a patient journey, you can identify resource-intensive stages and areas where efficiency can be improved, enabling a healthcare organization to allocate resources more effectively.
- It's a great way to identify opportunities for smoother transitions between different stages of care, ensuring continuity and preventing gaps in treatment.
- It becomes clear where patient involvement in the decision-making process can contribute to their healthcare journey.
Example: Tom, recovering from surgery, feels more empowered as his healthcare team provides clear post-operative care instructions, making him an active participant in his recovery.
In summary, patient journey mapping provides a comprehensive framework for healthcare improvement, addressing specific challenges at each stage and leading to tangible enhancements in patient experience, communication, and overall care delivery.
Patient journey stages
Patient journeys can differ, and if we take a broad perspective, some key stages would include:
Awareness
This stage involves the patient recognizing symptoms and becoming aware of a potential health issue.
- Key considerations: Pay attention to how patients identify and interpret their symptoms, as well as the information sources they consult.
Example: John notices persistent joint pain and, through online research, suspects it might be arthritis. His journey begins with a heightened awareness of his symptoms.
Seeking information
Patients actively look for information to understand their symptoms, potential causes, and the importance of consulting a healthcare professional.
- Key considerations: Review the information sources patients use and how well they understand the need for professional medical advice.
- Example: Emily researches her persistent cough online, learning about various respiratory conditions and recognizing the importance of seeing a doctor for an accurate diagnosis.
First contact
This marks the initial interaction with the healthcare system, typically through scheduling an appointment with a primary care physician.
- Key considerations: Assess the ease of access to healthcare services and the patient's initial experience with medical professionals.
- Example: Alex schedules an appointment with his family doctor to discuss recent changes in his vision, initiating his journey within the healthcare system.
Diagnostic process
Patients undergo diagnostic tests to identify the root cause of their symptoms.
- Key considerations: Examine the efficiency of the diagnostic process and the clarity of communication about the tests.
- Example: Maria undergoes blood tests and imaging to determine the cause of her abdominal pain, marking the diagnostic phase of her journey.
Treatment planning
Patients receive a diagnosis, and healthcare providers collaborate on creating a personalized treatment plan.
- Key considerations: Evaluate how well the diagnosis is communicated and involve patients in treatment decisions.
- Example: Emily receives a diagnosis of rheumatoid arthritis. Her healthcare team takes the time to explain the condition, discusses various treatment options, and actively involves her in deciding on a comprehensive plan that combines medication, physical therapy, and lifestyle adjustments.
Treatment and clinical care service
Patients initiate the recommended treatment plan, experiencing the day-to-day challenges and improvements associated with their patient journey in a hospital.
- Key considerations: Monitor treatment adherence, side effects, and the patient's overall experience during this active phase.
- Example: Sarah starts chemotherapy for her cancer, navigating the treatment process with the support of her healthcare team.
Psychological support
Patients deal with the emotional toll of managing a health condition, including anxiety, frustration, or isolation.
- Key considerations: Acknowledge and address the emotional aspects of the journey, providing resources for mental health support.
- Example: James copes with the emotional challenges of managing chronic pain, seeking counseling to navigate the psychological impact.
Regular checkups
Patients undergo routine checkups to monitor their health status and adjust treatment plans as needed.
- Key considerations: Ensure consistent communication and scheduling of regular checkups to track progress and address any emerging issues.
- Example: Sarah, diagnosed with hypertension, attends regular checkups where the healthcare team monitors blood pressure, discusses lifestyle adjustments, and ensures medication efficacy. The routine checkups create a proactive approach to managing her condition.
Patients provide feedback on their experiences, allowing healthcare providers to refine and tailor their care.
- Key considerations: Establish mechanisms for patients to share feedback easily and transparently, encouraging an open dialogue.
- Example: John shares his experiences with a new treatment plan, providing feedback on its effectiveness, side effects, and overall impact on his daily life. This feedback loop allows the healthcare team to make timely adjustments and improve the patient's journey.
The stages may vary based on diverse scenarios and individual health circumstances. For instance, when a patient undergoes surgery or faces an acute medical event, the trajectory of their journey can diverge significantly from a more routine healthcare experience.
Factors such as the need for emergency care, hospitalization, and specialized interventions can introduce unique stages and considerations. Additionally, variations may arise due to the specific nature of medical conditions, treatments, and the individual preferences and needs of patients.
Recognizing this variability is crucial for comprehensive journey mapping, allowing for a more nuanced understanding of the patient experience across different healthcare contexts.
Types of healthcare journey maps

Healthcare journey maps can take various forms depending on their focus, purpose, and the specific aspects of the patient experience they aim to understand.
Here are a few types of healthcare journey maps:
Clinical journey maps
Focus: Emphasize the clinical aspects of a patient's experience, including diagnosis, treatment, and recovery.
Purpose: Help healthcare providers understand the medical processes and interventions involved in the patient's journey.
Example: A clinical journey map for a cancer patient would detail the steps from initial symptoms to diagnosis, treatment modalities, and post-treatment care.
Service delivery maps
Focus: Highlight the various touchpoints and services a patient encounters throughout their healthcare journey. Then, detail the back and front processes your team does or has to do during each stage.
Purpose: Enable healthcare organizations to assess the efficiency and effectiveness of service delivery.
Example: Mapping the service delivery for a patient undergoing surgery, including preoperative consultations, surgical procedures, and post-operative care.
Digital journey maps
Focus: Examine the patient's interaction with digital tools and technologies, such as online portals, mobile apps, and telehealth platforms.
Purpose: Help improve the digital aspects of patient engagement and communication.
Example: Mapping the patient's journey when using a telehealth platform for virtual consultations, prescription refills, and accessing medical records.

Chronic disease management maps
Focus: Explore the long-term journey of patients managing chronic conditions.
Purpose: Aid in understanding the challenges and opportunities for supporting patients in their ongoing self-management.
Example: A journey map for a diabetes patient would encompass regular monitoring, medication management, lifestyle adjustments, and periodic checkups.
Emergency care journey maps
Focus: Examine the patient’s experience during emergencies, from the onset of symptoms to emergency room admission and follow-up care.
Purpose: Help optimize response times, communication, and the overall emergency care process.
Example: Mapping the journey of a patient experiencing chest pain, from the initial call to emergency services to the triage process and subsequent cardiac care.
Pediatric patient journey maps
Focus: Tailored specifically for the unique needs and considerations of pediatric patients and their families.
Purpose: Address the emotional and practical aspects of pediatric healthcare experiences.
Example: Such a map is good for a child undergoing surgery to consider the role of parents, age-appropriate communication, and post-operative care.
Palliative care maps
Focus: Center on the patient's journey when facing serious illness, with a focus on providing comfort and support.
Purpose: Enhance the quality of life for patients and their families during end-of-life care.
Example: This kind of journey map suits a patient receiving palliative care when considering symptom management, emotional support, and coordination of services.
The mentioned types of maps cover different patient scenarios and clinical cases. There can also be "AS-IS" and "TO-BE" maps, reflecting the current state of the journey and the desired one, respectively.
All these types of healthcare journey maps offer a nuanced understanding of the diverse aspects of patient experiences, allowing healthcare providers and organizations to tailor their services to meet the unique needs of different patient populations.
How to do patient journey mapping?

Mapping a patient's journey is a thorough process that needs careful planning, teamwork, and analysis. Here's a guide on how to do it:
- Define the objectives
Clearly articulate the goals of the patient journey mapping exercise. Determine what aspects of the patient experience you want to understand and improve. All involved parties should be aware of these goals and agree with them.
- Assemble a cross-functional team
Form a team that includes representatives from various departments, including healthcare providers, administrative staff, patient advocates, and anyone involved in the patient experience.
- Do research
Conduct thorough research to gather quantitative and qualitative data related to the patient experience. This may involve analyzing patient records, studying existing feedback, diving into analytics and market research, and reviewing relevant literature on best practices in healthcare.
- Select a patient segment
Identify a specific patient segment or persona to focus on. This could be based on demographics, health conditions, or specific healthcare services.
Tip: You can leverage your segments or patient personas to craft an empathy map , which is particularly valuable in healthcare.
- Conduct stakeholder interviews
Interview stakeholders, including healthcare professionals and administrative staff. Gather insights into their perspectives on the patient journey, pain points, and opportunities for improvement.
- Define the stages
Outline the patient journey by mapping out each stage and interaction with the healthcare system. This can include pre-visit, during a visit, and post-visit experiences.
Tip: To speed up the process, run a journey mapping workshop with your team. It will help with the next step, too.
- Create the patient journey map
Develop a visual representation of the patient journey. This can be a timeline or infographic that illustrates each stage, touchpoint, and the emotional experience of the patient.
- Identify pain points and opportunities
Analyze the collected data to pinpoint pain points, areas of friction, and opportunities for improvement. Consider emotional, logistical, and clinical aspects of the patient experience.

- Review and validate
Consider collaborative journey mapping . Share the draft patient journey map with stakeholders, including frontline staff and patients, to validate its accuracy. Incorporate feedback to ensure a comprehensive and realistic representation.
- Develop actionable plans
Generate specific, actionable plans based on the identified pain points and opportunities. Each initiative should be feasible, considering resources and organizational constraints.
- Prioritize and implement changes
Prioritize the recommendations based on impact and feasibility. Begin implementing changes that address the identified issues, whether they involve process improvements, staff training, or technology enhancements.
- Monitor and iterate
Continuously monitor the impact of implemented changes. Gather feedback from both staff and patients to understand the effectiveness of the improvements. Iterate on the patient journey map and make recommendations as needed.
- Measure your success
You can also establish KPIs to measure the success of any improvements made based on the patient journey mapping insights. These could include patient satisfaction scores, reduced wait times, or improved communication metrics.
- Document insights (optional)
And keep a record of the lessons learned during the patient journey mapping process. This documentation can inform future initiatives and contribute to ongoing efforts to enhance the patient experience.
- Promote a culture of continuous improvement
Foster a culture within the organization that values continuous improvement in patient care. Encourage ongoing feedback and regularly revisit your journey map to ensure its relevance over time.
By following these steps, healthcare organizations can gain valuable insights into the patient experience, leading to targeted improvements that enhance healthcare quality and patient satisfaction.
How to improve the patient journey?

Striving for a seamless patient journey involves enhancing the overall experience that individuals have when seeking and receiving healthcare services. Here are some strategies to consider:
Patient-centered care
- Prioritize patient needs and preferences.
- Emphasize education and empower patients to actively participate in their healthcare journey.
- Foster open communication and active listening.
Streamlined access to care
- Reduce wait times for appointments and procedures.
- Implement online scheduling and appointment reminders.
- Provide options for virtual consultations when appropriate.
Effective communication
- Ensure clear and understandable communication with patients.
- Provide information about treatment plans, medications, and follow-up care.
- Confirm that patients are well-informed about the potential risks and benefits of treatment options.
Education and empowerment
- Offer educational resources to help patients understand their conditions and treatment options.
- Encourage patients to actively participate in their health management.
- Provide tools for self-monitoring and self-management when possible.
Care coordination
- Improve collaboration and communication among healthcare providers to strengthen care coordination, ensuring a more cohesive and seamless experience for patients throughout their healthcare journey.
- Define and implement standardized protocols for communication and handovers between care teams, reducing the risk of errors and ensuring continuity of care.
- Implement remote monitoring technologies to track patients' health remotely, enabling timely interventions and reducing the need for frequent in-person visits.
Technology integration
- Adopt electronic health records (EHRs) for efficient information sharing.
- Use telemedicine to enhance accessibility and convenience.
- Implement mobile health apps for appointment reminders, medication management, and health tracking.
Feedback and continuous improvement
- Conduct regular surveys to gather specific insights into patient satisfaction, allowing for a more nuanced understanding of their experiences.
- Establish easily accessible channels for patients to provide real-time feedback, ensuring that their voices are heard promptly.
- Respond promptly to patient feedback, address concerns, and communicate any changes or resolutions, fostering a sense of responsiveness and accountability.
Cultural competency
- Train healthcare staff to be culturally competent and sensitive to diverse patient needs.
- Promote diversity in healthcare staff to reflect the communities served, fostering a more inclusive and culturally sensitive environment.
- Recognize and celebrate cultural awareness events within the healthcare setting, fostering an inclusive atmosphere that appreciates the richness of diverse traditions.
Emotional support
- Address the emotional and psychological aspects of healthcare.
- Provide resources for mental health and emotional well-being.
- Consider support groups or counseling services.
Efficient billing and financial assistance
- Simplify billing processes and provide clear information about costs.
- Offer financial assistance programs for patients in need.
- Communicate transparently about insurance coverage and out-of-pocket expenses.
Staff training:
- Train healthcare staff in patient-centered communication and empathy.
- Ensure staff is knowledgeable about the resources available to patients.
- Foster a culture of empathy and compassion in the healthcare environment.
By focusing on these aspects, healthcare providers can contribute to a more positive and effective patient journey. Regularly reassessing and adapting strategies based on feedback and evolving healthcare trends is crucial for ongoing improvement.
UXPressia already has some healthcare journey map examples:
- Surgical patient journey
This map focuses on the healthcare journey of a patient persona, Robin, from the moment when the patient understands that something is wrong to the recovery period. This journey is long and very detailed.
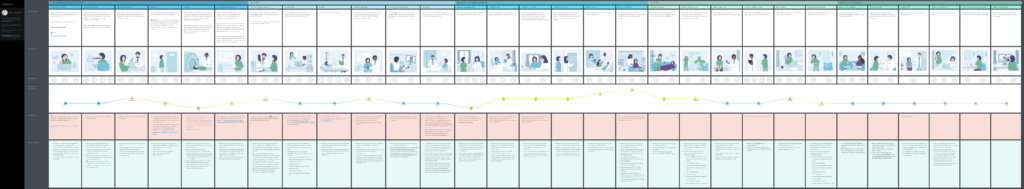
- Non-surgical patient journey
This map visualizes the journey of a patient, Lotta, who decides to undergo a checkup at a hospital. She schedules a visit, gets a consultation, takes some tests, and starts taking some medicine prescribed by her doctor.
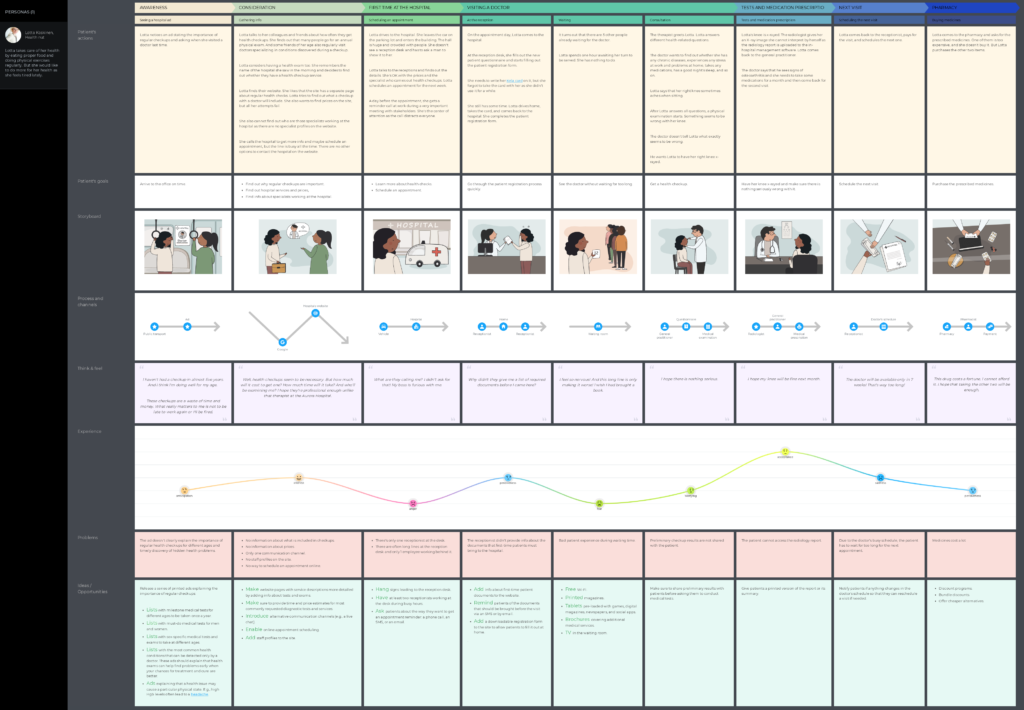
More healthcare and well-being templates are available in our library.
Wrapping up
In wrapping up, think of patient journey mapping as a powerful tool reshaping the healthcare landscape, with the patient's experience taking center stage. It's like creating a roadmap that intricately traces every step of a patient's interaction within the healthcare system.
This deliberate mapping isn't just a plan; it's a compass guiding healthcare organizations toward key points where they can enhance patient satisfaction, simplify access to care, and cultivate a more compassionate and patient-focused healthcare environment. Investing in patient journey mapping is more than a strategy—it's a dedication to raising the bar in care quality, amplifying the patient's voice, and ensuring that every leg of the healthcare journey is characterized by empathy, understanding, and an unwavering pursuit of excellence in patient experience.
Related posts
Rate this post

Journal for Practice Managers
- All Articles
- Case Studies
What is the Patient Journey?
Why is patient journey mapping important, advantages of patient journey mapping, what does a patient’s journey consist of, what are the steps of a successful patient journey, patient journey mapping: what is it & why does it matter.

Without a doubt, patient satisfaction is the cornerstone of any medical practice’s success.
After all, it improves patient retention and increases the likelihood of patients recommending your healthcare practice to their family and friends.
But, let’s be honest, providing patient satisfaction is easier said than done. With your patients likely having different expectations, ensuring that each and everyone is satisfied with your services can be quite a challenge.
Well, with patient journey mapping, meeting patient expectations and improving the patient experience becomes much easier!
Learn how to simplify your practice workflow and free up more time for patients with Medesk.
Not sure what patient journey actually is or how to use patient journey mapping to enhance your medical practice?
We’ve got you covered. In this article, you will learn:
Put simply, a patient journey defines the entire experience a patient goes through during their medical treatment at your healthcare facility.
As such, the patient journey covers the whole medical process (virtual and in-person), from developing symptoms and scheduling a doctor’s appointment to completing the medical treatment and beyond.
Patient journey mapping, in turn, gives a detailed overview of all the stages a patient goes through during their entire interaction with a specific healthcare facility. In turn, this helps healthcare providers to improve patient experience and increase patient satisfaction.
Medesk helps automate scheduling and record-keeping, allowing you to recreate an individual approach to each patient, providing them with maximum attention.
Patient journey mapping is vital to the success of your medical practice as it helps you to:
- Manage and meet patient expectations .
- Identify your medical practice’s weak spots, which allows you to effectively improve your medical practice.
- Get valuable insight and evaluate your medical practice from the patient’s perspective.
- Create a personalized, hyper-targeted patient experience.
- Effectively allocate your budget to improve your medical practice’s efficiency and performance.
- Deliver successful treatment outcomes by improving your healthcare quality.
- Increase patient engagement and patient satisfaction, leading to better patient retention .
Patient journey mapping has numerous advantages for healthcare providers and patients alike, including:
- Seamless, comprehensive, and continuous patient care . Patient journey mapping allows you to identify gaps and blind spots that bring down the quality of your healthcare services such as ineffective use of medical technology.
- Effective communication between healthcare providers and patients . Patient journey mapping allows you to improve communications by helping you spot and solve communication issues, such as inconsistency, lack of clarity, insufficient medical updates, and more.
- Clinical workflow optimization . Patient journey mapping can help you assess and optimize your clinical workflow and processes to deliver high-quality care for your patients, improve treatment outcomes, and increase patient satisfaction.
- Healthcare efficiency . By optimizing your clinical workflow, providing staff with clear instructions, and improving communication between patients and healthcare providers, patient journey mapping helps to improve your medical practice’s efficiency and performance.
- Patient retention . Patient journey mapping can effectively improve patient retention rates by promoting clear communication, improving treatment outcomes, and ensuring an excellent patient experience. In turn, patient journey mapping builds trust and loyalty, which can encourage patients to refer your medical practice to family and friends.
- Improved staff performance . Patient journey mapping can help you to optimize internal processes and online tools, allowing for more automation. This way, patient journey mapping can improve your staff performance and efficiency.
- Stress and anxiety reduction . By helping to bridge communication gaps, optimize workflows, and more, patient journey mapping helps to alleviate stress and anxiety. For example, patient journey mapping can improve your patient and family update system, allowing patients and family members to get medical updates via text.
- Effective patient flow management . Patient journey mapping allows medical practices to optimize and manage patient flow by ensuring smooth admission, procedure scheduling, and discharging processes.
As we mentioned above, the patient journey covers the entire patient experience.
That being said, the patient journey doesn’t simply refer to the typical interaction between a patient and a healthcare provider. Instead, it also encompasses the patient experience before and after their visit to the healthcare facility.

In essence, the patient journey consists of three main stages, which include:
- Pre-visit stage
- During-visit stage
- Post-visit stage
So, let’s take a closer look at each of them.
Pre-visit Stage
The pre-visit stage is the beginning of a patient journey, which can include:
- Noticing symptoms and self-assessing the health condition
- Researching symptoms, healthcare services, and more
- Browsing the Internet to find a healthcare practitioner
- Scheduling an appointment (in-person, online, or via phone call)
- Navigating the healthcare facility upon initial arrival
Put simply, the beginning of the patient journey sets the tone and expectations for the whole patient experience.
A confusing and complicated pre-visit experience, for example, can lead the patient to experience stress, discomfort, confusion, frustration, and anxiety.
For this reason, it’s important to make sure that the patient journey begins with a positive pre-visit experience, as it can impact the patient’s emotional state and well-being and thus affect the patient’s future interaction with the healthcare facility.
During-visit Stage
The during-visit stage covers the entire patient experience at your healthcare facility upon the patient’s arrival, including activities such as:
- Checking in, either at the front desk or at a self-service kiosk.
- Waiting for the appointment in the waiting room.
- Interacting and communicating with the staff, including front-desk, nurses, doctors, etc.
- Receiving healthcare treatment.
- Updating family members on the patient’s condition and treatment.
By making sure that your patients have a positive experience during their visit, you can improve patient satisfaction, reduce patient dropout rates, and improve treatment outcomes.
Post-visit Stage
Although the post-visit stage often gets the least attention, this last stage of the patient journey is crucial to improving patient retention.
The post-visit stage includes the following:
- Instructing patients on aftercare
- Discharging patients from the hospital
- Receiving and analyzing patient feedback
- Paying for the healthcare services
- Follow-up appointments
Essentially, optimizing the post-visit stage of the patient journey ensures patient retention, successful treatment outcomes, patient satisfaction, and an overall positive patient experience.
Discover more about the essential features of Medesk and claim your free access today!
Using practice management software is one of the most important steps you can take to ensure a successful patient journey.
That’s because a well-designed practice management software comes with many tools and features that can tremendously improve each stage of the patient journey, such as:
- An online booking tool that can facilitate appointment booking and scheduling procedures, thus creating a positive experience before the visit.
- A medical billing tool can automate the payment procedures, which improves the patient experience during the visit.
- An integrated telemedicine software can be used to conduct follow-up appointments remotely, which promotes a successful patient journey after the visit by helping patients save time.
Not to mention, using practice management software optimizes your medical practice’s overall performance and efficiency, which can significantly boost patient satisfaction.

That being said, here are four additional steps you can take to ensure a successful patient journey at each stage:
- Optimize your healthcare website . For a positive pre-visit experience, take advantage of healthcare SEO . Optimizing your medical website for search engines allows your patients to easily find information about your healthcare services, medical practitioners, and more.
- Improve hospital wayfinding . Place hospital maps and navigation signs (e.g. for entrances, exits, parking, cafeteria, etc.) to help your patients find their way around your hospital. This can alleviate stress and save time , thus improving the patient experience.
- Upgrade your waiting room . For most patients, waiting is the most stressful part of visiting the doctor’s office . To provide a better waiting experience for your patients and their families during their visit, consider improving your waiting room .
- Collect and analyze patient feedback . Patient feedback surveys can reveal opportunities for improvement. For example, if many patients are unhappy with your receptionist’s communication , consider trying medical staff training .
And that’s all!
By now, you should have a better understanding of patient journey mapping.
Before you go, however, let’s quickly go over some of the key points of this article:
- The patient journey represents the entire experience a patient has at your medical practice, including before, during, and after receiving medical treatment.
- Patient journey mapping allows healthcare practitioners to get insight into their medical practice from the patient’s perspective, which helps to make necessary improvements.
- Patient journey mapping brings numerous advantages to both medical practices and patients, some of which include improved communication between healthcare providers and patients, optimized clinical workflows, and improved patient retention.
- Using practice management software can improve all stages of the patient journey.
- Improving hospital navigation, optimizing your practice’s website, collecting patient feedback, and upgrading your waiting room can help to ensure a successful patient journey.
Sign up for free
Create your free account and start your journey with Medesk today.
Should You Charge Your Patient’s a No-Show Fee? Pros & Cons
6 top medical practice management software for your practice in 2024, how to start a physical therapy clinic in 2024 [10 easy steps].
- Online Booking
- Electronic Health Records
- Consultation Form Templates
- Integration
- Task Management
- About Company
social media

What is patient journey mapping
Patient journey mapping — also called user journey mapping in healthcare — is an exercise for medical startup owners and developers to create a visual trip of the patient across the solution and come up with a seamless patient journey.
The key idea is to construct a patient experience that encompasses all aspects of the patient’s interaction with the startup, its services, and the product. It includes what users think and feel about the platform.
To create a patient journey map , you need to come up with every step patients would take in the app to reach their goals.
The goal of the process is to get more competent about how patients will interact with your platform, and what they expect and think.
Here is an example of an average healthcare journey:
Key benefits of a patient journey map
More than 79% of marketing leads don’t convert into sales and customers, according to the MarketingSherpa report. The main reason for this is a lack of information about the needs of the user based on who they are and where they are in the interaction. It means that even if your marketing strategy is eye-catching and effective, without knowledge about your user, the platform has little chance of being successful.
Creating a patient journey map can directly and significantly impact user experience on your healthcare platform. Here is the list of 5 benefits of patient journey mapping for web and mobile apps.
Patient journey mapping:
- Creates personalized patient experiences;
- Lets you determine unmet user needs and identify pain points;
- Aligns your organization and stakeholders with a common view of the patient experience;
- Helps measure gaps between the intended experience for your patients versus the actual experience;
- Assists with breaking down and understanding complex journeys across multiple touchpoints.
4 types of patient journey maps
To purposefully design patient experience and create a healthcare journey, you will need to choose a type of map. The choice usually depends on the time and priorities you have, as well as the level of engagement of your stakeholders.
To get a better idea, check out these 4 examples of the most popular types of a patient journey map and 4 templates you can reuse for your startup:
Current state maps . The current state healthcare journey map is a “snapshot” of how things are today. It depicts how a patient interacts with a product and shows the weaknesses and strengths of the experience. It’s the most common and easy-to-create type of map but not very strategic.
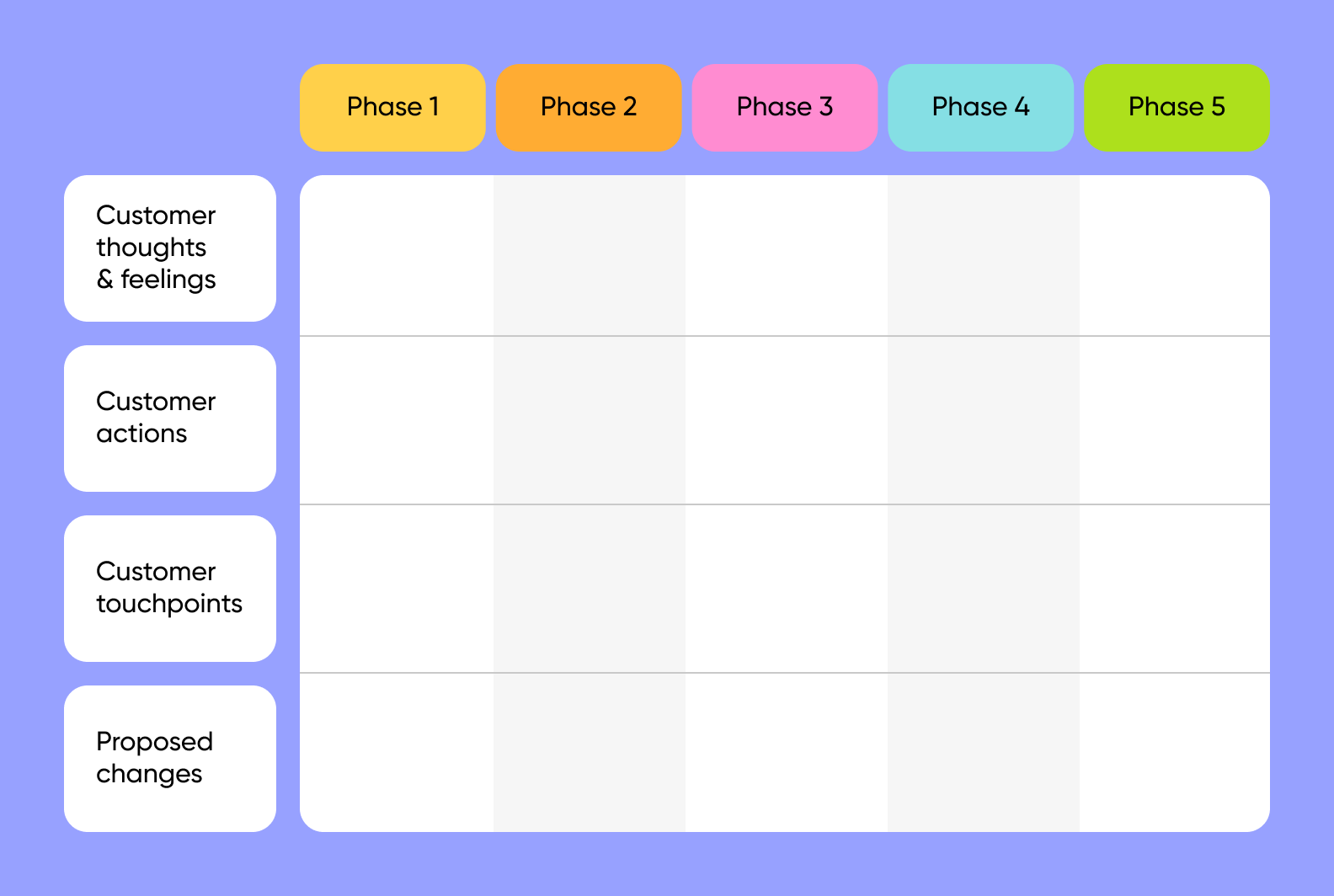
To fill in our template, you have to describe every step of the journey with the customer’s thoughts, actions, and touchpoints (when and how they come in contact with your solution), as well as proposed changes.
Future state maps . Such maps present an ideal situation. It’s a “dream” version of a patient journey map that highlights innovation and bold ideas for improvement. Future state maps are built based on current state maps, but they are free of existing constraints and limitations. This type of map is important for strategic planning and UI/UX improvements.
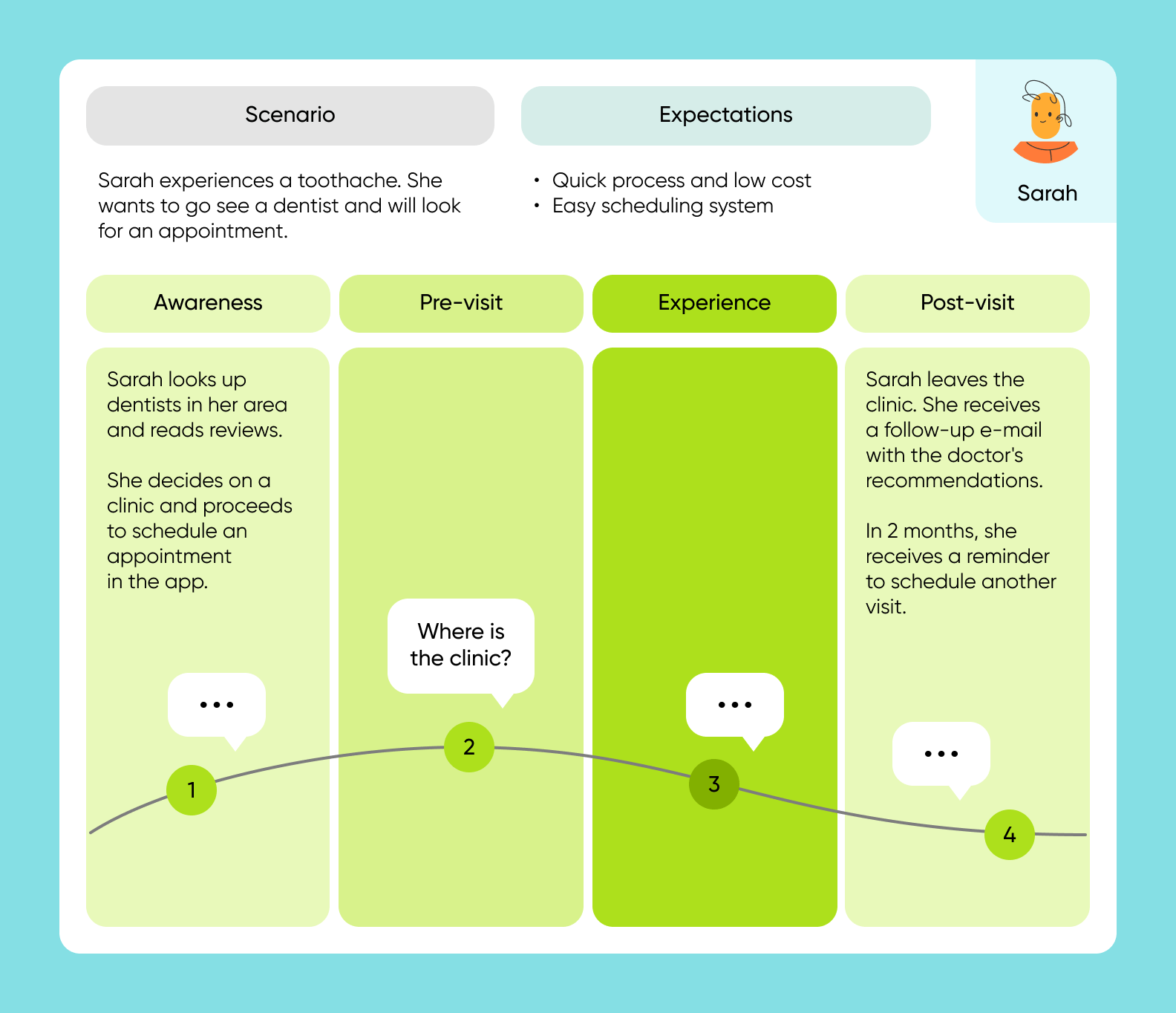
To create a future state map, you need to come up with a dream scenario and patient expectations a customer would have. Break them down into awareness steps, pre-visit, experience, and post-visit, and add the user’s actions for each.
Day-in-the-life maps . Day-in-the-life maps show everything patients think, feel and do during the day. This type is similar to current state maps, but there is a difference. Day-in-the-life journey is not limited by your product, it includes everything a user does inside and outside of a healthcare service.
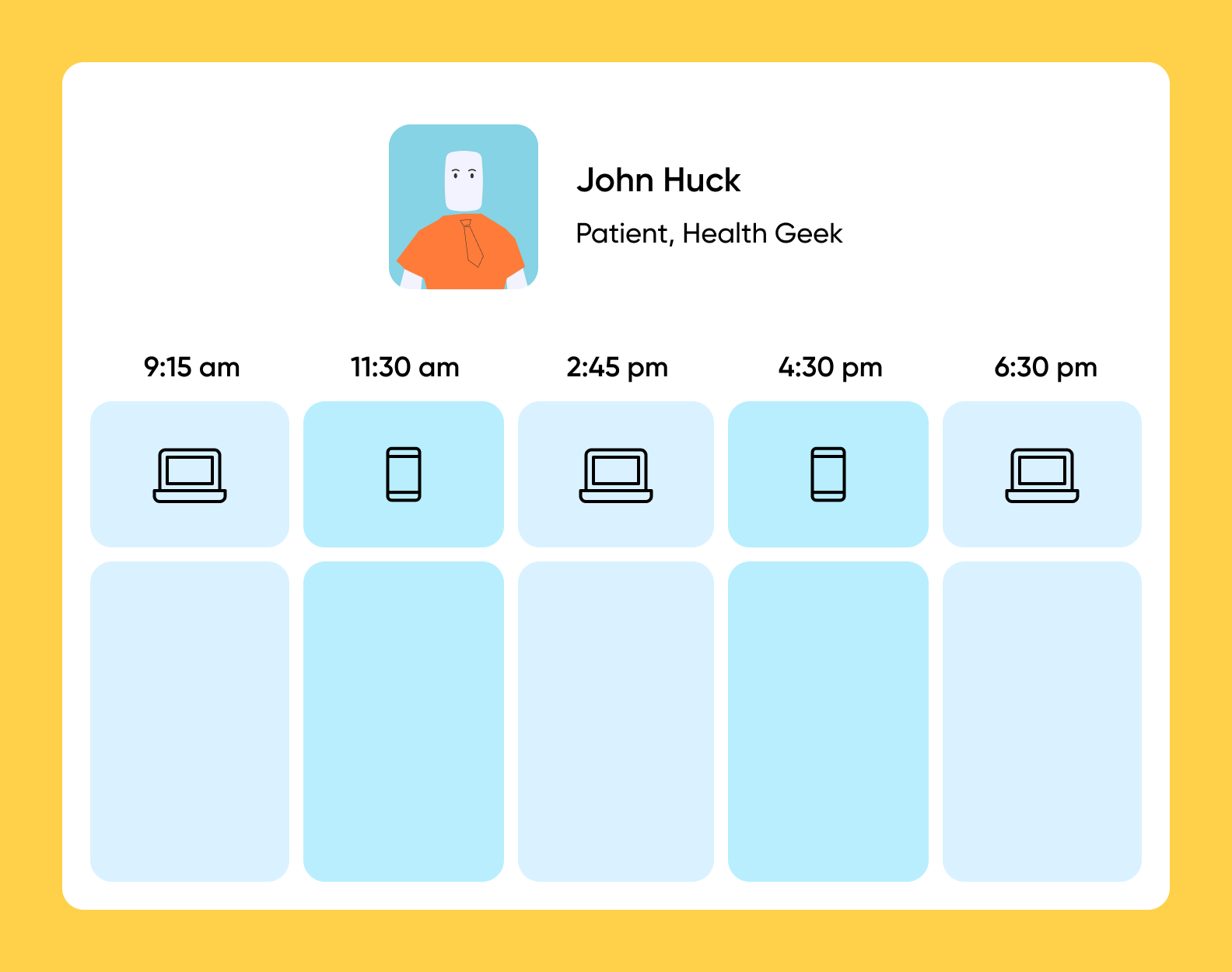
To fill in the day-in-the-life map, imagine how the journey of your customers goes from the moment they wake up till the time they go to bed. Describe each step with details.
Service blueprint maps . Those are not exactly the patient journey maps but a visual layout of administrative systems and tools required to deliver a great user experience at every step. It breaks down what’s happening behind the scenes of patient flow and what resources are used to support a patient’s journey.
Service blueprint maps can include the company’s mission and vision, employees, technology, customer activity, internal and external factors, and backstage actions. Service Blueprint can help you not only understand who your patients are but also how you can operate better and grow the business internally.
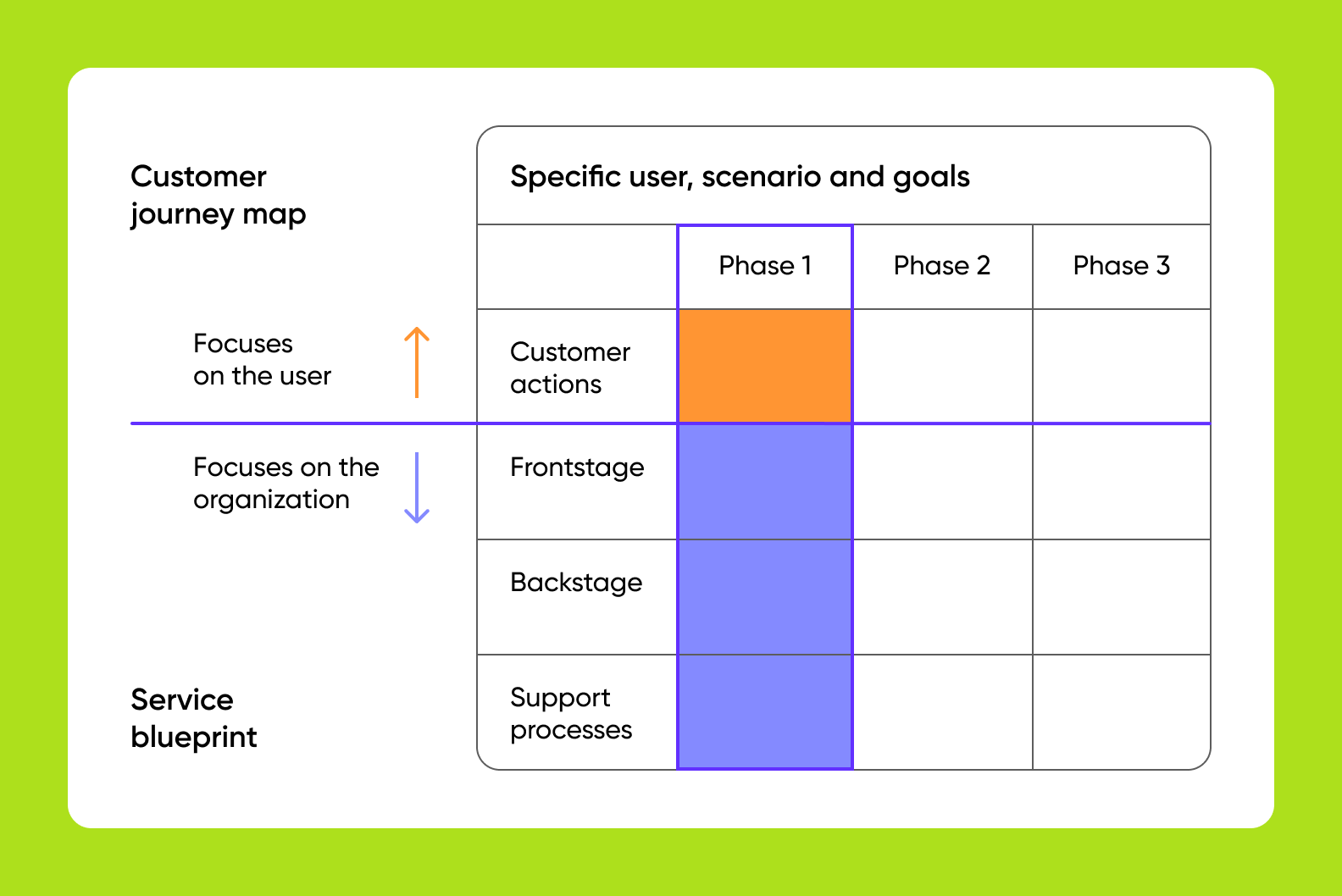
To create a service blueprint, get the simple customer journey map, and for each step, add frontstage and backstage actions that happen to support the user’s journey.
6 steps to create a patient journey map
Patient journey mapping requires a lot of knowledge about the patients. Without understanding your customers and their needs, finding gaps and growth opportunities can be very challenging.
To help you approach mapping the patient journey, we put together a 6-step guide to creating an effective and useful map.
Step 1: Define goals and the scope of the map
First things first, you will need to identify the goal and the type of the map.
In the healthcare industry especially, positive patient experience is tied to transparency and clarity during the process. When users deal with health issues, the last thing they want is confusing navigation.
To build a path from A to B and make sure all stakeholders are on the same page, you will need to define end results, main objectives, and key points of patient journey mapping. See our list of questions to ask to get started with the process.
❓Questions to ask:
- What is the purpose of creating the map? What are the expected results from the process of patient journey mapping?
- What type of patient journey maps will we use?
- How will we know our end goal is achieved? What success looks like?
Step 2: Create patient personas and do user research
A patient persona or a user persona — is a fictional character that represents a segment of users with similar needs and traits. It can be based on your current or ideal customers, depending on the type of map you choose to create.
Patient persona profiles should include demographic information (age, race, marital status, income), habits, goals, common pain points, and motivations. You can be as detailed as possible and add any patient data that is relevant to your healthcare solution, from needs and frustrations to coffee preferences and favorite brands.
- What are the types of users that will interact with your app?
- What are the reasons why patients will use this healthcare service?
- How often do they interact with healthcare providers? What are the pain points of this interaction?
- How is your startup helping them overcome their challenges?
Step 3: Map the patient’s touchpoints
Next, we recommend mapping every step of a patient’s journey, including the first interaction, pre-visit services, treatment, and post-visit. The touchpoints will include every interaction with your healthcare service. All this information will become the backbone of your healthcare experience.
To make the most out of patient journey maps, you can include information about the user’s emotional state at each touchpoint and ideas for potential changes. This way, when you return to the map in the future, you will reconstruct what users feel and think about the solution at each step.
- How does the first touch with our platform happen? What’s the new and first-time user experience like?
- What are the main stages of a customer’s journey?
- What pre-visit and post-visit services do we offer to a patient?
Step 4: Use automation tools
Once you define touchpoints and arrange them on the map, it’s time to make use of technology and come up with ways to automate patient care. It might seem too easy to do, but in a complex healthcare system, something can always slip away.
Your goal is to make sure all processes are automated and run as smoothly as possible. For example, add online appointment booking to help patients schedule a consultation in seconds. Or enable prescription refill reminders to help users stay on top of things and show that you care about them.
- What digital engagement tools exist on the market? Which of them can benefit this particular healthcare journey?
- Will patients be satisfied with each step? How can you make their experience better?
Step 5: Create a communication plan
Clear communication and education can prevent misunderstandings and possible confusion among patients. Their journey should be well-informed and effective at each and every stage. This step can be executed towards the final launch or can be ongoing during the rest of the development services.
Before creating a communication plan, you need to analyze your current communication efforts and identify what works and what doesn’t. Researching the competitors and the market can also help you find new communication tools that can be implemented for a better patient experience. For example, you can improve your patient messaging system, spice up the tone of voice on the platform, or sign up for EHR calling to create a smart office.
- How effective is our current communication system?
- What are the most recent communication technologies and innovative tools we can adopt?
- Do healthcare providers know about the communication technologies we use/plan to use?
Step 6: Get patient feedback for future improvements
Last, but not least is to gather patient feedback from those who have already interacted with your solution and received healthcare services. If all previous steps can be done before the launch, this stage requires real users.
You will need to ask the patients how they really feel about the solution and compare it with your expectations or predictions. Feedback can be received by a short post-visit survey or quick thumb-up/thumb-down buttons on the screens. You can store this information separately or add it to the map so you can make precise data-driven decisions about patient journey mapping in the future.
- Was it easy to schedule an appointment with the app? What was patients’ overall experience with the platform like?
- How easy or difficult for patients was to interact with an app and complete their journey?
- What was missing from the patient’s interaction with the app?
Wrapping up
Overall, patient journey mapping is an effective tool to meet your user’s needs, create a personalized patient experience, improve patient satisfaction, and identify the room for improvement. When you start working on the map for your solution, preparation is the key to success. The better you know your customer, the more detailed and precise map you can create.
It’s very important to remember that you are not your own patient, and despite years of experience and expertise, you can still uncover surprising insights during the patient journey mapping.
Create insightful patient journey maps to better understand what your users experience and innovate your services accordingly.
Eventually, patient journey maps will lead to a higher patient retention rate, elevated quality of patient care, and improved user satisfaction.
At Purrweb, we provide mobile and web software development services with straightforward and cutting-edge UI/UX to level up the user experience. We help startups and existing companies build an MVP in 3 months and test a business idea with real-world customers.
What is patient journey mapping?
Patient journey mapping is a process of recreating steps patients would take in the healthcare app to reach their goals.
What is patient experience?
Patient experience encompasses all aspects of the patient's interaction with the startup, its services, and the product. To map the patient journey, you need to recreate every step patients would take in the app to reach their goal.
What are the benefits of patient journey mapping?
Creating a patient journey map can directly and significantly impact user experience on your platform. In particular, it can lead to personalized patient experience, identifying unmet user needs and common pain points, a common view of the patient experience among all team members, locating gaps between the intended experience for your patients versus the actual experience, breaking down and understanding complex journeys across multiple touchpoints.
Why is the patient journey map important in healthcare?
How patient journey maps are created.
Step 1: Define goals and the scope of the map. Step 2: Create patient personas and do user research. Step 3: Map the patient’s touchpoints. Step 4: Use automation tools. Step 5: Create a communication plan. Step 6: Get patient feedback for future improvements.
How to Develop a Fitness App: Features, Steps, Monetization
- Healthcare apps

Developing a Vet On-demand App in 2024
- Marketplace apps
Accounting Software Development: Types, Features, and Best Practices
Thanks for your inquiry. It usually take up to 24 hours to get back with reply.
Wanna schedule an online meeting?
Sorry, something went wrong with your request.
Please, try again later.
- FOLLOW US ON INSTAGRAM

The Patient Journey
What is the patient journey and how do you create a patient journey that will help you grow your practice .
Let’s discuss….
Introduction: What’s the Big Deal with the Patient Journey?
Ever wonder what goes through a patient’s mind from the moment they decide to seek help? It’s not just about booking an appointment and getting a prescription. The patient journey, especially in mental healthcare, is about navigating a maze filled with questions, doubts, and, hopefully, some answers. Why should we care? Because understanding this journey is the first step in transforming a daunting experience into a supportive voyage towards wellness.
Why does the patient journey matter? Why do patients expect so much more now?
Gone are the days when patients were passive recipients of care. Now, they’re informed, they’re vocal, and yes, they have options. With the internet at their fingertips, patients are not just looking for “any” therapist or counselor. They want someone who gets them, who can tailor the care to their unique stories. Are we ready to meet them where they are, or are we stuck in the “one-size-fits-all” mindset?
Stages of the Mental Healthcare Patient Journey: More Than Just a Waiting Room?
The mental healthcare journey is intricate. It’s personal. It starts with that first whisper of courage to seek help – but what comes next?

This is what it looks like from the client’s perspective:
Realization and Acknowledgment: What’s going on with me?
Ever had one of those days where you’re just off, and you can’t shake the feeling? It’s like your brain’s in a fog, but you’re not sure why. This stage is all about recognizing that what you’re feeling isn’t just a series of bad days; it’s something deeper.
Seeking Information: Where do I even begin to look for help?
You’ve realized something’s up, and now you’re on a quest for answers. You’re online, typing away, trying to figure out if what you’re feeling has a name. It’s a bit like detective work, but instead of looking for clues in a dark alley, you’re deep in web forums and mental health resources.
Evaluation of Options: Therapist or psychiatrist? Group therapy?
Now, this is where it gets real. You’re sifting through the sea of mental health professionals. Do you need someone to talk to, or is it more than that? Maybe a group setting is more your style? It’s all about finding the right fit for you.
Initiating Contact: Can I just text them, or do I have to call?
Picking up the phone or sending that first email to a mental health professional can feel like you’re about to cliff dive. It’s a big step, acknowledging you need help and reaching out.
Engagement in Care: What’s this therapy thing all about?
You’re in it now. Regular sessions, maybe some homework. It’s a bit like peeling an onion – lots of layers and a few tears, but it’s all part of the process.
Ongoing Management: How do I keep this up?
You’ve made progress, but how do you maintain it? This stage is all about the long game, finding strategies to manage your mental health day-to-day.
Each stage is a critical touchpoint. Understanding what your patient goes through at each stage means you can meet their actions with empathy and help them through the process.
Mapping the Mental Healthcare Patient Journey: Where Do We Even Start?
So, how do we map this journey? Is there a GPS for navigating mental health care? Not quite, but here’s how mental healthcare professionals can chart the course:
Understanding the patient’s world: What’s their story?
Dive deep. Understand the patient’s background, their struggles, and what they hope to achieve. This isn’t just about their symptoms; it’s about understanding the person behind them.
Identifying key touchpoints: When do they really need us?
Pinpoint those moments when a patient is most likely to seek help, make progress, or possibly disengage. These are critical opportunities for intervention and support.
Assessing Barriers to Care: What’s stopping them?
Stigma, access, cost? Identifying these barriers helps in tailoring the approach to care, making it as seamless and accessible as possible.
Tailoring Communication: How do they prefer to talk?
Some might like the directness of a phone call, while others might prefer the buffer of an email. It’s about meeting them where they’re comfortable.
Leveraging Digital Tools: Apps, portals, teletherapy, anyone?
Technology can be a game-changer in mental health care, offering new ways to connect, monitor progress, and provide support.
Feedback Loops: What’s working? What’s not?
Regular check-ins to gauge progress and patient satisfaction can help in adjusting the care plan as needed. It’s a partnership, after all.
Challenges and Real Solutions: Are We Doing Enough?
We face real challenges in mental healthcare. Stigma. Accessibility. Continuity of care. Are we addressing them, or just applying band-aids? Real solutions come from understanding the real problems. That means digging deep, asking uncomfortable questions, and being ready to overhaul systems that no longer serve our patients.

The patient journey in mental healthcare is more than a path from point A to B.
It’s a reflection of how we, as professionals, adapt to the evolving needs of our patients. Are we ready to embark on this journey with them? To not just lead but to listen, learn, and adapt? The future of mental healthcare depends on our willingness to embrace this journey, together.
Q&A: A Deep Dive Into the Patient Journey
What is a patient journey.
So, what’s this ‘patient journey’ everyone keeps talking about? It’s like the roadmap of a person’s experience in the healthcare system, from the first “Hmm, something’s not right” moment to the ongoing management of their health. But it’s not just a simple A to B trip. It’s more like a road trip with multiple stops, detours, and maybe even a flat tire or two along the way.
The patient journey encompasses every interaction and experience a patient has within the healthcare ecosystem. This includes online research, appointments, treatments, and follow-up care. It’s the full story of a patient’s path through care, including the emotional, physical, and psychological aspects. Why does it matter? Because understanding this journey helps healthcare providers offer more empathetic, efficient, and personalized care. It’s about seeing the person behind the patient chart.
What are the Stages of the Patient Journey?
Ever wonder what stages a patient goes through in their healthcare journey? It’s not just about showing up at the doctor’s office. The journey kicks off way before that, often at the first Google search for symptoms.
- Awareness: The “Something’s off” stage. It’s where the journey begins, with the patient noticing symptoms and starting to look for answers.
- Consideration: The “What are my options?” phase. Here, patients are digging deeper, researching conditions, and starting to look for potential healthcare providers.
- Decision: The “Let’s do this” moment. The patient chooses a provider and decides to seek treatment.
- Care: The “In the thick of it” stage. This includes all the appointments, treatments, and interactions with healthcare professionals.
- Post-Care: The “What now?” phase. After treatment, patients focus on recovery, follow-up care, and managing their health long-term.
Why is this important? Because understanding these stages helps healthcare providers anticipate needs and offer the right support at the right time.
How Do You Create a Patient Journey?
Wondering how to sketch out a patient journey? It’s part art, part science. You’re not just mapping a route; you’re stepping into your patients’ shoes, understanding their experiences, fears, and hopes.
- Research: Start by gathering data. Talk to patients, conduct surveys, and dive into their feedback. What’s working? What’s frustrating them?
- Persona Development: Create patient personas. These are composite sketches of your typical patients, capturing their backgrounds, needs, and healthcare goals.
- Mapping: With your research in hand, start mapping out the journey. Identify key touchpoints, decisions, and emotions at each stage.
- Analysis: Look for patterns and pain points. Where do patients feel lost or unsupported? Where are the moments of truth that can make or break their experience?
- Action Plan: Use your insights to improve. This might mean tweaking your communication strategy, offering more support at critical stages, or streamlining the appointment process.
Creating a patient journey map isn’t a one-and-done task. It’s an ongoing process of understanding, empathy, and improvement.
What is the Difference Between Patient Experience and Patient Journey?
So, patient experience and patient journey – same thing, right? Not quite. Think of the patient journey as the entire road trip, from the moment you start planning to when you return home. Patient experience, on the other hand, is how enjoyable the ride was. Was the car comfy? Was the scenery nice?
The patient journey is the broad overview of a patient’s entire healthcare process, covering every step and interaction along the way. It’s the map that outlines the path patients take through the healthcare system.
The patient experience dives deeper into the details of each interaction within that journey. It’s about how patients feel about the care they receive, the attitude of the healthcare staff, the ease of making appointments, and the quality of communication.
Why does the distinction matter? Because you can have a well-designed patient journey but still drop the ball on patient experience. Maybe the steps are all there, but if each step is fraught with frustration or indifference, the overall journey suffers. Understanding both is key to truly patient-centered care.
Helping businesses from the west to east coast, and everything in between!
Follow Us On Instagram!
Helpful page links.
Marketing for ABA
Marketing for Psychiatry
Google Ads
Social Media
LMR Digital Marketing
Digital Marketing Services for Healthcare & Other Service Based Companies. Reach out today to see if we are a good fit.
Who We Help
- Applied Behavior Analysis Companies
- Group Therapy Practices
- Rehab Centers
- Telehealth Companies
- EHR and other Saas Companies
- Speech Therapy Practices
- Medical Practices
- Psychiatric & Medication Management
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Donaldson L, Ricciardi W, Sheridan S, et al., editors. Textbook of Patient Safety and Clinical Risk Management [Internet]. Cham (CH): Springer; 2021. doi: 10.1007/978-3-030-59403-9_10

Textbook of Patient Safety and Clinical Risk Management [Internet].
Chapter 10 the patient journey.
Elena Beleffi , Paola Mosconi , and Susan Sheridan .
Affiliations
Published online: December 15, 2020.
The wide implementation of patient safety improvement efforts continues to face many barriers including insufficient involvement of all stakeholders in healthcare, lack of individual and organizational learning when medical errors occur and scarce investments in patient safety. The promotion of systems-based approaches offers methods and tools to improve the safety of care. A multidisciplinary perspective must include the involvement of patients and citizens as fundamental contributors to the design, implementation, and delivery of health services.
The patient journey is a challenging example of using a systems approach. The inclusion of the patient’s viewpoint and experience about their health journey throughout the time of care and across all the care settings represents a key factor in improving patient safety. Patient engagement ensures that the design of healthcare services are aligned with the values, the preferences, and needs of the patient community and integrates the real-life experience and the skills of the people to enhance patient safety in the patient journey.
The utmost priority to implement patient engagement is the training of patients. Therefore, training for both patients/families/advocates and health professionals is the foundation on which to build active engagement of patients and consequently an effective and efficient patient journey.
The chapter offers examples of successful training courses designed to foster strategic alliances among healthcare professionals and researchers with patients and their organizations. Training of patients constitutes the first step to develop shared knowledge, co-produced projects, and the achievement of active multilevel participation of patients for the implementation of patient safety in the patient journey.
10.1. Introduction
Almost 20 years after publication “To Err is Human: Building a Better Health System” (Kohn et al. 1999), patient safety is still not widely implemented. This report from the Institute of Medicine is the milestone that constituted a turning point for improving quality of care and patient safety identifying the need to rethink healthcare delivery to provide safe, effective, and efficient care.
The barriers of implementing patient safety as a driving force for change towards more effective healthcare include multiple factors: insufficient involvement of all stakeholders contributing to the care process, lack of willingness of organizations and individuals to learn from errors and scarce investments in patient safety improvement and research.
There is a growing need to promote systems approaches to finding solutions in healthcare to improve the safety of care, the quality of healthcare delivery, patients’ health and citizens’ well-being.
The discussion paper “Bringing a Systems Approach to Health” defines the systems approach as one “that applies scientific insights to understand the elements that influence health outcomes; models the relationships between those elements; and alters design, processes, or policies based on the resultant knowledge in order to produce better health at lower cost” [ 1 ].
A multidisciplinary approach must include the involvement of citizens and patients as fundamental contributors to the design, implementation, delivery, and evaluation of health services.
This means that citizen participation plays an essential role, bringing the unique point of view of patients and family members into the debate on patient safety and quality of care.
Patients and more generally citizens, when actively and systematically engaged, bring ideas and experiences which can support a collaborative and reciprocal learning process among the healthcare stakeholders. This produces knowledge that leads to improved practices, a real knowledge creation process where the dynamic participation of all actors in healthcare systems contribute to an active learning environment where the identification, the investigation, and the planning of solutions related to health incidents is a cyclic process enabling healthcare knowledge creation.
The added value of involving patients in healthcare is, respect to other more complex interventions, a low cost opportunity to take into consideration unconventional points of view creating and building knowledge and providing original insights and ideas that otherwise would not be considered.
Health professionals and patients’ skills and knowledge are acquired through individual experience or education and transferred to the health organizations in a perspective of co-production of healthcare. It is a merging of the efforts of those who produce and those who use the solutions to address health problems. It serves to establish a strengthened and long-term relationship in terms of trust and effectiveness and to distribute the responsibilities among all stakeholders [ 2 ].
In light of these arguments, the systems approach—inspired by the fundamentals of ergonomics and human factors (HFE)—creates new alliances between healthcare and engineering, of which patient journey is a challenging example [ 3 ].
Applying the systems approach to patient safety allows the analysis of the factors that characterize the encounters and the interactions between healthcare professionals and patients during the entire course of care. The observation of possible critical issues to the individual and specific encounter between clinician and patient is crucial in widening the scope of observation and research of the entire “journey” of the patient, taking into consideration the complexity of patient, their values and needs, their preferences, the economic and social context in which they live, and language and communication issues.
These observations and research should be carried out considering the interconnections and interactions together with the components of the processes; importance should be given to the context, and to manage the complexity, the value of a holistic approach.
10.2. The Patient Journey
A modern health system looks to the future in the context of the challenges imposed by the real world. It must manage the gap between guidelines and health protocols and what effectively happens and how reality is perceived by patients and family members.
It is more and more necessary to bring the patient’s point of view in the analysis of the care process, in the incident reporting and analysis, in the design and implementation of solutions and guidelines in healthcare.
Vincent and Amalberti in “Safer Healthcare” (2016) [ 4 ] stated that the incident analysis should broaden the class of events having consequences on patient safety. Incidents reported from the patient’s point of view should be included in addition to those suggested by health professionals. Additionally, when analyzing an incident, it should be done in the context of the patient journey rather than a single episode.
Instead of focusing on the individual encounter, it is necessary to extend the observation timeframe by applying the examination of contributing factors to each of the encounters that compose the patient journey (temporal series of encounters with healthcare facilities, a hospital unit, a specialist visit, a primary care clinic, a home health agency), considering both the negative and positive events and the points for improvement that were revealed (Fig. 10.1 ).
Analysis of safety along the patient journey
The adoption of this wider approach is unique in that it incorporates the patient’s perspective of safety and includes new features in the incident analysis such as asking patients to recount the episode of care, including patient and family in the investigation team when possible, asking patients the contributory factors from their point of observation and perception and involving patients and families in the reflections and comments on the disclosure process [ 4 ].
The episodes patients and families can highlight are often different from those that professionals are more accustomed to reporting. However, patients could be involved in further ways in incident reporting and assessment, and today patient-derived information constitutes a free and little used resource.
As per McCarthy’s definition, “patient journey mapping describes the patient experience, including tasks within encounters, the emotional journey, the physical journey, and the various touch points” [ 5 ]. Carayon and Woldridge define “patient journey as the spatio-temporal distribution of patients’ interactions with multiple care settings over time” [ 3 ], where at each point of touch with each healthcare service along the patient journey, the patient interacts with several system elements (task interaction, physical environment, interaction with tools and technologies, organization interaction, interaction with other organizations and other people, interaction with other people and teams within the organization) (Fig. 10.2 ).
The patient journey as a set of interactions and transitions
The patient journey represents the time sequence of what happens to the patient, especially during transitions of care, in particular considering that the health professional who takes care of the patient only sees the portion of care for which he is responsible and in which he has an active role. Conversely, the patient is the only person who has a continuously active and first-hand role during their health journey. They alone are in possession of information that characterizes the entire care experience.
Moreover, when patients navigate their journey, they contact and interface with multiple work systems at several time points, where the sequence of interactions in the work systems determine the outcome experienced by patients and families, healthcare professionals, and health organizations. (Fig. 10.3 ). Each local work system is influenced by a wider socio-organizational context, which can be formal healthcare organization (such as hospital, primary care facility, nursing home) or informal (home).
SEIPS 3.0 model: sociotechnical systems approach to patient journey and patient safety
Every point of the patient journey offers data on health outcomes and patient experience outcomes that should be used as feedback to redesign healthcare work systems in terms of adaptation, learning, improvement.
Patient’s experience represents an important resource in participatory collaborative design, especially in the patient journey where this experience is the result of multiple interactions across space and time.
10.3. Contextualizing Patient Safety in the Patient Journey
Many of the incidents or near-misses during healthcare are not due to serious errors, but to the combination of small failures, such as limited experience of a recently qualified doctor, use of obsolete equipment, an infection difficult to diagnose or inadequate communication within a team.
We know that the analysis of an incident requires looking back to the succession of events that have occurred and that led to the problematic episode, considering both active and latent errors, and all the aspects connected directly or indirectly. It is fundamental to examine the safety of the entire patient journey, all the encounters that make up the entire care process, to study the whole medical history of the patient in an attempt to reconstruct all the elements that characterize the “health journey”, not only from the viewpoint of the health professionals, but also from that of the patient and family.
In light of these arguments, new concepts, tools, models, and methods need to be embraced to support patient safety in the patient journey.
A significant contribution in terms of concepts, frameworks, and models is offered by Industrial and Systems Engineering, and often human factors and systems engineering (HF/SE) have an approach to include the preferences and the needs of stakeholders when designing solutions to address the critical aspects of a health process.
Human factors and ergonomics are described as “the scientific discipline concerned with the understanding of interactions among humans and other elements of a system, and the profession that applies theory, principles, data and methods to design in order to optimize human well-being and overall system performance. Practitioners of ergonomics and ergonomists contribute to the design and evaluation of tasks, jobs, products, environments and systems in order to make them compatible with the needs, abilities and limitations of people. Ergonomics helps harmonize things that interact with people in terms of people’s needs, abilities and limitations” [ 6 ].
Process models have found widespread use in drug management, visit planning, care transition, to name a few, and can offer tools and methods to investigate interprofessional and physician–patient communication, interruptions and health information handover.
Drawing from the finding of Carayon’s studies [ 3 ], the Systems Engineering Initiative for Patient Safety (SEIPS) model gives a description of five work system elements which when applied to a definite patient journey model should outline who (person) is doing what (tasks) with tool and technologies, taking into consideration the physical and organizational environment where all these activities take place. All these factors have to be examined for both patients and workers and the process analysis and modelling have to consider what patients and families/caregivers, healthcare professionals and workers actually do ( work-as-done versus work-as-imaginated ).
Patients, families, and caregivers are deeply involved in the healthcare process due to the tasks they carry out in the intermediate sectors of care between encounters. Away from direct interactions with professionals, they have to perform multiple actions requiring understanding of what behaviour to adopt, which instructions to follow, how to administer a medication and how to communicate with hospital doctors, general practitioner, and home healthcare professionals [ 3 ].
Taking into account what has been highlighted so far, one of the leading and most challenging keys to success in improving patient safety is to adopt a systems approach to patient safety which includes the patient’s perspective about their health journey throughout the time of care and across all the care settings.
This assumption highlights that patients and their families are valuable resources and can play an important role in patient safety improvement efforts. Viewing health systems as “co-producing systems”, patients can engage as partners in co-producing patient safety improvement activities individually, in groups and collectively. Individual patient and family member participation/co-production of safer care is fundamental. Equally as important is the co-management and co-governance of healthcare services, in addition to the engagement of communities in policy definition and designing activities.
In fact, patient engagement directs the design of healthcare systems towards the preferences, the values, the real-life experiences, and—not less important—the skills of the people to enhance patient safety in the patient journey.
Such a change of perspective involves multiple dimensions of interactions and relationship between patients and professionals, encompassing cooperation, dialogue and listening, trust, reciprocity and peer-to-peer work [ 2 ].
It follows that on the one hand the healthcare organizations have to demonstrate the willingness to support health professionals to effectively engage patients in the patient journey to achieve the common goal of reducing the risk of patient harm or incidents as well as the willingness to integrate patients and family members as partners into quality and safety improvement efforts. On the other hand, it is necessary to motivate and encourage patients and families/caregivers to actively participate during the individual care process for safer care as well as partner in organizational patient safety improvement efforts to ensure safer care for others.
The working group Patient and Family Involvement for the delivery of Safe and Quality Care [ 7 ] stated that the utmost priority to realize the patient involvement is the training of patients, followed by the promotion of interdisciplinary training programmes for healthcare professionals to promote patient and family engagement, the implementation of multilevel structures that allow for participatory processes by patients and smarter allocation of resources in healthcare that supports involving citizens in patient safety improvement efforts for better healthcare.
This working group was part of the activities of the “1st International Meeting about Patient safety for new generations—Florence, 31st August and 1st September 2018” organized by the Centre for Clinical Risk Management and Patient Safety, Tuscany Region—WHO Collaborating Centre for in Human Factors and Communication for the Delivery of Safe and Quality care [ 7 ].
Therefore, training for both patients/families/advocates and health professionals is a pillar on which to build active engagement of patients and consequently an effective and efficient patient journey. From this perspective, the participation of patients (i.e. representatives of patients’ associations and organizations, patient and citizen advocates) in training courses—specifically designed for this target audience of trainees and aimed to encourage co-production of care—is an essential and effective activity to co-produce a better healthcare system in terms of quality and safety of care.
Sharing a common language, promoting citizens’ and patients’ awareness of importance of co-production of care, teaching the key role that patients can play in making treatments safer (investments in health literacy), learning to work together and within a network (locally, regionally, and nationally/internationally) on priority safety and quality of care issues: these are some of the main strengths of training courses aimed to be at the basis of active engagement of patients and citizens.
Examples of successful training courses include “PartecipaSalute” and “Accademia del Cittadino” organized in Italy by Laboratory for Medical Research and Consumers Involvement of the Istituto di Ricerche Farmacologiche Mario Negri IRCCS and the Centre for Clinical Risk Management and Patient Safety, Tuscany Region. The following paragraph describes this educational experience which is specifically designed for citizens and patients to improve their knowledge and skills in patient safety and quality of care, with the aim of co-producing better healthcare services.
10.4. From PartecipaSalute to the Accademia del Cittadino: The Importance of Training Courses to Empower Patients
Over the last few years in the field of health and research and with regard to participation and involvement of citizens and patients, we have witnessed the transition from a paternalist to a partnership model. Individual citizens and those citizens involved in patients’ associations or groups have acquired a new role: no longer passive but actively involved in decision-making regarding health, healthcare, and research in the health field [ 8 , 9 ].
This is a progressive step-by-step process based on the recognition and implementation of the key concepts such as health literacy and empowerment. Health literacy, more properly used at individual level is defined as the capacity to obtain, read, understand, and use healthcare information in order to make appropriate health decisions and follow instructions for treatment [ 10 ]. Empowerment, more used at the community level, is a process that, starting from the acquisition of accurate knowledge and skills, enables groups to express their needs and more actively participate to request better assistance, care, and research. At this level, the availability of organized independent and evidence-based training courses is essential to allow people to be able to critically appraise and use information about the effects of healthcare interventions. Consequently, they will have the skills to participate in the multidisciplinary working groups (composed of researchers, health professionals, patient and citizen advocates, institutional representatives).
In the late 1990s, the Istituto di Ricerche Farmacologiche Mario Negri IRCCS held the first training courses of this kind focused at breast cancer associations. Some years later, within the project PartecipaSalute—a not-for-profit research project designed to foster a strategic alliance among healthcare professionals, patients, and their organizations—an ad hoc training programme for representatives of citizens’ and patients’ organizations was defined with a multimodule format [ 11 , 12 ]. This was an innovative approach, at least in the Italian setting in that period.
PartecipaSalute training programme has combined different experiences: the Mario Negri Institute IRCCS experience in collaborative research activities with patients’ associations, the Italian Cochrane Centre with the activities aimed at promoting the principles of evidence-based medicine, and Zadig long-term experience in health communication. The above promoters jointly developed the PartecipaSalute training programme on the belief that data are more important than opinions, and that every decision should be supported by well-conducted research data.
The spread of this belief to patients and citizens with the purpose of stronger involvement was a key point of PartecipaSalute training courses.
Therefore, patient, family, and community knowledge of the principles of how evidence is developed through clinical research is essential to make or support decisions in the health debate, to promote better clinical research, or to convey correct information. The strength of the PartecipaSalute programme was based on the exchange of experiences in an interactive way aimed at creating opportunities for discussion, overcoming the teacher–learner model. Each session started with an interactive discussion of a real situation—such as a screening, vaccination, therapy—and after sharing data, opinions or articles from media, evidence was presented and discussed, underlining significant methodological aspects. The programme offered the opportunity to debate the value and significance of the methodology offering critical appraisal tools. Each participant was invited to take an active part, starting from direct personal or associative experience. Table 10.1 presents the topics considered in the first three editions of the training programme. The participation was free, and different types of materials were provided including an ad hoc manual published by PartecipaSalute, copies of the PowerPoint presentation and articles.
Topics considered in PartecipaSalute [4] and PartecipaSalute-Accademia del Cittadino training courses
Considering the characteristics of the programme and its modular structure, the PartecipaSalute training programme could be adapted to specific contexts. In fact, the experience of PartecipaSalute was adopted at the regional level by Regione Toscana (Centre for Clinical Risk Management and Patient Safety and the Quality of healthcare and Clinical pathways of Health Department, Tuscany Region) developing a more specific training programme called PartecipaSalute-Accademia del Cittadino (Academy of Citizen), focused on patient safety and risk management. In particular, after some modules on methods related to evidence-based medicine, uncertainties in medicine and information and communication in health, the training was mainly dedicated to regional and local activities on clinical risk management, the role of patients’ associations to improve patient safety and to support the implementation of best practices, the analysis and data of adverse events and risk assessment in terms of quality and safety in the care processes (Table 10.2 ).
Topic integration in the PartecipaSalute-Accademia del Cittadino joint courses
The PartecipaSalute-Accademia del Cittadino joint training programme has been implemented in three editions over the last decade and has trained about 100 members of patient and citizen advocates representing 38 patients’ associations. The courses ranged from 5 to 3 modules of 2 days each in residential mode to allow participants to get to know each other and create a network of associations committed to be engaged in clinical research, quality, and healthcare safety issues.
The entire educational experience was characterized by the use of participatory training methods, based on working groups, practical exercises, lectures from experts with opportunities for discussions. As a result of this training course model, the participants were recognized as “expert patients” and were regularly involved in basic activities for promoting patient safety as auditors on significant events and helping to define policies on patient safety at the Tuscany regional level. In addition, they have participated in patient safety walkarounds in hospitals and in developing eight cartoons intended to promote the education of citizens for the prevention of the most diffused risks (such as prevention of infections, prevention of falls and handovers).
Feedback on the satisfaction on tutors, topics discussed and knowledge gained was regularly requested from participants through questionnaires distributed before and after the programme. In general, positive feedback was received; participants appreciated the interactive methods of work, the clarity of the language, and the effort to make difficult problems easy to understand. An ad hoc questionnaire was provided to the participants regarding the methodology of clinical research, always showing an improvement in the self-evaluated knowledge before and after the course. Feedback of the results of the evaluation was also shared with each participant. Most of participants reported their experience to other members of the organization. In particular, in the case of the Regione Toscana training, the possibility of immediately transferring what was learned in the course in all the activities in collaboration with the health institutions, policy makers, and health professionals—such as working groups on patient safety best practices, participation to audits, development of tools to improve health literacy—was appreciated.
Some limitations emerged from these experiences. The selection of participants is the first issue, not only because the training course is accessible to a small number of participants (in general no more than 30 participants), but also because the groups comprised of middle-aged and retired participants, with few younger ones. Additionally, there were few individual patient or family member representatives from patient associations. The majority of those representing patient associations were in managerial or leadership positions. Furthermore, it is difficult to choose between small, local, or bigger regional associations. Residential training courses also restricted the participation for geographical reasons.
The PartecipaSalute and ParteciaSalute-Accademia del Cittadino training experiences show that patients and citizens are willing to get actively involved in healthcare and the research debate. There is a real desire to improve their knowledge and skills on health and research issues and allow some general considerations regarding the active engagement of citizens representing associations and advocacy groups.
In conclusion, it is very important to invest in a process of empowerment aimed to have well-trained activists involved vigorously and constructively in the debate, design, and assessment of health and research. Switching from tokenism to active participation is necessary to effectively partner with patients and the general population to design, plan, and co-produce safer more effective healthcare, while also supporting better more patient-centred research [ 13 , 14 ].
Also, the training courses are feasible and useful, as has recently been discovered also by pharma or other groups that organize courses mainly focused on drugs and drug development, thus directing the participation of the groups more to market needs than to public health.
Furthermore, this training initiative facilitates the networking among associations in part overcoming the difficulties that derive from personalization and division among the associations representing citizens and patients.
Finally, this illustrates the importance of the design and promotion of training courses with institutions, such as the Regione Toscana, in order to be able to implement projects of real collaboration between institutions, healthcare professionals, and consumers’ and patients’ representatives.
10.5. Recommendations
A systemic approach to health can provide valuable models for wider implementation of patient safety. A multidisciplinary approach includes the involvement of citizens and patients as unique stakeholders in the design, implementation, delivery, and assessment of health services.
Involving patients in healthcare is an opportunity to bring uncommon points of view into policy making and to create shared knowledge between healthcare professionals and patients.
The implementation of patients’ and families’/caregivers’ perspectives in the patient journey is the golden opportunity to leverage crucial input, such as experiential knowledge, safer care, patient motivation, and trust and social cohesion into the co-production of safety solutions in healthcare. This represents a way to get closer to person-centred care, to create opportunities for patients to meet and share information and knowledge, to develop structures and policies for patient involvement at different levels (with healthcare systems, universities, and policy makers).
However, little has been done to overcome some healthcare systems barriers: the power imbalance between the doctor and patient, language differences, the lack of diffusion of non-technical skills and, last but not least, the lack of evidence about the value of patient involvement.
To be widely implemented, patient engagement in the patient journey requires courageous leadership, organizational efforts, a wider culture of safety of care, the implementation of multilevel structures for the engagement of patients and resources from smarter spending in healthcare.
Education is the landmark to integrate meaningful patient and citizen engagement in healthcare. Training of patients is the fundamental starting point to develop shared knowledge, co-produce projects, and implement an active multilevel participation of patients and families for the improvement of quality and safety of care.
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
- Cite this Page Beleffi E, Mosconi P, Sheridan S. The Patient Journey. 2020 Dec 15. In: Donaldson L, Ricciardi W, Sheridan S, et al., editors. Textbook of Patient Safety and Clinical Risk Management [Internet]. Cham (CH): Springer; 2021. Chapter 10. doi: 10.1007/978-3-030-59403-9_10
- PDF version of this page (884K)
In this Page
- Introduction
- The Patient Journey
- Contextualizing Patient Safety in the Patient Journey
- From PartecipaSalute to the Accademia del Cittadino: The Importance of Training Courses to Empower Patients
- Recommendations
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. [JBI Database System Rev Implem...] The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. Newell S, Jordan Z. JBI Database System Rev Implement Rep. 2015 Jan; 13(1):76-87.
- The future of Cochrane Neonatal. [Early Hum Dev. 2020] The future of Cochrane Neonatal. Soll RF, Ovelman C, McGuire W. Early Hum Dev. 2020 Nov; 150:105191. Epub 2020 Sep 12.
- A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. [JBI Libr Syst Rev. 2012] A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. Truglio-Londrigan M, Slyer JT, Singleton JK, Worral P. JBI Libr Syst Rev. 2012; 10(58):4633-4646.
- Review Health professionals' experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. [JBI Database System Rev Implem...] Review Health professionals' experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. Eddy K, Jordan Z, Stephenson M. JBI Database System Rev Implement Rep. 2016 Apr; 14(4):96-137.
- Review Evidence Brief: The Effectiveness Of Mandatory Computer-Based Trainings On Government Ethics, Workplace Harassment, Or Privacy And Information Security-Related Topics [ 2014] Review Evidence Brief: The Effectiveness Of Mandatory Computer-Based Trainings On Government Ethics, Workplace Harassment, Or Privacy And Information Security-Related Topics Peterson K, McCleery E. 2014 May
Recent Activity
- The Patient Journey - Textbook of Patient Safety and Clinical Risk Management The Patient Journey - Textbook of Patient Safety and Clinical Risk Management
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Definitive Healthcare (View)
- Monocl (ExpertInsight)
- Populi (Claims analytics)
- Carevoyance (Sales accelerator)
Patient Journey
What is a patient journey.
Patient journey is a term referring to a patient’s experience throughout an episode of care, beginning at admission and concluding with hospital discharge.
The renewed focus on patient experience in recent years stems from growing trends in healthcare consumerization and value-based care initiatives . To remain competitive, providers are beginning to consider patients more as customers and, consequently, are working to improve the overall healthcare experience and keep patients within their networks.
Why is the patient journey important in healthcare?
Patient journey mapping allows healthcare providers and other industry stakeholders to gain a better understanding of the patient experience and to find new ways to improve all points of the patient journey.
By understanding the patient journey, providers can build a hyper-targeted experience that addresses the unique needs of each patient and delivers more successful patient outcomes. Improved patient experiences can also save providers money — for example, by reducing the average time to diagnosis.
Share this Glossary Entry
Related links.
How Patient Journeys Influence Medical Device Strategy Consumerization 2.0: The Patient Joins the Care Team Top 8 Healthcare Trends in 2020
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Process mapping the...
Process mapping the patient journey: an introduction
- Related content
- Peer review
- Timothy M Trebble , consultant gastroenterologist 1 ,
- Navjyot Hansi , CMT 2 1 ,
- Theresa Hydes , CMT 1 1 ,
- Melissa A Smith , specialist registrar 2 ,
- Marc Baker , senior faculty member 3
- 1 Department of Gastroenterology, Portsmouth Hospitals Trust, Portsmouth PO6 3LY
- 2 Department of Gastroenterology, Guy’s and St Thomas’ NHS Foundation Trust, London
- 3 Lean Enterprise Academy, Ross-on-Wye, Hertfordshire
- Correspondence to: T M Trebble tim.trebble{at}porthosp.nhs.uk
- Accepted 15 July 2010
Process mapping enables the reconfiguring of the patient journey from the patient’s perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital.
Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the patient’s perspective to identify problems and suggest improvements. 1 2 We outline the steps involved in mapping the patient’s journey, as we believe that a basic understanding of this versatile and simple technique, and when and how to use it, is valuable to clinicians who are developing clinical services.
What information does process mapping provide and what is it used for?
Process mapping allows us to “see” and understand the patient’s experience 3 by separating the management of a specific condition or treatment into a series of consecutive events or steps (activities, interventions, or staff interactions, for example). The sequence of these steps between two points (from admission to the accident and emergency department to discharge from the ward) can be viewed as a patient pathway or process of care. 4
Improving the patient pathway involves the coordination of multidisciplinary practice, aiming to maximise clinical efficacy and efficiency by eliminating ineffective and unnecessary care. 5 The data provided by process mapping can be used to redesign the patient pathway 4 6 to improve the quality or efficiency of clinical management and to alter the focus of care towards activities most valued by the patient.
Process mapping has shown clinical benefit across a variety of specialties, multidisciplinary teams, and healthcare systems. 7 8 9 The NHS Institute for Innovation and Improvement proposes a range of practical benefits using this approach (box 1). 6
Box 1 Benefits of process mapping 6
A starting point for an improvement project specific for your own place of work
Creating a culture of ownership, responsibility and accountability for your team
Illustrates a patient pathway or process, understanding it from a patient’s perspective
An aid to plan changes more effectively
Collecting ideas, often from staff who understand the system but who rarely contribute to change
An interactive event that engages staff
An end product (a process map) that is easy to understand and highly visual
Several management systems are available to support process mapping and pathway redesign. 10 11 A common technique, derived originally from the Japanese car maker Toyota, is known as lean thinking transformation. 3 12 This considers each step in a patient pathway in terms of the relative contribution towards the patient’s outcome, taken from the patient’s perspective: it improves the patient’s health, wellbeing, and experience (value adding) or it does not (non-value or “waste”) (box 2). 14 15 16
Box 2 The eight types of waste in health care 13
Defects —Drug prescription errors; incomplete surgical equipment
Overproduction —Inappropriate scheduling
Transportation —Distance between related departments
Waiting —By patients or staff
Inventory —Excess stores, that expire
Motion —Poor ergonomics
Overprocessing —A sledgehammer to crack a nut
Human potential —Not making the most of staff skills
Process mapping can be used to identify and characterise value and non-value steps in the patient pathway (also known as value stream mapping). Using lean thinking transformation to redesign the pathway aims to enhance the contribution of value steps and remove non-value steps. 17 In most processes, non-value steps account for nine times more effort than steps that add value. 18
Reviewing the patient journey is always beneficial, and therefore a process mapping exercise can be undertaken at any time. However, common indications include a need to improve patients’ satisfaction or quality or financial aspects of a particular clinical service.
How to organise a process mapping exercise
Process mapping requires a planned approach, as even apparently straightforward patient journeys can be complex, with many interdependent steps. 4 A process mapping exercise should be an enjoyable and creative experience for staff. In common with other audit techniques, it must avoid being confrontational or judgmental or used to “name, shame, and blame.” 8 19
Preparation and planning
A good first step is to form a team of four or five key staff, ideally including a member with previous experience of lean thinking transformation. The group should decide on a plan for the project and its scope; this can be visualised by using a flow diagram (fig 1 ⇓ ). Producing a rough initial draft of the patient journey can be useful for providing an overview of the exercise.
Fig 1 Steps involved in a process mapping exercise
- Download figure
- Open in new tab
- Download powerpoint
The medical literature or questionnaire studies of patients’ expectations and outcomes should be reviewed to identify value adding steps involved in the management of the clinical condition or intervention from the patient’s perspective. 1 3
Data collection
Data collection should include information on each step under routine clinical circumstances in the usual clinical environment. Information is needed on waiting episodes and bottlenecks (any step within the patient pathway that slows the overall rate of a patient’s progress, normally through reduced capacity or availability 20 ). Using estimates of minimum and maximum time for each step reduces the influence of day to day variations that may skew the data. Limiting the number of steps (to below 60) aids subsequent analysis.
The techniques used for data collection (table 1 ⇓ ) each have advantages and disadvantages; a combination of approaches can be applied, contributing different qualitative or quantitative information. The commonly used technique of walking the patient journey includes interviews with patients and staff and direct observation of the patient journey and clinical environment. It allows the investigator to “see” the patient journey at first hand. Involving junior (or student) doctors or nurses as interviewers may increase the openness of opinions from staff, and time needed for data collection can be reduced by allotting members of the team to investigate different stages in the patient’s journey.
Data collection in process mapping
- View inline
Mapping the information
The process map should comprehensively represent the patient journey. It is common practice to draw the map by hand onto paper (often several metres long), either directly or on repositionable notes (fig 2 ⇓ ).
Fig 2 Section of a current state map of the endoscopy patient journey
Information relating to the steps or representing movement of information (request forms, results, etc) can be added. It is useful to obtain any missing information at this stage, either from staff within the meeting or by revisiting the clinical environment.
Analysing the data and problem solving
The map can be analysed by using a series of simple questions (box 3). The additional information can be added to the process map for visual representation. This can be helped by producing a workflow diagram—a map of the clinical environment, including information on patient, staff, and information movement (fig 3 ⇓ ). 18
Box 3 How to analyse a process map 6
How many steps are involved?
How many staff-staff interactions (handoffs)?
What is the time for each step and between each step?
What is the total time between start and finish (lead time)?
When does a patient join a queue, and is it a regular occurrence?
How many non-value steps are there?
What do patients complain about?
What are the problems for staff?
Fig 3 Workflow diagram of current state endoscopy pathway
Redesigning the patient journey
Lean thinking transformation involves redesigning the patient journey. 21 22 This will eliminate, combine and simplify non-value steps, 23 limit the impact of rate limiting steps (such as bottlenecks), and emphasise the value adding steps, making the process more patient-centred. 6 It is often useful to trial the new pathway and review its effect on patient management and satisfaction before attempting more sustained implementation.
Worked example: How to undertake a process mapping exercise
South Coast NHS Trust, a large district general hospital, plans to improve patient access to local services by offering unsedated endoscopy in two peripheral units. A consultant gastroenterologist has been asked to lead a process mapping exercise of the current patient journey to develop a fast track, high quality patient pathway.
In the absence of local data, he reviews the published literature and identifies key factors to the patient experience that include levels of discomfort during the procedure, time to discuss the findings with the endoscopist, and time spent waiting. 24 25 26 27 He recruits a team: an experienced performance manager, a sister from the endoscopy department, and two junior doctors.
The team drafts a map of the current endoscopy journey, using repositionable notes on the wall. This allows team members to identify the start (admission to the unit) and completion (discharge) points and the locations thought to be involved in the patient journey.
They decide to use a “walk the journey” format, interviewing staff in their clinical environments and allowing direct observation of the patient’s management.
The junior doctors visit the endoscopy unit over two days, building up rapport with the staff to ensure that they feel comfortable with being observed and interviewed (on a semistructured but informal basis). On each day they start at the point of admission at the reception office and follow the patient journey to completion.
They observe the process from staff and patient’s perspectives, sitting in on the booking process and the endoscopy procedure. They identify the sequence of steps and assess each for its duration (minimum and maximum times) and the factors that influence this. For some of the steps, they use a digital watch and notepad to check and record times. They also note staff-patient and staff-staff interactions and their function, and the recording and movement of relevant information.
Details for each step are entered into a simple table (table 2 ⇓ ), with relevant notes and symbols for bottlenecks and patients’ waits.
Patient journey for non-sedated upper gastrointestinal endoscopy
When data collection is complete, the doctor organises a meeting with the team. The individual steps of the patient journey are mapped on a single long section of paper with coloured temporary markers (fig 2 ⇑ ); additional information is added in different colours. A workflow diagram is drawn to show the physical route of the patient journey (fig 3 ⇑ ).
The performance manager calculates that the total patient journey takes a minimum of 50 minutes to a maximum of 345 minutes. This variation mainly reflects waiting times before a number of bottleneck steps.
Only five steps (14 to 17 and 22, table 2 ⇑ ) are considered both to add value and needed on the day of the procedure (providing patient information and consent can be obtained before the patient attends the department). These represent from 13 to 47 minutes. At its least efficient, therefore, only 4% of the patient journey (13 of 345 minutes) is spent in activities that contribute directly towards the patient’s outcome.
The team redesigns the patient journey (fig 4 ⇓ ) to increase time spent on value adding aspects but reduce waiting times, bottlenecks, and travelling distances. For example, time for discussing the results of the procedure is increased but the location is moved from the end of the journey (a bottleneck) to shortly after the procedure in the anteroom, reducing the patient’s waiting time and staff’s travelling distances.
Fig 4 Workflow diagram of future state endoscopy pathway
Implementing changes and sustaining improvements
The endoscopy staff are consulted on the new patient pathway, which is then piloted. After successful review two months later, including a patient satisfaction questionnaire, the new patient pathway is formally adopted in the peripheral units.
Further reading
Practical applications.
NHS Institute for Innovation and Improvement ( https://www.institute.nhs.uk )—comprehensive online resource providing practical guidance on process mapping and service improvement
Lean Enterprise Academy ( http://www.leanuk.org )—independent body dedicated to lean thinking in industry and healthcare, through training and academic discussion; its publication, Making Hospitals Work 23 is a practical guide to lean transformation in the hospital environment
Manufacturing Institute ( http://www.manufacturinginstitute.co.uk )—undertakes courses on process mapping and lean thinking transformation within health care and industrial practice
Theoretical basis
Bircheno J. The new lean toolbox . 4th ed. Buckingham: PICSIE Books, 2008
Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 [online publication 29 April]
Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998; 7 (suppl):S30-6
Graban M. Lean hospitals, improving quality, patient safety and employee satisfaction . New York: Taylor & Francis, 2009
Womack JP, Jones DT. Lean thinking . 2nd ed. London: Simon & Schuster, 2003
Cite this as: BMJ 2010;341:c4078
Contributors: TMT designed the protocol and drafted the manuscript; TMT, MB, JH, and TH collected and analysed the data; all authors critically reviewed and contributed towards revision and production of the manuscript. TMT is guarantor.
Competing interests: MB is a senior faculty member carrying out research for the Lean Enterprise Academy and undertakes paid consultancies both individually and from Lean Enterprise Academy, and training fees for providing lean thinking in healthcare.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ Kollberg B, Dahlgaard JJ, Brehmer P. Measuring lean initiatives in health care services: issues and findings. Int J Productivity Perform Manage 2007 ; 56 : 7 -24. OpenUrl CrossRef
- ↵ Bevan H, Lendon R. Improving performance by improving processes and systems. In: Walburg J, Bevan H, Wilderspin J, Lemmens K, eds. Performance management in health care. Abingdon: Routeledge, 2006:75-85.
- ↵ Kim CS, Spahlinger DA, Kin JM, Billi JE. Lean health care: what can hospitals learn from a world-class automaker? J Hosp Med 2006 ; 1 : 191 -9. OpenUrl CrossRef PubMed
- ↵ Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998 ; 7 (suppl): S30 -6. OpenUrl
- ↵ Peterson KM, Kane DP. Beyond disease management: population-based health management. Disease management. Chicago: American Hospital Publishing, 1996.
- ↵ NHS Modernisation Agency. Process mapping, analysis and redesign. London: Department of Health, 2005;1-40.
- ↵ Taylor AJ, Randall C. Process mapping: enhancing the implementation of the Liverpool care pathway. Int J Palliat Nurs 2007 ; 13 : 163 -7. OpenUrl PubMed
- ↵ Ben-Tovim DI, Dougherty ML, O’Connell TJ, McGrath KM. Patient journeys: the process of clinical redesign. Med J Aust 2008 ; 188 (suppl 6): S14 -7. OpenUrl PubMed Web of Science
- ↵ King DL, Ben-Tovim DI, Bassham J. Redesigning emergency department patient flows: application of lean thinking to health care. Emerg Med Australas 2006 ; 18 : 391 -7. OpenUrl CrossRef PubMed
- ↵ Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 ; published online 29 April.
- ↵ Rath F. Tools for developing a quality management program: proactive tools (process mapping, value stream mapping, fault tree analysis, and failure mode and effects analysis). Int J Radiat Oncol Biol Phys 2008 ; 71 (suppl): S187 -90. OpenUrl PubMed Web of Science
- ↵ Womack JP, Jones DT. Lean thinking. 2nd ed. London: Simon & Schuster, 2003.
- ↵ Graban M. Value and waste. In: Lean hospitals. New York: Taylor & Francis, 2009;35-56.
- ↵ Westwood N, James-Moore M, Cooke M. Going lean in the NHS. London: NHS Institute for Innovation and Improvement, 2007.
- ↵ Liker JK. The heart of the Toyota production system: eliminating waste. The Toyota way. New York: McGraw-Hill, 2004;27-34.
- ↵ Womack JP, Jones DT. Introduction: Lean thinking versus Muda. In: Lean thinking. 2nd ed. London: Simon & Schuster, 2003:15-28.
- ↵ George ML, Rowlands D, Price M, Maxey J. Value stream mapping and process flow tools. Lean six sigma pocket toolbook. New York: McGraw Hill, 2005:33-54.
- ↵ Fillingham D. Can lean save lives. Leadership Health Serv 2007 ; 20 : 231 -41. OpenUrl CrossRef
- ↵ Benjamin A. Audit: how to do it in practice. BMJ 2008 ; 336 : 1241 -5. OpenUrl FREE Full Text
- ↵ Vissers J. Unit Logistics. In: Vissers J, Beech R, eds. Health operations management patient flow logistics in health care. Oxford: Routledge, 2005:51-69.
- ↵ Graban M. Overview of lean for hospital. Lean hospitals. New York: Taylor & Francis, 2009;19-33.
- ↵ Eaton M. The key lean concepts. Lean for practitioners. Penryn, Cornwall: Academy Press, 2008:13-28.
- ↵ Baker M, Taylor I, Mitchell A. Analysing the situation: learning to think differently. In: Making hospitals work. Ross-on-Wye: Lean Enterprise Academy, 2009:51-70.
- ↵ Ko HH, Zhang H, Telford JJ, Enns R. Factors influencing patient satisfaction when undergoing endoscopic procedures. Gastrointest Endosc 2009 ; 69 : 883 -91. OpenUrl CrossRef PubMed Web of Science
- ↵ Del Rio AS, Baudet JS, Fernandez OA, Morales I, Socas MR. Evaluation of patient satisfaction in gastrointestinal endoscopy. Eur J Gastroenterol Hepatol 2007 ; 19 : 896 -900. OpenUrl CrossRef PubMed Web of Science
- ↵ Seip B, Huppertz-Hauss G, Sauar J, Bretthauer M, Hoff G. Patients’ satisfaction: an important factor in quality control of gastroscopies. Scand J Gastroenterol 2008 ; 43 : 1004 -11. OpenUrl CrossRef PubMed Web of Science
- ↵ Yanai H, Schushan-Eisen I, Neuman S, Novis B. Patient satisfaction with endoscopy measurement and assessment. Dig Dis 2008 ; 26 : 75 -9. OpenUrl CrossRef PubMed Web of Science
Root out friction in every digital experience, super-charge conversion rates, and optimise digital self-service
Uncover insights from any interaction, deliver AI-powered agent coaching, and reduce cost to serve
Increase revenue and loyalty with real-time insights and recommendations delivered straight to teams on the ground
Know how your people feel and empower managers to improve employee engagement, productivity, and retention
Take action in the moments that matter most along the employee journey and drive bottom line growth
Whatever they’re saying, wherever they’re saying it, know exactly what’s going on with your people
Get faster, richer insights with qual and quant tools that make powerful market research available to everyone
Run concept tests, pricing studies, prototyping + more with fast, powerful studies designed by UX research experts
Track your brand performance 24/7 and act quickly to respond to opportunities and challenges in your market
Meet the operating system for experience management
- Free Account
- Product Demos
- For Digital
- For Customer Care
- For Human Resources
- For Researchers
- Financial Services
- All Industries
Popular Use Cases
- Customer Experience
- Employee Experience
- Employee Exit Interviews
- Net Promoter Score
- Voice of Customer
- Customer Success Hub
- Product Documentation
- Training & Certification
- XM Institute
- Popular Resources
- Customer Stories
- Artificial Intelligence
- Market Research
- Partnerships
- Marketplace
The annual gathering of the experience leaders at the world’s iconic brands building breakthrough business results.
- English/AU & NZ
- Español/Europa
- Español/América Latina
- Português Brasileiro
- REQUEST DEMO
- Experience Management
- Industry Specific
- The Patient Journey
The patient journey: What it is and how it’s vital for success
10 min read In the digital age, the patient experience has become more complex but also more critical as it relates to patient retention, reimbursement, and patient satisfaction. In order to thrive in today’s healthcare landscape, it’s important to look at the patient journey when aiming to improve the patient experience.
Does your healthcare organisation ask patients for feedback following clinical encounters? This is a common approach used to improve the patient experience . You may gather key insights about a specific encounter, but you’ll miss out on an untapped system of important patient interactions throughout the care journey.
Improving patient experiences requires looking at the entire healthcare ecosystem. Patients communicate with their healthcare providers through a variety of channels, while interacting with a wide range of departments and individuals along the way.
To stand out in the market and provide an optimal experience for your patients, hospitals and health systems should look beyond clinical service delivery and begin patient journey mapping.
The patient journey is the entire sequence of events that begins when the patient first develops a need for clinical care and engages with your organisation. It follows the patient’s steps as they navigate your healthcare system, from initial scheduling to treatment to continuous care.
Learn how you can collect data and drive action along your patient journey
The patient journey vs. the patient experience
Why is the patient journey important? Each touchpoint of the patient engagement journey, from a simple visit to your website to checking in for an appointment, has downstream effects that can help or hinder meeting patient needs.
As the patient experience evolves, it’s important to expand how you are listening to your patients in order to close gaps and make continuous improvements.
In recent years, emphasis on the patient experience has become the focus of regulatory programs and payment incentives. Many quality measures today center around collecting patient feedback on the healthcare experience.
To satisfy these measures and drive quality improvement efforts, many organizations turn to post-transactional patient satisfaction surveys. The feedback from these surveys often measures only a limited set of touchpoints while overlooking other critical data from the full patient journey.
A holistic view
Patient experience programs often hone in on clinical service delivery, and many regulatory programs focus solely on numerical scores to measure improvement. These approaches may fail to identify pain points occurring in dozens of patient interactions within a healthcare system.
A holistic view of the patient journey is the key to modernising and strengthening your efforts to meet your patients’ needs. By breaking down silos into separate patient events, you can begin to identify blind spots where hidden challenges exist in your patient experiences.
By the time your patients engage with their care providers, they’ve likely interacted with your organisation a number of times. These interactions can occur digitally, over the phone, or in person. Navigating your website, verifying insurance coverage, and scheduling an appointment are all examples of pain points that may be creating barriers to care.
It’s easy to assume any given touchpoint is more or less important than another. The fact is that each one provides unique value to the patient’s experience. Each of them plays a role in helping the patient achieve their goals.
Patient engagement with your organisation doesn’t begin when the patient is examined by the healthcare provider, or even when they enter your medical facility. From initial awareness to ongoing care, the patient journey encompasses every separate interaction throughout the process of seeking, receiving, and continuing care within a health system.
There are several stages of the patient journey you should consider.
What triggers the patient’s need for care, and how does the patient learn about your organisation?
- Quality ratings and online reputation
- Campaign management
- Community involvement
Consideration
What drives a patient to choose your organisation over another?
- Coverage and benefits
- Healthcare provider search
What impacts your patient’s ability to receive care or support from your organisation?
- Patient portal
- Call centre
- Price transparency
Service delivery
What is your patient’s experience with their clinical care?
- Interaction with healthcare professionals
- Check-in and check-out
- Discharge process
Ongoing care
What type of patient engagement occurs after a visit?
- Wellness and care management
- Social determinants of health
- Population health
All of these examples influence the way in which your patients make decisions. It’s essential to understand which touchpoints along the patient’s journey are the most impactful or leave the largest gaps in care. There are patient expectations surrounding each type of interaction.
Patient journey mapping
How do you move beyond patient feedback on service delivery and focus instead on the end-to-end patient journey? Patient journey mapping can provide context around what your patients experience as they move through the various channels of your organisation.
A patient journey map is a visual representation of the steps the patient takes as they engage with your organisation in order to receive care. Patient journey maps should capture pre-visit and post-visit touchpoints in addition to those that occur when the patient is onsite at your medical facility.
Your patient journey may be broad and applicable to your entire patient base, or it may be specific to certain specialties, patient personas , demographics, or health events.
Start with an inventory of all the touchpoints for which you currently collect patient feedback. Next, determine what’s missing. Envision moving through your organisation from your patient’s point of view. Your patient journey map should include Interactions that take place pre-visit and post-visit, which are not always captured by traditional or regulatory surveys.
Benefits of patient journey mapping
There are many benefits to capturing key moments along the whole patient journey.
- A patient journey map allows you to walk in your patient’s shoes and think the way they think as they engage with your organisation. Patient journey mapping looks at patient experiences from the outside in.
- Mapping your patient journeys helps you to hone in on the areas where you may not be listening to your patients, but should be.
- You can uncover inconsistencies, gaps in care, and common pain points with patient journey mapping. These are difficult to identify when you collect feedback only on service delivery. Collecting data around these areas can aid in process optimisation and improve patient satisfaction.
- A patient journey map can give you a cross-functional view of your patient experience so you can engage all teams and stakeholders in gathering and understanding patient insights.
- Patient journey mapping provides context around behaviour and attitudes as patients move throughout the channels of your organisation. Are patients having to repeat paperwork? Do patients understand their follow-up care instructions? Are your patients able to easily navigate your patient portal? Patient journey mapping can help to answer these types of questions.
- Mapping the patient journey can transform your patient care approach from a reactive one to a proactive one.
Using patient journey data
Once you can visualise the end-to-end patient journey within your organisation, it’s time to listen to your patients and start gathering data.
Gather the right data
Collect data on all the touchpoints of the patient journey. Understand how your patients are interacting with every aspect of your organisation, including non-clinical interactions such as your website, scheduling, and billing. Involve multiple stakeholders during this process, including managers, doctors, nurses, other healthcare professionals, and administrative staff.
It’s important to capture all steps involved in each of these stages. For example, when looking for potential pain points surrounding the patient portal, consider how the patient sets up an account, logs in, navigates the interface, gets technical assistance, and so forth.
Also, consider patient expectations and usage–what are they using the portal to accomplish? Look for potential gaps in these experiences, such as paying a bill, contacting the provider with a question, reviewing test results, or scheduling an appointment.
Understanding the patient’s goals and actions along all the different paths of your patient journeys is essential to gathering the data you need to take action.
Understand the data
Gain insights using analytics , benchmarking, and visualisations to identify gaps and discover opportunities at each step of the patient’s journey. Trends along the various touchpoints can help you to discover pain points and identify opportunities.
It’s also important to engage all the right stakeholders when reviewing the data you collect. Involving the right teams and people is essential to understanding gaps and improving experiences.
Take action
Use the insights from all touchpoints along your patient journey to develop solutions to improve your patient experience.
A closed-loop system is ideal for taking action to close gaps along the patient journey. For example, if a patient gives a low score on a survey for your online scheduling tool, you could follow up with the patient to ensure they were able to schedule an appointment.
Using the data you collect to drive specific actions and feed into processes is vital to creating a seamless patient journey.
Why Qualtrics?
At Qualtrics, we want to enable you to listen to and understand your patients across all aspects of their journey, all within a single platform. Omnichannel distribution lets you gather feedback from patients from where they are at during each touchpoint, with powerful built-in analytics for uncovering meaningful insights.
The Qualtrics XM Platform™ provides a single source for all of your patient journey data. Real-time feedback displayed in role- and location-based dashboards helps deliver pertinent information to the right people, allowing you to take prompt action where needed.
Start collecting data and driving action along your patient journey
Related resources
Patient experience: your complete guide 12 min read, symptoms survey 10 min read, quality improvement in healthcare 11 min read, nurse satisfaction survey 11 min read, cahps surveys 6 min read, patient journey mapping 15 min read, nursing shortages 13 min read, request demo.
Ready to learn more about Qualtrics?

- Adelaide Crows Adelaide Crows
- Brisbane Brisbane
- Carlton Carlton
- Collingwood Collingwood
- Essendon Essendon
- Fremantle Fremantle
- Geelong Geelong
- Gold Coast Suns Gold Coast Suns
- GWS Giants GWS Giants
- Hawthorn Hawthorn
- Melbourne Melbourne
- North Melbourne North Melbourne
- Port Adelaide Port Adelaide
- Richmond Richmond
- St Kilda St Kilda
- Sydney Swans Sydney Swans
- West Coast Eagles West Coast Eagles
- Western Bulldogs Western Bulldogs
More from Telstra
Australia's best network.

- Match Centre

- Team Lineups
- Broadcast Guide
- Injury List
- Match Videos
- National Champs
- Club Finder
- Buy Tickets
- Play Fantasy
- Fantasy Hub
- National Championships
- Rising Star
- Competitions & Promotions
- AFL Policies
- Annual Reports
- AFL On Demand
Follow AFLW on Social
'Clear evidence': Injury-hit Pies staying patient amid 0-4 start
Sarah Black speaks to Collingwood's head of women's football Jess Burger after the Pies' tough start to the season

A NEW coach and a fresh gameplan, followed by an injury crisis and four straight losses to open the season.
Just over a third of the way through the season, where does Collingwood go from here?
And what can we expect from the Magpies for the rest of the year under Sam Wright?
It's not yet the Pies' worst start to a year, after 2019 saw them sit at 0-6 before nabbing one win in the last round of the year, in Wayne Siekman's last season in charge.
"We're all in this industry because we're competitive and we want to get wins on the board. But what it has looked like is very process driven," head of women's football Jess Burger told AFL.com.au .
"As cliched as that sounds like, we are very clear on what the type of environment we're trying to create, very clear on what game system we're trying to paint the picture of each week.

W Show: Panic stations at the Pies, Daisy shows us how it’s done
Ben Brown joins The W Show this week to dissect why it’s time for the Magpies to panic, what’s going on at the Dees, and why Daisy Pearce is showing the rest of the comp how it’s done
"We're not satisfied with playing really solid first halves against quality outfits and actually being really competitive and then falling away. But what that has given us, is really clear evidence on what it does look like to play our system, and then what it doesn't look like when we don't execute.
"To play a certain system, you need continuity, and we've seen the best sides for a long time. There's no secret as to why Brisbane and Melbourne and those sorts of teams have been up the top for so long. It's because they've had that shared experience, that continuity in game style, coaches and those sorts of things."
The medical department at Collingwood has been working overtime, with an average of seven players unavailable each week, for a squad of only 30 players.
The Magpies will be without their entire first-choice midfield of Bri Davey (concussion), Brit Bonnici (calf) and Mikala Cann (suspension) for their vital clash against fellow winless side the Western Bulldogs on Sunday .

Massive Magpies blow with skipper ruled out
Collingwood suffers a big injury concern with captain Bri Davey forced out of the contest after copping some heavy contact to the back of the head
Cann was cited for a dangerous tackle on Bella Lewis, and accepted a one-match suspension rather than challenging it at the Tribunal, despite the team's lengthy unavailable list and the West Coast midfielder playing out the match.
"When you look at how it was graded, there was very little room to be able to challenge what that looks like," Burger said.
"It's careless. Her head does make contact with the ground as a result of the tackle, so there is high contact received, and the League has been very clear around any sort of dangerous tackle will be graded as medium impact.
"That doesn't leave us with much wriggle room to try and challenge around that. Mikala knows she's got a duty of care, she's a physical player, and I would say nine times out of 10, she's executing her tackles really well. We'll continue to educate and train on what it looks like to tackle hard but fair."
Kalinda Howarth was recruited with the knowledge she still had quite some way to go in her ACL recovery, but the Pies had hoped ex-Docker Mikayla Hyde would have been right to go in round one, despite a foot issue.

Instead, the lively small forward suffered a setback with irritation in the affected area, and is still building her running loads after missing most of pre-season.
The two long-term injuries immediately cut the list from 30 to 28, while integral forward Nell Morris-Dalton (back) and classy runner Aishling Sheridan (personal) had already been ruled inactive and replaced in the primary squad during pre-season.
The attack was always going to be skinny this year – the Pies having struggled to find a quality forward since the departure of Chloe Molloy – but Morris-Dalton was set to play a key role as leader of the forward line.
Collingwood has kicked a total of 13.22 in its first four matches this year.
Imogen Barnett – who missed nearly the entire 2023 season with a broken ankle – is carrying a heavy load as the near-sole tall target, and her absence is noted when she rotates into the ruck to give Sabrina Frederick a chop-out.

Barnett breaks drought with first AFLW goal
After seven career behinds, Imogen Barnett finally earns a well-deserved major in the big league following a quality mark and set shot
Top-up player Jordi Ivey plays for Collingwood's VFLW side, and is technically a train-on player with Geelong, training with the Cats over pre-season, but AFLW list management rules allow her to be temporarily elevated by another side to broaden the replacement pool across the League.
Ivey has been a preferred selection in attack over Erica Fowler and draftee Georgia Clark , but at 175cm, is not the tallest forward going around.
Fellow top-up player and Pies VFLW midfielder Sarah Ingram will play against the Bulldogs.
"It was a pretty easy phone call for us to make, to say, 'Hey, can you get yourself back up the highway?'" Burger said.
"Her (Ivey's) experience, her level head, her knowledge, and she's been completely unfazed to come in and play a really difficult role.

"For someone to come in off limited education – in terms of within our system – but she certainly hasn't had limited preparation, she's played a lot of footy this year. She's been able to do it seamlessly, and it's a credit to her and what she's been able to do to get herself right.
"She's obviously had a bad run with injury (foot issues), but I think the experience that she's had playing at multiple clubs has held her in really good stead, because she's been able to come in and get the job done, no matter what we've asked of her."
Most expected Collingwood to bounce back from last year's 11th-place finish, given the four straight finals appearances that had preceded it.
But it's become clear we've had to re-adjust our expectations as to what the Magpies will look like for the rest of the season because of squad unavailability, teething issues around adopting the new gameplan, and the simple fact of improvement from the rest of the competition.
It's no surprise Wright came from the powerful North Melbourne, given his continual discussion at press conferences of "the system", a common refrain at the Roos. But limited numbers on the track means it's harder to get everyone on the same page at the same time, and training bodies and minds to act instinctively to a new system, while under pressure, doesn't happen overnight.

It's just going to take time.
"Absolutely, the injuries do take their toll, but what we've seen is when the players have come back, they've actually made an impact straight away," Burger said.
"We desperately want to have our best outfit out there, but I guess the silver lining is now it's really clear that almost every player on our list (bar Clark) has been exposed to our system in terms of what it does and doesn't look like, and the role they can play within that.
"It also gives us a really good look about how we're going to continue to move forward, and who's able to contribute to the roles we need for that, too.
"The exciting thing is, we're going to have more reinforcements over the coming weeks, and touch wood, we continue to build on the roles that the players are playing at the moment, to be able to demonstrate that execution of that system.
"What that then hopefully translates to is some results and some excitement around it, because we do genuinely think that the brand that we're going to be executing will take the game forward. We want to be playing a quick, up-tempo style that allows us to score. We certainly want to reinforce that with a really consistent defensive system."

Tagged is back! New co-host, same show
Sarah Hosking is joined by NEW co-host Sarah Rowe for another laugh-packed season of Tagged

Terrific Tigers power past Port for fourth straight win
The Tigers have continued their good form with a strong win over the Power

The verdict is in: Docker learns fate at Tribunal
Gabby O'Sullivan challenged her one-match suspension at the AFLW Tribunal

AFLW injury list, W5: Another blow for Dees, star Cat could return
Who's still sore? Who's nearing a return? Check out your club's injury updates ahead of AFLW week five

Dockers run down Demons in a comeback special
For the second week in a row Fremantle has come from behind, this time running down a four-goal deficit to beat Melbourne
Latest Videos

AFLW full post-match, WK5: Power
Watch Port Adelaide's press conference after week five’s match against Richmond

AFLW full post-match, WK5: Tigers
Watch Richmond's press conference after week five’s match against Port Adelaide

AFLW Mini-Match: Richmond v Port Adelaide
Extended highlights of the Tigers and Power clash in week five of the 2024 NAB AFLW Season

AFLW Highlights: Richmond v Port Adelaide
The Tigers and Power clash in round five of the 2024 NAB AFLW Season
Latest News

AFLW TEAMS: Roos rest star duo, recruit to make Blues debut
The teams are in for Wednesday's AFLW match between Carlton and North Melbourne
Premier Partner

Major Partners

Download the Official AFL App
- Download on the app store
- © 2024 AFL
- Terms of Use
- Privacy Policy
- AFLW Women's Football Vision
- Diversity & Inclusion
- Mental Health & Wellbeing
- Get Involved
- Schools.AFL
- AFL Membership
Acknowledgement of Country
In the spirit of reconciliation the AFL acknowledges the Traditional Custodians of country throughout Australia and their connections to land, sea and community. We pay our respect to their Elders past and present and extend that respect to all Aboriginal and Torres Strait Islander peoples today.
- Share on Facebook
- Share on Twitter
- Share on WhatsApp
- Copy link Copied to clipboard!

IMAGES
VIDEO
COMMENTS
Your patient engagement journey is what guides your patients to making the best possible decisions on their care so they get better. The easier you make it for them to engage with you, the higher quality their care will be. Ultimately, you want your patients to be evangelists for your services based on their positive experiences.
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end. A patient's journey begins before they even walk through the doors of a doctor's office or hospital. It may start when they research ...
The patient journey map employs visual representation to gain deeper insights into how patients engage with a healthcare facility throughout their care journey. This unique approach is an evolution of the customer journey map, tailored specifically to the healthcare context. By employing this method, healthcare providers can unravel the ...
What is the patient journey? The patient journey is the sequence of events that begins when a patient first develops a need for care. Rather than focusing on service delivery, the patient journey encompasses all touchpoints of a patient's healthcare experience-from locating healthcare providers and scheduling appointments, to paying the bill and continuing their care after treatment.
Patient journey maps provide a deeper understanding of the patient's experience. This helps identify key touchpoints along the journey where improvements can be made. Patient journey maps reveal critical moments in the patient's experience, allowing organizations to address gaps and enhance service delivery.
Patient journey mapping works to identify and understand the details of all patient touchpoints within a specific healthcare experience. It helps you visualize the process patients go through to receive care, complete a treatment plan, and/or reach a desired outcome. When done correctly, patient journey maps make it easier for you to identify ...
Patient journey mapping is a pivotal strategic process for capturing and communicating patient interactions. This practice, when executed effectively, establishes a foundation for seamless patient experiences, fosters empowerment for both patients and physicians, and yields valuable insights for informed decisions. ...
The patient journey is the entire sequence of events that begins when the patient first develops a need for clinical care and engages with your organization. It follows the patient's steps as they navigate your healthcare system, from initial scheduling to treatment to continuous care.
Patient Journey Mapping is a strategic tool in healthcare that visually illustrates the entire patient experience, from initial contact to post-treatment follow-up. It involves mapping out key touchpoints and stages, such as appointment scheduling, diagnosis, treatment, and aftercare.
Mapping a patient journey offers a range of benefits that contribute to improving the overall quality of healthcare delivery. Here are some key advantages: Visualization of the entire patient journey helps healthcare providers identify critical patient journey touchpoints that impact patient satisfaction and experience and require immediate attention. . By paying more attention to these ...
Put simply, a patient journey defines the entire experience a patient goes through during their medical treatment at your healthcare facility. As such, the patient journey covers the whole medical process (virtual and in-person), from developing symptoms and scheduling a doctor's appointment to completing the medical treatment and beyond. ...
Patient journey mapping, also called healthcare process mapping, is the exercise healthcare leaders use to understand better how patients interact with a healthcare system or practice throughout their journey. The patient journey map helps the stakeholders to analyze the patient experience from various perspectives. With proper journey mapping ...
Therefore, hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey [12 - 14]. Many tools may be used to measure and understand patient experience [15, 16]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and safety ...
Patient journey mapping is a useful strategy to employ during the build-out of any healthcare engagement campaign. As mentioned, the patient journey happens in six distinct stages: It begins with awareness - the moment the patient develops symptoms or becomes motivated to pursue medical treatment - and, in an ideal scenario, never entirely ...
Patient journey mapping — also called user journey mapping in healthcare — is an exercise for medical startup owners and developers to create a visual trip of the patient across the solution and come up with a seamless patient journey. The key idea is to construct a patient experience that encompasses all aspects of the patient's ...
The patient journey is the broad overview of a patient's entire healthcare process, covering every step and interaction along the way. It's the map that outlines the path patients take through the healthcare system. The patient experience dives deeper into the details of each interaction within that journey.
The patient journey is a challenging example of using a systems approach. The inclusion of the patient's viewpoint and experience about their health journey throughout the time of care and across all the care settings represents a key factor in improving patient safety. Patient engagement ensures that the design of healthcare services are ...
Join Ed Marx and Cris Ross, authors of Diagnosed: An Insider's Guide for Your Healthcare Journey, in supporting the nonprofit mission of Mayo Clinic Comprehensive Cancer Center. With your support, Mayo Clinic is able to provide unparalleled expertise in patient care and innovative research to meet the needs of our patients.
Patient journey is a term referring to a patient's experience throughout an episode of care, beginning at admission and concluding with hospital discharge.. The renewed focus on patient experience in recent years stems from growing trends in healthcare consumerization and value-based care initiatives.To remain competitive, providers are beginning to consider patients more as customers and ...
Patient journey map. A patient journey map is a visual tool that illustrates the relationship a patient has with a healthcare organization over time. It outlines all of the patient touch points during each stage of interaction and aids in the creation of strategic outreach that improves both patient engagement and satisfaction. When done ...
Patient journey mapping is a research approach undertaken to help better understand the touchpoints and pain points of the patient experience with a healthcare provider. More specifically, you will find that patient journey mapping is concerned with the patient experience at three different stages - The pre-visit, visit, and post visit.
Process mapping enables the reconfiguring of the patient journey from the patient's perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital. Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the ...
The patient journey is the entire sequence of events that begins when the patient first develops a need for clinical care and engages with your organisation. It follows the patient's steps as they navigate your healthcare system, from initial scheduling to treatment to continuous care. Learn how you can collect data and drive action along ...
Patient journey definition "OK, but how does that apply to healthcare and more specifically to patient journey maps?" you may ask. When we talk about patient journey mapping, what's implied is a visual representation of all patient interactions with a healthcare system.. It's not some abstract notion or a newly minted buzzword thrown around at healthcare conferences.
The Migraine Patient Journey: Case Challenges on Best Practices in Identification and Treatment. When is migraine becoming chronic migraine, and how do we manage it? Authors: Stephanie J. Nahas, MD, MSEd, FAHS, FAAN. Login to Start Continue Activity ((((( ® . Supported by an independent educational grant from AbbVie. ...
'Clear evidence': Injury-hit Pies staying patient amid 0-4 start. Sarah Black speaks to Collingwood's head of women's football Jess Burger after the Pies' tough start to the season By Sarah Black. 22 hrs ago Collingwood players leave the field after a loss to Hawthorn in round two, 2024. Picture: AFL Photos