Stephen King Wiki
Hello Stephen King fan ! We at the Stephen King Wiki are incredibly happy you've decided to visit, please feel free to check out our Discusions and/or start editing articles. If you're visiting anonymously you'll need to make an account . Before you start editing or posting, you'll want to read our simple ruleset , just so you don't accidentally break any rules. If you see anyone breaking any of these rules, please report it to the message wall of an Administrator .

Captain Trips
- View history
Captain Trips is a nickname for the constantly-shifting antigen virus that exterminates 99.4% of the human population in The Stand . The meaning of the nickname is never revealed.
- 1 Background
- 2 Description & Symptoms
- 3 Susceptibility
- 6 Aftermath
- 7 Appearances
Background [ ]
Developed under the codename Project Blue by a biological weapon's laboratory located beneath California's Mojave Desert, it is also known as Blue virus ( Blue Virus ), 848-AB , A-prime , A6 , the rales , superflu , choking sickness , and tube neck .
The virus is set loose on the population when Charlie Campion , who was working in the base that developed it, noticed that the virus had been released throughout the facility and managed to escape with his wife and daughter, but not before being infected with it himself. He carried the virus all the way to Arnette, Texas , before dying, thus setting in motion the events of the novel.
Description & Symptoms [ ]
Captain Trips is an extremely deadly virus, able to be transmitted as easily as the common flu it is based on, with far more lethal results. It has a communicability rate of 99.4%, meaning that all but a tiny number of humans can catch it. The virus starts out like a common cold, causing weariness, nasal congestion and sneezing, and most people who catch it think that a common cold is all they have.
The superflu virus is highly adaptable, shifting and changing constantly, making medicines useless against it. At best, medicine only briefly holds off the inevitable. No vaccine was ever developed for it, before or after its escape from the lab where it was created, as its constantly-changing nature made a vaccine impossible to create. The fact that it was designed as a biological weapon is another reason for the lack of a cure; it was supposed to be unstoppable, as anything less would have limited its ability to kill swiftly and efficiently.
As it progresses, Captain Trips causes increasingly-worse fever, headaches, crippling physical pain, swelling, and delirium. Victims slip in and out of consciousness, and begin thinking they are in other places, other times in their lives. Sometimes, when nearing death, victims will actually calm down and return to clear, level-headed thinking for a short time. In all cases, however, once someone has caught Captain Trips, the chances of death are 100% certain - it's just a question of how long it will take for the virus and it's complications to wear out their body's natural defenses.
Susceptibility [ ]
- Domestic guinea pigs ( Cavia porcellus )
Immunity [ ]
It is unknown how a given human or animal can be immune to the superflu, but based on the United States Military's own knowledge of the virus (from data on it in the files of Project Blue), 0.6% of the human race was immune to it. Most likely, immunity is genetic, and would be that way for the animals capable of catching the virus as well.
Colonel Richard Deitz, operating in Atlanta, then in Vermont after the Plague Center in Atlanta was compromised, led the effort to find a cure for the virus. Due to the fact that "Captain Trips" shifts at an extremely rapid pace, not one attempted vaccine worked. Men and women with a lifetime of experience in medicine were mystified at Stuart Redman's survival, especially after they injected him with the superflu under the guise of administering a sedative. Redman's immune system swiftly isolated and killed the virus, but with no visible sign of how.
Human civilization collapsed entirely within one month of the outbreak, and no cure or means of giving others immunity to the superflu was ever developed.
Outbreak [ ]
The superflu was a biological weapon created by the American government, which got loose during a containment breach on June 13, 1990. Everyone died in the base, except for a security guard named Charlie Campion, who fled the base with his wife and child, unaware that he was infected himself.
Campion was able to survive long enough to drive to a gas station in Arnette, Texas on June 16, before succumbing to the virus. The virus spread to the residents of Arnette, and on June 18, started an explosive spread across America and then the world, like a chain letter from Hell. It had a 99.4% communicability rate and a 99% mortality rate. The US government forced news services to print and broadcast the official line, which was that there was nothing wrong going on, it was just the normal flu, and the situation was being under control.
Hospitals were soon over-filled to capacity and entire towns were quarantined as soldiers were deployed on the roads and highways, blocking off the entrances and exits. It wasn't long before evidence to the contrary began to spread: photos, videos, and eyewitness accounts revealed to the world the truth. Film footage of soldiers coldly dumping bodies into harbors from trucks and barge-trains full of plague victims that were towed out to the sea to be dumped was seen by protestors and shown on the news. US military operations were soon directed toward news networks that broadcast the footage, many of them being shut down by violent means.
Posters went up on college and university campuses throughout the country. Flyers that were variations on the theme of government complicity and cover-up with the superflu, which spread panic. Rebellious journalists, news staff, and talk radio broadcasters began to print and broadcast the truth, alerting the public to the lethal pandemic and the government coverup. To suppress the news, soldiers massacred protesting college students, executed news employees, and blew up the buildings of news broadcasters.
Full blown riots broke out in most parts of the country (and the world), as people took advantage of the situation to loot for supplies. Eventually, these looters and rioters caught the superflu, and either locked themselves in other peoples’ houses, or died trying to leave the city in clogged highways. Most of the population died either bedridden in their own homes, or stuck in traffic until they succumbed to the plague. The president, himself infected with the superflu, gave one last speech to a dying country, one last time denying its lethality and that the virus was created by the government.
Eventually, the superflu burned out, and by July 4, 1990, 99.4% of the human population had died. Bodies laid either in their own homes, in their cars, or even on the streets.
Aftermath [ ]
Captain Trips, a man-made virus created by the United States Military on taxpayer dollars, killed all but a handful of the humans, dogs, guinea pigs, horses and monkeys on Earth by July 4 of 1980/1985/1990/1994/2020 (depending on the exact version or adaptation of the story). Riots, suicides, accidents, injuries (many of which were made fatal by a total absence of functioning hospitals and available living medical personnel), and murders cut down the number of survivors even further.
The animal species able to catch Captain Trips are implied to be doomed, left without a sustainable population, and humans have an uncertain future at best. While Frannie Goldsmith's baby, Peter, was able to fight off the superflu, another woman in Boulder had previously given birth to twins, and both of them had caught the superflu and died.
Millions of dead bodies were left in the wake of Captain Trips, most killed by the virus, others from different causes. In the few areas where survivors congregated, like Las Vegas, Nevada and Boulder, Colorado in the former United States, the decaying remains were collected and buried in mass graves. Everywhere else, the bodies were left in the hospitals, houses, cars, and on the streets where they had died. With the human population virtually wiped out, nearly all of the old world's settlements, vehicles, structures and buildings were abandoned, left to be reclaimed by the elements.
Appearances [ ]
- The Stand: The Complete & Uncut Edition
- Wizard and Glass
- The Stand: Captain Trips
- The Stand: American Nightmares
- The Stand: Soul Survivors
- The Stand (miniseries)
- The Stand (2020 Miniseries)
Gallery [ ]

- Stephen King
- 2 Beverly Marsh
- 3 Eddie Kaspbrak
Screen Rant
The stand: where the superflu nickname "captain trips" comes from.
Stephen King's The Stand features a deadly virus that spreads across the United States that is often called "Captain Trips," but what does it mean?
Stephen King's The Stand features a deadly virus that sweeps across the United States, killing over 99% of the population. In the book, the virus is most often called the superflu, but it goes by several other names as well, including an odd one, Captain Trips. Here's where this curious nickname likely stems from.
The Superflu in The Stand goes by many names. The scientists working in the weapons lab where the virus originated call it by its military codename, " Project Blue ." However, it's also called " A-Prime ," " A6 ," and " 848-AB " at various points in the novel. Outside of the military and scientific community in the thick of the superflu pandemic , it goes by different names that are far more descriptive. It's called "choking sickness," "the rales," "tube neck," and, of course, the "superflu." Given the fact that the virus is a respiratory illness, many of these colloquial terms are rather fitting and self-explanatory.
Related: The Stand: How The Superflu Started In Each Version (Miniseries & Book)
However, the name "Captain Trips" is a bit harder to describe. Stephen King has never officially explained why the Superflu is called Captain Trips, other than it's a term young people came up with to identify the virus. Given that and nothing else, the term Captain Trips likely refers to the symptoms of the virus in that it causes delirium, some rather hungover-like headaches, and hallucinations similar to those experienced by people on LSD. On the other hand, the term goes deeper than that and may even refer to legendary rocker Jerry Garcia from the Grateful Dead.
Other Theories About The Stand's Term "Captain Trips"
In addition to the term "Captain Trips" never being explained in Stephen King's book , it also never comes up in any of the adaptations. The Stand has been published in two different versions, made into a comic book series, and twice been developed into a miniseries for television. In each one, the virus is referred to as Captain Trips on several occasions. It even appears in King's short story " Night Surf ," that was published in 1969 and served as inspiration for the larger epic. In the 2020 miniseries version of The Stand (made for CBS All Access), the term Captain Trips is used in the first episode.
Perhaps one of the most likely origins of the term Captain Trips is a reference to Grateful Dead guitarist Jerry Garcia. In his day, Garcia had the nickname "Captain Trips" because he was known for spiking people's drinks with hallucinogenic drugs, particularly LSD. It could also have originated with one of the pioneers of LSD, Alfred Mathew Hubbard, who has been called " The Original Captain Trips ." The theory is that contracting the superflu virus is a lot like unknowingly dropping acid and falling into a deep delirium.
One final explanation is that the term is referencing the fact that the superflu virus was developed for military purposes and that human incompetence allowed it to spread. In other words, the US army creates the virus and then a captain holding a jar of it literally trips and drops the jar, where it smashes open and brings about the end of the world. That said, it's still possible that The Stand on CBS All Access could solve this mystery once and for all, although perhaps it's better for the explanation to be left to the imagination.
Next: The Stand's Shining Easter Egg Hints At A Stephen King Universe Connection
‘The Stand’ Episode 1 ‘The End’ Spoilers: Why are Stu, Harold and Frannie not infected with Captain Trips virus?
Spoilers for ‘The Stand’ on CBS All Access and Stephen King's 1978 novel
Aptly named ‘The End’, the first episode of ‘The Stand’ spills death and doom. The one-hour dark fantasy episode begins with a prologue by Randall Flagg aka The Dark Man (Alexander Skarsgård). “The Dark Man grows stronger... He comes to destroy all who stand against him,” he says and the scene shifts to a room full of dead men crammed inside with insects buzzing around.
Based on Stephen King's book, the nine-episodic miniseries introduces a deadly virus (dubbed “Captain Trips”) that almost wipes out the population of the world. Mysteriously, Stuart Redman (James Marsden), Frances Goldsmith (Odessa Young) and Harold Lauder (Owen Teague) are among the few who aren't affected by contagious influenza. Right in the beginning, Stu is told, “The reason why I'm not wearing a mask is because you are not contagious.” Later in the episode, Harold tells Frannie after saving her from an attempted suicide, “Frannie we are the only ones remaining... That means the fatality rate for this virus is 99 percent. That means we're the future.”
The mind-boggling twist will leave one question buzzing through your mind if you haven't read King's novel: Why are Stu, Frannie and Harold not infected with Captain Trips? Ready for spoilers from the book? Well, read at your own risk.

In ‘The Stand’ — ‘Chapter 14’, Four stages of Captain Trips — a man-made virus that is later revealed to have been created by the United States Military on taxpayer dollars — varies from person to person but is highly contagious in all its stages:
STAGE ONE : No visible symptoms. However, a person may experience abnormal fluctuations in blood pressure and the appearance of “wagon wheel” incubator cells. In the book, Bob Brentwood and Eva Hodges go through the first stage.
STAGE TWO : Headache, sniffles, sneezes, mild cough are some symptoms and you may not be able to identify if differs from the flu. Although most characters, like Norm Bruett, are able to continue normal activities, but it slowly starts to affect their health with swelling in lymph glands.
STAGE THREE : With intense respiratory symptoms, painful swollen glands, high fever, it leads to a combination of mononucleosis and influenza (grading to pneumonia). Characters like Alice Underwood undergo the stage before going to bed or seeking medical help. STAGE FOUR : The tube neck is the most common symptom and it leads to pneumonic plague and cancer. As shown in the CBS All Access series, it leads to a buildup of phlegm and blood with a high fever. In the book, characters like Charles Campion and Christopher Bradenton are depicted facing these troubles before their fatal end.

But, how do the survivors remain unaffected by the virus?
As per a Fandom bio, there's no specific reason why certain people are immune to the superflu, but the date of Project Blue files in the book attributed it to genes. The description reads: “Colonel Richard Deitz, operating in Atlanta, then in Vermont after the Plague Center in Atlanta was compromised, led the effort to find a cure for the virus. Due to the fact that Captain Trips shifts and changes at an extremely rapid pace, not one attempted vaccine worked. Men and women with a lifetime of experience in medicine were mystified at Stuart Redman's survival, especially after they injected him with the superflu under the guise of administering a sedative. Redman's immune system swiftly isolated and killed the virus, but with no visible sign of how.”
As more episodes air, we may find out if the miniseries really spells out the reason why certain people are not infected by the virus. Until then, let's wait and watch.
‘The Stand’ premieres on December 17, 2020, with the first episode titled ‘The End’ and subsequent episodes in the nine-episode limited-event series will follow every Thursday on CBS All Access.
‘The Stand’: Where Does the Term ‘Captain Trips’ Come From?
CBS All Access limited series based on Stephen King’s novel premiered Thursday

The first episode of CBS All Access’ limited series based on Stephen King’s novel “The Stand” premiered Thursday, and it couldn’t have come at a more apt time. The series follows a group of survivors after a superflu knocks out 99% of the world’s population, and it hits close to home as we face the very real, though not as fatal, coronavirus pandemic.
But the superflu in “The Stand” is known by a more casual, less scientific name: “Captain Trips.” If you’re wondering where that term came from and what it means, you’ve come to the right place.
The meaning and origin behind the phrase “Captain Trips” is never directly explained in King’s book. (It should be noted that the original version of “The Stand” was published in 1978, but King released a longer, updated version in 1990 that restored sections that had been cut from the original novel. The 1990 edition is the reference point for the series’ story).
“Captain Trips” does, however, appear in the book as a colloquial phrase used by young people to identify the virus. The virus was initially created by a military biological weapons lab under the codename “Project Blue,” and is also referred to in a more scientific context as “Blue virus,” “848-AB,” “A-prime” and “A6.” Other colloquialisms used to identify the respiratory illness in the book include “the rales,” “choking sickness,” “tube neck” and simply, “the superflu.”
King has never directly spelled out the origin of “Captain Trips.” It also wasn’t explained in his original 1969 short story “Night Surf” that spawned the book, nor in the 1978 version of “The Stand” novel, in the 1994 television miniseries or in the “Captain Trips” comic book. The phrase is mentioned in the first episode of the CBS All Access limited series, but not explained.
According to some online sci-fi fan forums , the best explanation of where the phrase comes from is that it originated with the late Grateful Dead guitarist Jerry Garcia, who was nicknamed “Captain Trips” because he was known for spiking people’s drinks with hallucinogenic drugs like LSD. The nickname has also been used to describe Alfred Matthew Hubbard, a pioneer of LSD in the 1950s who was dubbed “ The Original Captain Trips.”
Without an explanation from King himself, the most likely answer is that young people in the book began referring to the disease as “Captain Trips” because its symptoms can make a person delirious, resembling a drug-induced hangover. Another theory laid out in an archived Stephen King Reddit thread surmised, “I always thought it was because of the army = weaponised [sic] flu connection, captain trips and drops a jar of plague.”
Perhaps “The Stand” will eventually solve the “Captain Trips” mystery for us — keep watching to find out.
Episode 1 of “The Stand” is now streaming on CBS All Access.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
This site uses Akismet to reduce spam. Learn how your comment data is processed .
The Stand: Captain Trips Is STILL the Most Ridiculous Name for a Fictional Virus
Captain Trips is one of the names of the virus in The Stand, and it makes no sense in universe.
WARNING: The following contains spoilers for The Stand Episode 1, "The End," now streaming on CBS All Access .
Talk to any Stephen King fan, and they will acknowledge that the master of horror sometimes has a little trouble with the endings of his novels. There is the infamous and controversial scene with the kids in the sewers from It and the somewhat deflating ending in Under the Dome . In contrast to that, naming things has never been deemed a problem. The "shining" and the town of Castle Rock seem both fitting and perfectly acceptable names, which brings us to The Stand .
It is one of King’s most famous and beloved novels, and in 2020, the novel is more relevant and timely than ever, which may pay off for its new miniseries adaptation that debuted this past Thursday. However, one thing King got wrong is the naming of the virus Captain Trips. It may be the most ridiculous name for a fictional virus ever.
RELATED: The Stand Is an Underwhelming Adaptation of Stephen King's Epic
In the real world, viruses have simple, clear names, like the coronavirus. The name for the disease it causes has the simple abbreviation of COVID-19, which stands coronavirus disease, with the 19 tacked on to represent the year it was detected. There are tons of other viruses in the world, and most of them, like Ebola, are just known by their official name. Others, like Malaria, which is also known as Yellow Fever, may have different names that refer to their symptoms, in this case yellowing skin and fever. However, in all these cases, the names are simple and to the point.
This seems to be the case for Captain Trips, at least for its other names. The US government has been responsible for developing the novel’s virus in a military laboratory under the codename "Project Blue," and it is trying to deny and deflect any responsibility and downplay the severity and lethality of the virus. Since there is no official name that is recognized, it makes sense that the media and the population itself would come up with nicknames, like superflu, choking sickness or tube neck.
RELATED: The Stand Showrunner Teases Stephen King's New Coda to the Story
It is even plausible that these multiple names would all be coined in different parts of the country, since the book’s story is set in the last quarter of the last century, when the internet was in its infancy, and local television and newspapers were fairly common then. However, the name Captain Trips seems far fetched. It sounds more like a nickname college kids would use for a drug that gives them a great "trip" than it does for a serious virus.
It has never been publically made clear why Stephen King nicknamed the fictional virus Captain Trips, but there is a chance he named it after the Grateful Dead’s late singer, Jerry Garcia. Aside from being one of the most prolific, successful authors of our time, King is also a musician and big fan music, even writing a short story based around a town full of dead musicians called "You Know They Got a Hell of a Band."
RELATED: The Stand Reveals Randall Flagg's True Role in the Apocalypse
One band he is apparently a fan of is the Grateful Dead, even comparing himself to them at one point. There's also a connection between The Stand and the Grateful Dead, which is that frontman Jerry Garcia had the nickname Captain Trips for allegedly spiking the drinks of people around him with hallucinogenic drugs.
While that doesn’t have anything to do with an illness, it seems that King could've used the nickname of the singer for his virus. It would have probably been a better idea to keep the name shelved for something else that could've had a clearer connection to the band, if this was his reasoning. If it wasn't, then the virus' name lacks any justification for why it's so ridiculous.
The Stand stars Alexander Skarsgård as Randall Flagg, Whoopi Goldberg as Mother Abigail, James Marsden as Stu Redman, Odessa Young as Frannie Goldsmith, Jovan Adepo as Larry Underwood, Amber Heard as Nadine Cross, Owen Teague as Harold Lauder, Henry Zaga as Nick Andros, Brad William Henke as Tom Cullen, Irene Bedard as Ray Bretner, Nat Wolff as Lloyd Henreid, Eion Bailey as Weizak, Heather Graham as Rita Blakemoor, Katherine McNamara as Julie Lawry, Fiona Dourif as Ratwoman, Natalie Martinez as Dayna Jurgens, Hamish Linklater as Dr. Jim Ellis, Daniel Sunjata as Cobb and Greg Kinnear as Glen Bateman. The Stand releases new episodes Thursdays on CBS All Access.
KEEP READING: The Mandalorian Makes Clerks' Best Argument Star Wars Canon
‘Tripledemic:’ What Happens When Flu, RSV, and COVID-19 Cases Collide?
BY CARRIE MACMILLAN January 12, 2023
Doctors share tips on how to stay healthy this winter.

[Originally published: Nov. 22, 2022. Updated: Jan. 12, 2023]
Note: Information in this article was accurate at the time of original publication. Because information about COVID-19 changes rapidly, we encourage you to visit the websites of the Centers for Disease Control & Prevention (CDC), World Health Organization (WHO), and your state and local government for the latest information.
Last fall, as a common respiratory virus surged in children across the country, flu cases climbed, and COVID-19 simmered in the background, some medical experts worried about a potential “tripledemic.”
There’s no scientific definition for this term; it simply refers to a collision of RSV (respiratory syncytial virus), flu, and COVID-19 to the extent that it might overwhelm hospital emergency departments.
While all three viruses are present right now, they aren’t each peaking at the same time. Pediatric RSV and flu cases are now down; COVID-19 continues to increase in adults; and cases of adults with flu are declining in the elderly and somewhat stable among younger adults.
A big part of the flu increase in November, explains Scott Roberts, MD , a Yale Medicine infectious diseases specialist, was our lack of immunity from having not been exposed to the virus for several seasons due to masking and other precautions, many of which have fallen to the wayside.
We asked Dr. Roberts and Thomas Murray, MD, PhD , a Yale Medicine pediatric infectious diseases physician, more questions about how we can stay safe, especially as we spend more time indoors this winter.
What is happening with RSV and children?
RSV is a common and highly contagious respiratory virus that causes cold-like symptoms. Most kids are exposed to the virus by their second birthday and therefore develop a degree of immunity that makes future cases less troublesome.
Typically, kids and adults (who can still get it) recover within a week or two. “For the average healthy child, being under age 2 increases the risk of hospitalization. But even having said that, the vast majority of kids do not get hospitalized,” says Dr. Murray.
However, it can be more serious for the extremely young and very old, as well as anyone with a compromised immune system or underlying health conditions, such as congenital heart disease or cancer.
Plus, because of COVID-19 precautions, many young children haven’t been exposed to the virus in the last few years, but now with restrictions lifted, many are being infected. And in younger children, especially those less than 3 years old, it can lead to breathing difficulties because their lungs aren’t fully developed.
The good news, says Dr. Murray, is that this is not a new virus and health care providers know exactly how to take care of kids with RSV.
The problem last fall, Dr. Murray says, was the volume of sick children.
“Kids can get quite sick from it, but we know how to help them,” he says. “Children are admitted to the hospital for extra oxygen or other supportive measures such as positive pressure to help with breathing and keep the lungs open.”
There is no vaccine for RSV but there are several in development. Babies born prematurely or with an underlying medical condition may qualify for RSV antibody injections to help prevent severe disease.
What steps can we take to prevent illness?
Flu, COVID-19, and RSV are all respiratory viruses, but there are differences in how they spread.
“With COVID, we have appropriately focused on air quality, but many of these viruses can also spread by touching contaminated surfaces, which makes handwashing and cleaning contaminated surfaces really important,” Dr. Murray says.
Dr. Roberts agrees. “At the beginning of the pandemic, we were wiping down our fruit, vegetables, and everything with bleach, until we found out that COVID doesn’t spread through surfaces—but rather from sneezing, coughing, and expelling respiratory droplets and aerosols,” he says. “RSV spreads much more through contaminated surfaces. A kid rubs snot on their hands and puts the hand on someone else, and then that kid puts their hand in their mouth, and they can be infected. Handwashing and cleaning surfaces are more critical with RSV than with COVID.”
Flu, on other hand, is somewhere in the middle, and can spread from respiratory droplets, aerosols, and through contaminated surfaces, Dr. Roberts says. It’s important, therefore, to practice what the Centers for Disease Control and Prevention (CDC) calls “respiratory etiquette,” Dr. Murray says. “That means coughing into a tissue and disposing of it immediately in the garbage,” he says.
It may sound obvious, but the best prevention advice for all three illnesses is to avoid others who are sick. “And if you or your child is sick, stay away from others until you are improving and fever-free,” Dr. Murray says. “And if you have a baby, especially a newborn, be very careful about who visits in their first couple months of life. You only want people who are washing their hands and have no symptoms to be near the baby.”
How can we gather safely with others?
With colder weather keeping more people inside, it’s important to take certain precautions, doctors say. First and foremost, now is the time to get your flu shot and make sure you are up to date on your COVID-19 vaccination , including the new bivalent booster.
“The influenza vaccine may not completely prevent you from getting the flu, but it has a really good chance of keeping you from getting seriously ill and being hospitalized and dying,” Dr. Murray says.
If you are going to an indoor gathering, Dr. Roberts advises taking extra precautions in the week leading up to it. “In other words, don’t go to a big, indoor concert with tons of people shouting, where your odds of exposure to COVID or something else will be very high,” he says. “Plus, you can take a rapid test right before you go in the room for a gathering. If everybody does that, it’s an added layer of security. And if you are traveling, wear a mask, even if nobody else does.”
Dr. Murray says it’s also important to pay attention to symptoms. “If you have any symptoms, you really should not congregate with others. But if you insist, wear a mask and segregate yourself during activities such as eating, when you can’t be masked,” he says.
What is happening with COVID-19?
The COVID-19 variant XBB.1.5, yet another descendent of Omicron, is quickly spreading in the U.S. and has been described as the most transmissible form of the virus yet.
However, there is not yet evidence to suggest that it causes any more severe disease than other Omicron strains.
When should you call your child’s pediatrician?
“When your child starts to have cough and fever, it's always good to reach out to your pediatrician, to be in touch, says Dr. Murray. “That's very important. With babies, if you see really fast breathing or any blueness around the lips or what we call use of accessory muscles, which is if you start to see the shoulder blades when they're breathing or see the belly really going up and down really fast, or if the baby looks uncomfortable, those are reasons to come to the emergency room,” he says.
In the end, families need to be prepared that the hospital is a very busy place right now, he adds.
“If your child still looks well, then it's really important to start with your pediatrician. But certainly, if you're concerned, the emergency room evaluates your child quickly to see how sick they are,” Dr. Murray says. “And if they're quite sick, they will be seen faster.”
Information provided in Yale Medicine articles is for general informational purposes only. No content in the articles should ever be used as a substitute for medical advice from your doctor or other qualified clinician. Always seek the individual advice of your health care provider with any questions you have regarding a medical condition.
More news from Yale Medicine
Can ‘strategic masking’ protect against covid-19, flu, and rsv.

How Anti-Obesity Medications Can Help With Surgery

The Updated COVID Vaccines Are Here: 9 Things to Know

Let’s Talk About Bad Trips: Separating Difficult from Traumatic
Bad trips are a polarizing concept in psychedelics. acknowledging that they exist - and knowing how to work with them - can be healing..

Want to start a war on social media? Post something like this: “Bad trips exist.”
As somebody who has worked in the psychedelic space for years now and has supported many, many people during their trips, it’s time to come out of the closet and say it: people can be harmed by psychedelics, and bad trips exist.
But allow me to define the term “ bad trip ,” because the vague phrase has become too polarized to be meaningful.
When I talk about bad trips, I’m not talking about the harrowing, painful journeys to the underworld from which we return raw and exhausted, with some important piece of our healing work having been catalyzed.
When I talk about bad trips, I mean the trips that register in the body as a trauma or injury to the nervous system. And that is not , in fact, the same thing as a difficult trip.
What happens when we deny this truth is that we inadvertently alienate those who have had traumatic or harmful experiences. These people have endured a trauma, and are now being told that they have not.
So let’s talk about traumatic trips: The psychedelic experiences that leave us injured. Thankfully, they are rare.
I’m not just speaking from my observations as a clinician, but also from personal experience: I had a traumatic psychedelic experience on ayahuasca many years ago. I was decidedly “not okay” afterwards and required much time and support to recover.
Despite the shock and injury to my nervous system, I eventually used psychedelics again. In fact, in the eight or so years that have passed since the traumatic trip, I have openly supported the legalization of psychedelics, and have built two businesses centered around empowering people to heal with psychedelics.
I have also taken sabbaticals from my practice to work in other countries as a psychedelic facilitator. I am now a lead educator in the country’s first training program for psilocybin facilitators to be licensed by Oregon’s Higher Education Coordinating Commission (HECC). I’m a ketamine prescriber, and I train other prescribers in the use of ketamine for treating chronic pain and mood disorders. I lead and run intensive healing retreats. I’ve also taken my own fair share of mind altering substances in a variety of sets, settings, and time zones.
All of which is to say: I am no newcomer to the world of psychedelics.
And yet I cannot swallow the field’s echo-chamber-like mantra that “there is no such thing as a bad trip .” In fact, I find the rabidity with which some of my fellow cosmonauts deny the existence of bad trips to be rather disconcerting. In the more-than-one heated debate I’ve had about this topic, I’ve noticed certain patterns – or myths, if you will – around the topic of traumatic trips. I address each one here.
Myth: Bad Trips Only Happen When the Set and Setting Are Improper
If the word “only” didn’t appear in the above sentence, it would be true. In my experience in working with hundreds of patients who have used psychedelics – and in administering psychedelics myself – I’ll say that the vast majority of traumatic trips happen when the environment is not safe, calm, and supportive.
When we talk about set and setting in psychedelic harm reduction , we mean two things: (1) the person’s mindset when they took the drug, and (2) their physical environment. If somebody had just had an argument with their spouse before taking LSD, for example, that’s their set. If they were at a noisy, crowded music festival, that’s the setting. Perhaps unsurprisingly, the majority of bad trips happen when individuals on drugs feel overwhelmed in a noisy, chaotic setting like that of a concert or party. Drug-drug interactions are also often at play during difficult trips, for example, when people combine alcohol with psychedelics.
When people insist a little too strongly that, “There’s no such thing as a bad trip, if the set and setting are right,” I feel uneasy. It’s perhaps like asking a rape survivor, “Yeah, but what were you wearing?” (If you think the analogy of a bad trip and rape is too far of a reach, you luckily have never had a traumatic trip.)
There are other factors in psychedelic harm reduction that influence the outcomes. These include the substance being used, the dosage taken, and the people you’re with.

The night of my traumatic trip was the third of a three-night ayahuasca ceremony. I was there with my then-partner. I liked the other people attending. I trusted the facilitators completely and knew they were well trained and highly esteemed by their colleagues. The medicine was pure. The environment was soothing and well contained. The music was beautiful. The first half of the third ceremony was trippy, strange, and lovely.
After I drank my second dose of the brew, however, I was decidedly NOT OKAY. I will not describe the experience here, but I will say two things about it: (1) I felt like my nervous system was being gang raped, repeatedly, and (2) I can now absolutely understand why people with psychosis sometimes choose to die by suicide.
The facilitators of the circle took care of me, pulling me out of the ceremony space and letting me try to calm down outside. Somebody stayed with me at all times until I vomited up the salt water they gave me to drink.
There’s one factor of harm reduction we don’t discuss enough: dose. It’s possible that the second cup of ayahuasca I drank that night contained more voltage than my nervous system could handle – that it was too much, too fast, and too hard for me.
The Influence of Neuroticism
Aside from the environment, another factor that can predict bad trip potential is neuroticism. Neuroticism is one of the “Big Five” traits thought to collectively form the full picture of personality.
People who score high on neuroticism tend to overthink things, typically have a hard time relaxing, and may feel irritated in noisy settings or stressful situations. These folks are often described as “high strung.”
At least two studies have shown that people who score high on neuroticism scales are more likely to have a challenging psychedelic trip than those who score lower. [1] , [2] The theory behind this is that if a neurotic’s negative thoughts or feelings arise during a psychedelic trip, the person might get pulled into an amplification spiral of their own negativity.
But does that mean it’s somebody’s fault that if they tend towards neurosis and they have a bad trip? Aren’t psychedelics supposed to help heal negativity? What does it mean that the same drugs that help soothe negative thoughts and feelings can also make us feel worse? (Let a neurotic chew on that one.)
Once again, we could very easily slip into the territory of victim blaming if we are not mindful.
While writing this article, I took the Big Five Personality Test online. I scored in a higher-than-average percentile for negative emotionality (neuroticism). That may explain why grumpy cat is one of my heroes and why my friend Greg refers to me as “a female Larry David.” It could also explain why I’m one of the unlucky few who have had a traumatic psychedelic trip. (Side note: I also scored pretty high on open mindedness, so that could explain why got into psychedelics in the first place.)
Myth: Bad Trips Are Actually Just Difficult Experiences That Haven’t Been Integrated
I continue to stay in this field because traumatic trips are, indeed, exceedingly rare, and because the healing gains people typically experience from psychedelics are unparalleled by any other intervention I’ve found.
Working regularly with patients in non-ordinary states of consciousness, I see that the most challenging experiences are often the most rewarding. Drawing from my previous experiences in volunteering with the Zendo Project and White Bird , I teach my students the tenants of “trip sitting.”
As one of the Zendo principles states: difficult is not necessarily bad. Note that the phrase is not “difficult is not bad,” but rather, “ difficult is not necessarily bad. ” In other words, difficult can sometimes be bad.
Another layer to this argument is that if you wait long enough, the bad experience will prove itself to be good. This does, indeed, happen to many people after their challenging journeys. Yet there is a difference between suggesting this to a bad trip survivor and insisting that “everyone gets the trip they need.”
Many of my new-age peers have become allergic to the word “bad,” especially within the context of bad trips. “Is anything really bad?” I’m often asked. The argument here, as I understand it, is that with every cloud there comes a silver lining, and that silver lining might just hold a very valuable teaching for us.
I admit that my own traumatic trip gave me a lesson: It taught me that there is indeed such a thing as a bad trip. Another gift was that my bad trip helped me to better understand, validate, and support others who have been harmed by psychedelics. Another lesson was this: my bad trip was an amplifier of the toxic positivity that I see running rampant in the psychedelic field.
In fact, a patient once confessed to me, “I’m just so mad at her” – her being ayahuasca – “but everyone in the group is so in love with Great Grandmother that if I say one bad thing about her, it’ll be like heresy.” I noticed that he was clenching his jaw and only breathing into the upper part of his chest. I leaned forward, looked him in the eye, and said: “Tell me exactly what you think about that bitch – you won’t offend me.”
By the end of the hour, he had raged, wept, and laughed. His breath was reaching his abdomen and his jaw was relaxed. The client messaged me some days later, saying, “That was so healing for me just to be heard, to be able to say mean things without being afraid somebody would cancel me. Thank you.”
Perhaps for this client, “the medicine” was to be heard without anybody trying to stop him from expressing anger. Maybe the bad trip was just part of the arc that took him to that finale. I don’t know.
Myth: There’s No Such Thing as Bad
There’s that old story about the Zen master, whose son got a new horse. “What good luck!” The neighbors said. “We’ll see,” said the master. One day the son was thrown from the horse and broke his leg. “How terrible!” Said the neighbors. “We’ll see,” said the master. Then the country went to war, and the army came to recruit soldiers. Because the young man’s leg was broken, they army didn’t take him to battle. “How good!” said the neighbors. “We’ll see,” said the Zen master. Perhaps there is no good or bad.
What I’ve always found lacking in this story about the Zen master was the voice of his son – the one who actually fell from the horse.
Is a bad trip like falling from a horse? It absolutely can be. Yet something about the “you just haven’t integrated it yet, there’s gold there” argument feels like a dismissive bypass. Let us consider other situations in which we could apply such a statement:
- After getting food poisoning and vomiting for hours
- After taking penicillin and breaking out in a full body rash
- After going on a horrible date
- After surviving a sexual assault
- After your child has been diagnosed with a life-threatening illness
- After losing a loved one to cancer
- After surviving a terrible accident that has resulted in disability
- After your cat has been run over by a car
- After losing a house to foreclosure

Would we really tell the people in the above hypothetical situations that there was no such thing as bad shellfish? No such thing as a bad drug reaction or a bad date? No such thing as rape? No such thing as a bad diagnosis, a bad prognosis? Or how about just a bad day? Or something as non-threatening as a bad movie, a bad haircut, or a bad parking job? Would we really tell somebody whose child just died to avoid using the word “bad” to describe her condition?
Perhaps it is true that none of these things are bad, and that all of them are blessings in disguise. But would we really get righteous about it on social media, the way some of us do about denying bad trips?
And what’s so bad about saying “bad,” anyway? Must everything truly be a blessing? (The neurotic writing this article needs to know.)
I’d also like to share the story of Becks. Becks was a 24-year-old female patient of mine with anorexia nervosa who did MDMA-assisted psychotherapy to heal from PTSD (post-traumatic stress disorder) rooted in childhood sexual abuse.
In a follow-up visit, Becks told me that the MDMA-assisted therapy session (done with an underground provider) had done wonders for her. She was getting much more mileage out of her weekly therapy sessions. She was now remembering things she had repressed previously, and she was able to stay present when the memories arose.
Becks had also forgiven herself. She explained that without realizing it, she had blamed herself for what happened to her when she was a child, punishing herself through self-denigrating thoughts, food restriction, and high-risk drinking. Her MDMA-assisted therapy session helped her identify this pattern and realize that she didn’t deserve the blame or the punishment. Having forgiven herself, Becks was now sleeping better at night, eating when she was hungry, and avoiding alcohol. Clearly, much healing had occurred for her.
Yet Becks felt discouraged and worried. “I don’t think I’m doing it right,” she told me while pulling at the rings on her fingers.
“Why’s that?” I asked.
“Well,” she explained, “I know I’m supposed to get to this place where I feel like the trauma was a blessing – and that hasn’t happened.”
“You think you’re supposed to get to a place where you think that being repeatedly molested as a child is a blessing? ” I asked her.
“Yes,” she said with a defeated sigh as she looked at her shoes.
“Where’d you get that idea?”
Her head snapped up to look at me, breathless, huge-eyed. And then she burst out laughing. The laughter turned to tears. She sobbed and babbled something about a podcast she’d heard. Then she laughed some more. Her face lit up and the color returned to her cheeks.
“Becks, was being molested by your stepbrother every night a blessing?” I asked her.
“No, it was a fucking horrible nightmare that I wouldn’t wish on my worst enemy,” she declared.
“Okay,” I said, “and is it possible that it was a fucking horrible nightmare and that you still get to heal and have a happy adult life starting right now?” I asked.
“ Fuck yeah,” she said. And the look on her face told me she believed it.
(This, by the way, is what happens when you go to a doctor who scores high on neuroticism scales: We acknowledge and celebrate that life might be a fucked up mess sometimes, and that we can still heal even if we don’t buy into toxic positivity.)
(Also: I do have patients who come to see their traumas as gifts. It truly is a powerful and important step in their healing. But let’s not assume that healing cannot happen in other forms. Everyone’s path is different and valid.)
Myth: Talking About Bad Trips Is Going to Harm the Psychedelic Movement
On the day I graduated from medical school, I took an oath to First, Do No Harm . Sometimes, First, Do No Harm means doing the uncomfortable thing or saying what others don’t want to hear. In this case, it means acknowledging that there are risks to using psychedelic substances, and a traumatic trip is one of those risks.
Every therapy, every medicine, every experience comes with risks and benefits. One risk of taking vitamin C is that too much can cause diarrhea. One risk of antibiotics is that they can lead to vaginal yeast infections. One risk of using acetaminophen (paracetamol) is that it’s hard on the liver. One risk of eating a vegan diet is that it can deplete vitamin B12 stores and subsequently trigger depression. One risk of a life-saving surgery is that it can result in a lethal infection. And so forth.
Psychedelic medicines also come with their risks, and the risk of a traumatic trip should be on that list. Admittedly, it should be in small letters, towards the bottom of the list, next to the words “very rare when used in therapeutic contexts.” But traumatic trips are, in fact, “a thing.” They’re part of the fine print.
As far as I know, bad trips have not been reported in any of the clinical trials on psychedelics – but keep in mind that we haven’t had too many people go through the clinical trials as compared to the number of folks doing psychedelics “in the wild.” Bad trips may have also been down-played in the trials as “dysphoria” or “agitation” by the researchers.
Are the possible risks of psychedelic medicines worth wagering for the potential benefits? The answer to that question can only be answered on a case-by-case basis – as with any intervention.
For me personally: The healing engendered by psychedelics has far outweighed and more than redeemed the harm I’ve endured. Every time I take a psychedelic medicine now, I understand that I am taking a risk, and I make the clear, informed decision to proceed – or not to proceed, depending on the circumstance.
When I advocate for the destigmatization and legalization of psychedelics, furthermore, I don’t just act out of love for the movement: I act out of love for my patients.
What’s going to injure the psychedelic movement even more than a level-headed discussion about traumatic trips is the harm that may be caused by denying them.
How to Talk to a Bad Trip Survivor
So, what should we say to a survivor of a traumatic trip? Anything but: “There’s no such thing as a bad trip.”
If somebody tells you they’ve endured a bad trip, treat them as if they’d just told you that they survived an accident, an assault, or another kind of shock. Offer them comfort and support. Listen. Don’t ask them to prove the truth of what they say happened.
Essentially: treat them as you would treat the survivor of any kind of experience that was too much, too hard, and/or too fast for their mind, body, or spirit.
Remember that the word “trauma” does not refer to the distressing event itself, but rather to the resulting emotional and neurological response. Trauma can harm a person’s sense of Self, their sense of safety, their ability to navigate relationships, and their ability to regulate their emotions. Trauma, in other words, is injury to the nervous system that ripples outward. (To be clear: Trauma does not mean simply feeling uncomfortable or offended, as some people mistakenly use it.)
Even if integration of the experience would be helpful for the survivor – and might even help them stop using the term “bad trip” to describe it – that cannot happen at the beginning. The first thing the bad trip survivor likely needs is to know that they are safe now . The nightmare has ended, and they are loved and supported by trustworthy people who care.
How can we help others feel safe? By our presence. By regulating our own breath. By listening. By letting them know that we believe them. By showing empathy. By making them soup, gifting them a massage, or offering to pick their kids up from school. By being kind.
Even if the traumatic trip was the result of poor planning, improper set and setting, or other user error, hold your tongue for now. Think of how you might react if a friend was in a terrible car accident that resulted from driving when they were overly tired.
Think of how you might respond if a child dragged a chair to the kitchen counter and climbed atop it to try and reach the off-limits cookie jar sitting high up on a shelf – only to tumble backwards and slam onto the floor. Would you shout, “Well, that’s what you get for climbing on the chair!” while the poor kiddo cried on the linoleum? I hope not. I hope you would sit by their side, hug them, and stroke their hair. Once you felt their breathing return to normal and the smile return to their face – and not a second sooner – might you ask, “Honey, remember what we said about climbing on the furniture?”
Healing From My Bad Trip
It took me almost eight years to feel like I had fully integrated my bad trip. Curiously, what helped me complete the arc from wound to health was a peyote ceremony.
What prolonged my healing was people insisting that there was no such thing as a bad trip. I heard this line in my ayahuasca circle, at psychedelic conferences, on social media, on podcasts, and in books. The experience-denying and victim-blaming made me feel angry and alone.
Another factor that delayed my full recovery was peer pressure. Buckling to the well-intentioned insistence of friends, I returned to the ayahuasca circle (and other psychedelic circles) sooner than I truly wanted to. This meant that I was taking medicines with a mindset of doubt and fear, which resulted in several dysphoric, confusing, and terrifying journeys that only compounded the injury.
I was fortunate to find a healer who believed in bad trips and who confirmed that I was not fully in my body. Through regular sessions, I was able to return. While my therapist hadn’t had much psychedelic experience herself, she at least believed me. That allowed us to start from a place of trust and not from a place of defensiveness. I also took a break from psychedelics and instead cultivated gentler, more predictable health-affirming practices like singing and going to the gym.
Years after the experience, I read about the concept of “too much, too hard, too fast” in a book about psychedelic facilitation. I felt a surge of heat rush to my face as I read the words; hot tears filled my eyes. I hadn’t made it up. It had happened to me. I wasn’t weak, or stupid, or crazy. But why was the truth so hard for other people to accept?
I’m grateful to my own stubborn will to get better – to that spark within me that keeps me seeking out people, places, and things that can help me heal, grow, and learn.
There was, indeed, some good that came from my bad trip on ayahuasca all those years ago. The seams of that horrific shroud were sewn with golden thread. I am grateful for the blessings gleaned.
I am also grateful to my unconditionally supportive family, friends, and partner, and to Grandfather Peyote for helping me weave the blessings into my life and pull back the heavy curtain.
I had a bad trip, and that’s okay.
And you know? Considering that I’m a neurotic, I’m pretty proud of myself for saying so.
Follow your Curiosity
[1] Barrett FS, Johnson MW, Griffiths RR. Neuroticism is associated with challenging experiences with psilocybin mushrooms. Pers Individ Dif. 2017 Oct 15;117:155-160. doi: 10.1016/j.paid.2017.06.004 .
[2] Petter Grahl Johnstad (2021) The Psychedelic Personality: Personality Structure and Associations in a Sample of Psychedelics Users, Journal of Psychoactive Drugs, 53:2, 97-103, DOI: 10.1080/02791072.2020.1842569
You may also be interested in:

Harm Reduction

Mental Health

- Patient Care & Health Information
- Diseases & Conditions
- Traveler's diarrhea
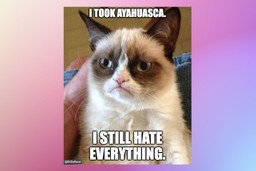
Gastrointestinal tract
Your digestive tract stretches from your mouth to your anus. It includes the organs necessary to digest food, absorb nutrients and process waste.
Traveler's diarrhea is a digestive tract disorder that commonly causes loose stools and stomach cramps. It's caused by eating contaminated food or drinking contaminated water. Fortunately, traveler's diarrhea usually isn't serious in most people — it's just unpleasant.
When you visit a place where the climate or sanitary practices are different from yours at home, you have an increased risk of developing traveler's diarrhea.
To reduce your risk of traveler's diarrhea, be careful about what you eat and drink while traveling. If you do develop traveler's diarrhea, chances are it will go away without treatment. However, it's a good idea to have doctor-approved medicines with you when you travel to high-risk areas. This way, you'll be prepared in case diarrhea gets severe or won't go away.
Products & Services
- A Book: Mayo Clinic Book of Home Remedies
- A Book: Mayo Clinic on Digestive Health
Traveler's diarrhea may begin suddenly during your trip or shortly after you return home. Most people improve within 1 to 2 days without treatment and recover completely within a week. However, you can have multiple episodes of traveler's diarrhea during one trip.
The most common symptoms of traveler's diarrhea are:
- Suddenly passing three or more looser watery stools a day.
- An urgent need to pass stool.
- Stomach cramps.
Sometimes, people experience moderate to severe dehydration, ongoing vomiting, a high fever, bloody stools, or severe pain in the belly or rectum. If you or your child experiences any of these symptoms or if the diarrhea lasts longer than a few days, it's time to see a health care professional.
When to see a doctor
Traveler's diarrhea usually goes away on its own within several days. Symptoms may last longer and be more severe if it's caused by certain bacteria or parasites. In such cases, you may need prescription medicines to help you get better.
If you're an adult, see your doctor if:
- Your diarrhea lasts beyond two days.
- You become dehydrated.
- You have severe stomach or rectal pain.
- You have bloody or black stools.
- You have a fever above 102 F (39 C).
While traveling internationally, a local embassy or consulate may be able to help you find a well-regarded medical professional who speaks your language.
Be especially cautious with children because traveler's diarrhea can cause severe dehydration in a short time. Call a doctor if your child is sick and has any of the following symptoms:
- Ongoing vomiting.
- A fever of 102 F (39 C) or more.
- Bloody stools or severe diarrhea.
- Dry mouth or crying without tears.
- Signs of being unusually sleepy, drowsy or unresponsive.
- Decreased volume of urine, including fewer wet diapers in infants.
It's possible that traveler's diarrhea may stem from the stress of traveling or a change in diet. But usually infectious agents — such as bacteria, viruses or parasites — are to blame. You typically develop traveler's diarrhea after ingesting food or water contaminated with organisms from feces.
So why aren't natives of high-risk countries affected in the same way? Often their bodies have become used to the bacteria and have developed immunity to them.
Risk factors
Each year millions of international travelers experience traveler's diarrhea. High-risk destinations for traveler's diarrhea include areas of:
- Central America.
- South America.
- South Asia and Southeast Asia.
Traveling to Eastern Europe, South Africa, Central and East Asia, the Middle East, and a few Caribbean islands also poses some risk. However, your risk of traveler's diarrhea is generally low in Northern and Western Europe, Japan, Canada, Singapore, Australia, New Zealand, and the United States.
Your chances of getting traveler's diarrhea are mostly determined by your destination. But certain groups of people have a greater risk of developing the condition. These include:
- Young adults. The condition is slightly more common in young adult tourists. Though the reasons why aren't clear, it's possible that young adults lack acquired immunity. They may also be more adventurous than older people in their travels and dietary choices, or they may be less careful about avoiding contaminated foods.
- People with weakened immune systems. A weakened immune system due to an underlying illness or immune-suppressing medicines such as corticosteroids increases risk of infections.
- People with diabetes, inflammatory bowel disease, or severe kidney, liver or heart disease. These conditions can leave you more prone to infection or increase your risk of a more-severe infection.
- People who take acid blockers or antacids. Acid in the stomach tends to destroy organisms, so a reduction in stomach acid may leave more opportunity for bacterial survival.
- People who travel during certain seasons. The risk of traveler's diarrhea varies by season in certain parts of the world. For example, risk is highest in South Asia during the hot months just before the monsoons.
Complications
Because you lose vital fluids, salts and minerals during a bout with traveler's diarrhea, you may become dehydrated, especially during the summer months. Dehydration is especially dangerous for children, older adults and people with weakened immune systems.
Dehydration caused by diarrhea can cause serious complications, including organ damage, shock or coma. Symptoms of dehydration include a very dry mouth, intense thirst, little or no urination, dizziness, or extreme weakness.
Watch what you eat
The general rule of thumb when traveling to another country is this: Boil it, cook it, peel it or forget it. But it's still possible to get sick even if you follow these rules.
Other tips that may help decrease your risk of getting sick include:
- Don't consume food from street vendors.
- Don't consume unpasteurized milk and dairy products, including ice cream.
- Don't eat raw or undercooked meat, fish and shellfish.
- Don't eat moist food at room temperature, such as sauces and buffet offerings.
- Eat foods that are well cooked and served hot.
- Stick to fruits and vegetables that you can peel yourself, such as bananas, oranges and avocados. Stay away from salads and from fruits you can't peel, such as grapes and berries.
- Be aware that alcohol in a drink won't keep you safe from contaminated water or ice.
Don't drink the water
When visiting high-risk areas, keep the following tips in mind:
- Don't drink unsterilized water — from tap, well or stream. If you need to consume local water, boil it for three minutes. Let the water cool naturally and store it in a clean covered container.
- Don't use locally made ice cubes or drink mixed fruit juices made with tap water.
- Beware of sliced fruit that may have been washed in contaminated water.
- Use bottled or boiled water to mix baby formula.
- Order hot beverages, such as coffee or tea, and make sure they're steaming hot.
- Feel free to drink canned or bottled drinks in their original containers — including water, carbonated beverages, beer or wine — as long as you break the seals on the containers yourself. Wipe off any can or bottle before drinking or pouring.
- Use bottled water to brush your teeth.
- Don't swim in water that may be contaminated.
- Keep your mouth closed while showering.
If it's not possible to buy bottled water or boil your water, bring some means to purify water. Consider a water-filter pump with a microstrainer filter that can filter out small microorganisms.
You also can chemically disinfect water with iodine or chlorine. Iodine tends to be more effective, but is best reserved for short trips, as too much iodine can be harmful to your system. You can purchase water-disinfecting tablets containing chlorine, iodine tablets or crystals, or other disinfecting agents at camping stores and pharmacies. Be sure to follow the directions on the package.
Follow additional tips
Here are other ways to reduce your risk of traveler's diarrhea:
- Make sure dishes and utensils are clean and dry before using them.
- Wash your hands often and always before eating. If washing isn't possible, use an alcohol-based hand sanitizer with at least 60% alcohol to clean your hands before eating.
- Seek out food items that require little handling in preparation.
- Keep children from putting things — including their dirty hands — in their mouths. If possible, keep infants from crawling on dirty floors.
- Tie a colored ribbon around the bathroom faucet to remind you not to drink — or brush your teeth with — tap water.
Other preventive measures
Public health experts generally don't recommend taking antibiotics to prevent traveler's diarrhea, because doing so can contribute to the development of antibiotic-resistant bacteria.
Antibiotics provide no protection against viruses and parasites, but they can give travelers a false sense of security about the risks of consuming local foods and beverages. They also can cause unpleasant side effects, such as skin rashes, skin reactions to the sun and vaginal yeast infections.
As a preventive measure, some doctors suggest taking bismuth subsalicylate, which has been shown to decrease the likelihood of diarrhea. However, don't take this medicine for longer than three weeks, and don't take it at all if you're pregnant or allergic to aspirin. Talk to your doctor before taking bismuth subsalicylate if you're taking certain medicines, such as anticoagulants.
Common harmless side effects of bismuth subsalicylate include a black-colored tongue and dark stools. In some cases, it can cause constipation, nausea and, rarely, ringing in your ears, called tinnitus.
- Feldman M, et al., eds. Infectious enteritis and proctocolitis. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 25, 2021.
- LaRocque R, et al. Travelers' diarrhea: Microbiology, epidemiology, and prevention. https://www.uptodate.com/contents/search. Accessed May 26, 2021.
- Ferri FF. Traveler diarrhea. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed April 28, 2023.
- Diarrhea. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/diarrhea. Accessed April 27, 2023.
- Travelers' diarrhea. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/yellowbook/2020/preparing-international-travelers/travelers-diarrhea. Accessed April 28, 2023.
- LaRocque R, et al. Travelers' diarrhea: Clinical manifestations, diagnosis, and treatment. https://www.uptodate.com/contents/search. Accessed May 26, 2021.
- Khanna S (expert opinion). Mayo Clinic. May 29, 2021.
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
WORLD TRADE ORGANIZATION
Home | About WTO | News & events | Trade topics | WTO membership | Documents & resources | External relations
Contact us | Site map | A-Z | Search
español français
Discussion on the extension of COVID-19 IP waiver
At MC12, trade ministers adopted the Ministerial Decision on the TRIPS Agreement, which gives members greater scope to take direct action to diversify production of COVID-19 vaccines and to override the exclusive effect of patents through a targeted waiver over the next five years. It addresses specific problems identified during the pandemic and aims to help diversify vaccine production capacity. It also contains a commitment that no later than six months from the date of the decision (17 June), members will decide on its possible extension to cover the production and supply of COVID-19 diagnostics and therapeutics.
Many members took the floor to welcome the successful outcome at MC12, saying it proved that WTO members can put aside differences and work together to respond to the most urgent health challenges.
A group of developing members who support an extension of the waiver to cover COVID-19 diagnostics and therapeutics circulated a proposal at the meeting including an indicative timeline for the TRIPS Council's next steps in this regard.
These members argued that the waiver on COVID-19 vaccines falls short of their expectation and is not enough to help developing countries comprehensively address current and future health challenges. Equitable access to therapeutics and diagnostics, as pointed out by the World Health Organization (WHO), is critical in helping detect new cases and new variants. They said this waiver extension needs to be discussed with a sense of urgency given the fact that many least developed countries (LDCs) lack access to life-saving drugs and testing therapeutics.
Many developing countries supported the initiative. They highlighted the joint statement made by the three Director Generals of the WHO, the World Intellectual Property Organization (WIPO) and the WTO in June 2021 reaffirming their commitment to intensifying cooperation in support of access to medical technologies worldwide to tackle the COVID-19 pandemic, including vaccines, therapeutics and diagnostics. There was also a shared view that the negotiation process for the waiver extension should be open, inclusive and transparent.
Other members cautioned that more time was needed to conduct domestic consultations on a possible extension of the waiver to therapeutics and diagnostics. Some members also flagged the importance of an evidence-based negotiation as there was no evidence that intellectual property did indeed constitute a barrier to accessing COVID-19 vaccines. Some also reiterated the need for members to fully make use of all the flexibilities that already exist in the TRIPS Agreement (including compulsory licensing) before requesting new flexibilities.
The chair, Ambassador Lansana Gberie (Sierra Leone), asked members that were ready to engage to commence discussing this matter in various configurations. He encouraged members to individually report on progress to the General Council meeting on 25-26 July while some members may need more time to deliberate on the matter, he noted. The chair will inform members how best to structure discussions on this matter going forward, he added.
Members also agreed to continue exchanges under the agenda item of IP and COVID-19 so that the TRIPS Council can keep abreast of new IP measures in relation to COVID-19 and share relevant experience. The Council also decided that the Secretariat will continue compiling and updating all COVID-related IP measures in its document “ COVID-19: Measures regarding Trade-Related Intellectual Property Rights ” to serve as the basis for members' exchanges.
Members noted that this exercise is also in line with the Ministerial Declaration on the WTO Response to the COVID-19 Pandemic and Preparedness for Future Pandemics which provides for ongoing analysis of lessons learned and challenges experienced during the COVID-19 pandemic within the relevant WTO bodies.
IP and innovation: IP licensing opportunities
Under an item on IP and Innovation which had been requested by Australia, Canada, the European Union, Hong Kong China, Japan, Singapore, Switzerland, Chinese Taipei, the United Kingdom and the United States, the co-sponsors presented their new submission with a focus on IP licensing opportunities ( IP/C/W/691 , circulated on 23 June).
The co-sponsors highlighted several major ways owners of IP assets can secure a broader reach for their products and services through licensing agreements, which enable IP owners to allow the licensee to make or sell the invention during the licence period. This includes licensing of patents, copyright, trademarks and know-how.
The proponents shared experiences on how to apply different licensing models and build up a friendly ecosystem to foster IP trading. To overcome the knowledge gap and complexity of implementing IP licensing, these countries have developed various toolkits to provide training, online guidelines, contract templates, legal services and dispute settlement so that small businesses and individuals can effectively participate in IP partnerships.
Members welcomed the discussion on IP innovation and IP licensing, with some sharing their domestic practices. WIPO introduced its recent activities in support of IP licensing, including the establishment of an IP and innovation ecosystems sector, the work of the WIPO arbitration and mediation centre, and guidance to help start-ups develop their IP strategy.
Non-violation and situation complaints
WTO members welcomed the decision adopted at MC12 to extend the moratorium on non-violation and situation complaints (NVSCs) under the TRIPS Agreement until the next Ministerial Conference (MC13). The decision tasked members to continue examining possible scope and modalities for NVSCs and to make recommendations to MC13.
This concerns the longstanding issue of whether members should have the right to bring dispute cases to the WTO if they consider that another member's action or a specific situation has deprived them of an expected benefit under the TRIPS Agreement, even if no specific TRIPS obligation has been violated.
This moratorium was originally set to last for five years (1995–99), but it has been extended a number of times since then in the absence of agreement by members on what the scope and modalities could look like if non-violation and situation complaints were to apply to the TRIPS Agreement.
At the meeting, several developing countries suggested continuing the examination of the scope and modalities of such complaints, with the aim of making it applicable to WTO dispute settlement. Some members backed the idea of seeking a permanent solution on this matter while others were concerned that allowing NVSC dispute complaints might jeopardize the flexibilities granted in the TRIPS Agreement.
More information on the TRIPS non-violation issue is available here .
Technical cooperation and capacity building
WIPO briefed the meeting on the WHO-WIPO-WTO COVID-19 Technical Assistance Platform , which offers a one-stop shop to help members and WTO accession candidates address their capacity building needs to respond to the COVID-19 pandemic.
The chair urged members to submit information on their activities in technical cooperation and capacity building as well as incentives for technology transfer by 12 September in preparation for the end-of-year annual review. Members are encouraged to use the online submission system ( e-TRIPS ) to make submissions.
Other matters
The European Free Trade Association was granted observer status for the next Council meeting.
Next meeting
The next TRIPS Council meeting is scheduled for 12-13 October 2022.

Problems viewing this page? If so, please contact [email protected] giving details of the operating system and web browser you are using.
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My watchlist
- Stock market
- Biden economy
- Personal finance
- Stocks: most active
- Stocks: gainers
- Stocks: losers
- Trending tickers
- World indices
- US Treasury bonds
- Top mutual funds
- Highest open interest
- Highest implied volatility
- Currency converter
- Basic materials
- Communication services
- Consumer cyclical
- Consumer defensive
- Financial services
- Industrials
- Real estate
- Mutual funds
- Credit cards
- Credit card rates
- Balance transfer credit cards
- Business credit cards
- Cash back credit cards
- Rewards credit cards
- Travel credit cards
- Checking accounts
- Online checking accounts
- High-yield savings accounts
- Money market accounts
- Personal loans
- Student loans
- Car insurance
- Home buying
- Options pit
- Investment ideas
- Research reports
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
- Newsletters
New on Yahoo
- Privacy Dashboard
‘The Stand': Where Does the Term ‘Captain Trips’ Come From?
The first episode of CBS All Access’ limited series based on Stephen King’s novel “The Stand” premiered Thursday, and it couldn’t have come at a more apt time. The series follows a group of survivors after a superflu knocks out 99% of the world’s population, and it hits close to home as we face the very real, though not as fatal, coronavirus pandemic.
But the superflu in “The Stand” is known by a more casual, less scientific name: “Captain Trips.” If you’re wondering where that term came from and what it means, you’ve come to the right place.
The meaning and origin behind the phrase “Captain Trips” is never directly explained in King’s book. (It should be noted that the original version of “The Stand” was published in 1978, but King released a longer, updated version in 1990 that restored sections that had been cut from the original novel. The 1990 edition is the reference point for the series’ story).
Also Read: 'The Stand' Trailer: It's Alexander Skarsgard vs Whoopi Goldberg in CBS All Access Limited Series (Video)
“Captain Trips” does, however, appear in the book as a colloquial phrase used by young people to identify the virus. The virus was initially created by a military biological weapons lab under the codename “Project Blue,” and is also referred to in a more scientific context as “Blue virus,” “848-AB,” “A-prime” and “A6.” Other colloquialisms used to identify the respiratory illness in the book include “the rales,” “choking sickness,” “tube neck” and simply, “the superflu.”
King has never directly spelled out the origin of “Captain Trips.” It also wasn’t explained in his original 1969 short story “Night Surf” that spawned the book, nor in the 1978 version of “The Stand” novel, in the 1994 television miniseries or in the “Captain Trips” comic book. The phrase is mentioned in the first episode of the CBS All Access limited series, but not explained.
According to some online sci-fi fan forums , the best explanation of where the phrase comes from is that it originated with the late Grateful Dead guitarist Jerry Garcia, who was nicknamed “Captain Trips” because he was known for spiking people’s drinks with hallucinogenic drugs like LSD. The nickname has also been used to describe Alfred Matthew Hubbard, a pioneer of LSD in the 1950s who was dubbed “ The Original Captain Trips.”
Also Read: How 'The Stand' Depicts Stephen King's Fictional Pandemic Amid a Real One
Without an explanation from King himself, the most likely answer is that young people in the book began referring to the disease as “Captain Trips” because its symptoms can make a person delirious, resembling a drug-induced hangover. Another theory laid out in an archived Stephen King Reddit thread surmised, “I always thought it was because of the army = weaponised [sic] flu connection, captain trips and drops a jar of plague.”
Perhaps “The Stand” will eventually solve the “Captain Trips” mystery for us — keep watching to find out.
Episode 1 of “The Stand” is now streaming on CBS All Access.
Read original story ‘The Stand': Where Does the Term ‘Captain Trips’ Come From? At TheWrap
Recommended Stories
2024 nba mock draft 6.0: projections for every pick following march madness.
With the NCAA tournament behind us, here's an updated look at Yahoo Sports' first- and second-round projections for the 2024 NBA Draft.
Republicans (?!?) are killing a tax cut
In a flip of the usual priorities, Senate Republicans seem likely to kill a set of tax cuts that have already passed the House and are broadly popular. Here's why.
Here’s who will pay for Biden’s student loan cancellations
Cancelling student debt is a windfall for the borrowers who benefit, but taxpayers foot the bill.
2025 Toyota 4Runner (finally!) revealed, and the new Trailhunter is extremely cool
The 2025 Toyota 4Runner is finally arriving this fall with a full lineup including returning TRD Pro and new Trailhunter. Hybrid power now available.
2024 NFL Draft guide: 32 teams, 32 needs, picks, best fits and more
What selections does your team have? What areas should it address? Who's the dream fantasy pick? We cover all that and more for every franchise right here.
Mock Draft Monday with PFF's Trevor Sikkema: Cowboys fill needs, Vikings and Broncos land QBs
We continue our 'Mock Draft Monday' series with PFF's Trevor Sikkema joining Matt Harmon the pod. Sikkema provides his five favorite picks from his latest mock draft as well as his least favorite pick. The PFF draft expert also shares what goes into his methodology when crafting a mock, especially as inch even closer to night one of the draft.
Inflation expected to remain elevated as rate cut debate takes center stage
March's CPI report is one of the most important data points the Federal Reserve will consider in its next interest rate decision.
Andrew Siciliano, face of 'Red Zone Channel,' and others out at NFL Network, per report
NFL Network is laying off four of its most popular and talented on-air personalities.
Rashee Rice didn't learn from the past, maybe other NFL players will learn from Rice
Rashee Rice should have taken a lesson from recent history.
Royals owner's wife warns team could move to Kansas after ballpark funding proposal voted down
Marny Sherman, the wife of Kansas City Royals owner John Sherman, warned that Missouri could lose both the Royals and Kansas City Chiefs after a stadium funding proposal was voted down.
Create a free profile to get unlimited access to exclusive videos, sweepstakes, and more!
Stephen King downplays comparisons between coronavirus and The Stand’s apocalyptic plague

Credit: KENZO TRIBOUILLARD/AFP via Getty Images
The coronavirus may be creating a worldwide scare — but don’t look to Stephen King for affirmation that the virus warrants the kind of global pandemonium that measures up against his own fictional horror.
The author of The Stand is taking a stand against what he views as fan overreaction in some social media corners to the threat of coronavirus, saying there’s really no comparison between the real-world illness and the rampant ravaging of more than 99 percent of Earth’s population that his made-up Blue virus (aka Captain Trips) wreaked in The Stand .
Taking to Twitter over the weekend, King struck a balance between making sure people took the coronavirus threat seriously and downplaying the idea that the world has an apocalyptic public health menace on its hands. “No, coronavirus is NOT like THE STAND,” he declared:
No, coronavirus is NOT like THE STAND. Itâs not anywhere near as serious. Itâs eminently survivable. Keep calm and take all reasonable precautions. — Stephen King (@StephenKing) March 8, 2020
Via CNBC , recent data suggests the flu-like coronavirus has a mortality rate among those it infects of 3.4 percent worldwide. And with a comparatively small proportion of the world’s population infected, imagining coronavirus as a sweeping phenomenon — one capable of toppling governments and hitting the reset button on law and order generally — appears to be on the pessimistically bleak side.
Although the emergent nature of the virus’ spread across the globe may have people seeing the potential for a pandemic, King reminded fans that coronavirus is “not anywhere near as serious” as The Stand ’s society-collapsing disease. “It’s eminently survivable,” King wrote. “Keep calm and take all reasonable precautions.”
That’s exactly what many in the entertainment world appear to be doing , even if it means a lull in what would otherwise be a busy March schedule of fun fan events. No Time to Die is bumping its Mar. 31 debut date all the way until November. Organizers of Seattle’s Emerald City Comic Con said last week the annual fan meetup will be put on hold until sometime this summer. And in Austin, SXSW has been outright canceled for the first time in its 33-year history.
This month’s annual Games Developer Conference also has been postponed until summertime, and Disney resorts in Japan, Hong Kong, and China all have been temporarily closed — even as the company says it's “carefully monitoring the evolving coronavirus situation” while it keeps its U.S. parks open.
- Coronavirus
- Stephen King
Related Stories

Did Marty Die (Twice?) in Back to the Future?

Were Back to the Future and Goonies Set on the Same Day?

Nope VFX Supervisor Dishes on Film's Creature Design

How Roland Emmerich Made Up Conspiracy Theory For Moonfall

How Resident Alien Made That George Takei Cameo Happen

Nathan Fillion's Resident Alien Cameo Explained

Why Are Parts of Oppenheimer in Black and White?

How to Stream Winnie-the-Pooh: Blood and Honey
Christian Bale Explains Why He Turned Down the Offer to Make a Fourth Dark Knight Film

Are The Harry Potter Movies Streaming on Peacock?

Land of the Lost Director on What Could've Happened in a Sequel

Why Mt. Everest May Not Be Earth’s Closest Place to Space
Recommended for you.

Linda Hamilton on Resident Alien Role: "I'm Not the Funny Girl, I'm the Straight Man"

The Classic Twilight Zone Episode That Inspired Jordan Peele's Us

Resident Alien's Alan Tudyk on Harry's New Love Interest, Edi Patterson's Blue Avian
Advertisement
Supported by
Fall Travel Trends: Have You Heard of ‘Trip Stacking’? (You Will.)
Uncertainty remains the new normal in travel this autumn driven by the rise in cases and ever-changing travel restrictions, but here are eight things you can expect.
- Share full article

By Concepción de León
After a summer in which travel accelerated rapidly, nearly reaching prepandemic numbers, fall is looking like the season of uncertainty. Increasing concern about the Delta variant, as well as a seasonal travel dip, have slowed bookings. Fear of the variant and the potential of changing regulations have prompted travelers to plan more cautiously.
International trips are being pushed to 2022, with some people monitoring conditions week by week before booking. The European Union’s announcement on Monday that it was removing the United States from its “safe list” of countries raises the question of whether European nations will reinstate restrictions.
Seth Borko, a senior research analyst at Skift Research, an arm of the Skift travel trade publication, said that while he thinks some countries — especially those dependent on international tourism — will ignore the guidance, some travelers may still be dissuaded. “The travel lists themselves reduce people’s inclination to go to those destinations,” he said.
Joshua Bush, the chief executive officer of Avenue Two Travel , a luxury travel agency based in Pennsylvania and New Jersey, said that as the virus continues to develop, “the one thing to know for certain is that everything is going to be uncertain, that things can change at any time.”
Here is what you can expect if you plan to travel this fall.
Booking a flexible ticket will be easier.
Because of the uncertainty raised by the Delta variant, said Paula Twidale, the senior vice president of travel at AAA , travelers are adopting a “wait and see approach,” delaying bookings or opting for flexible tickets.
Hopper , a travel booking app, has seen an increase in the use of its services that allow people to cancel or rebook flights free of charge. Purchases of its “cancel for any reason” add-on have increased 54 percent over the last 12 weeks and the number of people opting for its “rebooking guarantee” has grown by 50 percent since early spring.
Some airlines, like Delta and United, have reintroduced flexibility for basic economy passengers , who would not normally be allowed to change their tickets. This was a hallmark of early pandemic travel, said Scott Keyes, the founder of Scott’s Cheap Flights , a service that alerts subscribers to discounted airfares, adding that the reversal demonstrates the airline industry’s understanding of people’s skittishness in light of the Delta variant.
Some luxury travelers are opting for what some people call “trip stacking,” or buying two trips over the same time period in case one of them falls through, said Mr. Bush, who has been offering this service. Many of his clients had been forced to cancel travel plans because of regulation changes during the pandemic. Booking two trips, he said, ensures that “they wouldn’t be left out in the cold without having any trip at all.”
“Ultimately, they’re going to take both of those trips,” he said. “It just matters which is the one that is going to be most likely to come to fruition in October.”
For budget travelers thinking of trying this strategy, said Mr. Keyes, it’s important that they “come in cleareyed about what happens to the ticket they don’t use.”
Fliers are only entitled to a refund if the airline cancels the flight or there is a significant delay. If passengers cancel, airlines will typically offer travel vouchers for future use.
The only exception, said Mr. Keyes, is if you book with miles, in which case you will get back your miles and any taxes and fees if you decide not to travel.
You may have more room on the plane, but your rental car may cost more.
Both domestic and international airfares are expected to drop this fall as demand drops, said Adit Damodaran, an economist and chief travel expert at Hopper. Though flight prices do not seem to have been affected by the new E.U. travel guidelines so far, Mr. Damodaran said that if restrictions are put in place and demand declines, prices could drop further.
“I would say that the general theme going into the fall at the moment is kind of a return to the way that travel was in the spring,” Mr. Damodaran said. “What I mean by that is lower prices compared to the summer, and also a little bit more domestic travel compared to international travel.”
But prices are still high in other sectors, especially for hotels and car rentals. A recent survey by Skift Research found that 73 percent of respondents intended to take a road trip in 2020, and Mr. Borko said that the E.U. action will likely accelerate that trend.
Because so many international destinations remain closed, “what is open, there’s such a high demand,” Ms. Twidale said. “If you’re waiting for a last minute booking or a last minute deal, it’s really not a good value proposition for you to do that,” she said.
Jasmine Jordan, 31, a singer-songwriter and marketer who lives in Seattle, said that she also now spends more on travel expenses that she considered unnecessary in the past, like travelers’ insurance.
During a recent trip to Mexico, she also opted for private transportation as opposed to shuttles to minimize her interaction with people outside her party. She finds herself “paying more for the convenience and, I guess, security of just knowing you’re in tighter spaces with really just your tight knit people,” she said.
Traveling domestically? You’ll have company.
The spread of the Delta variant has made many would-be travelers wary of making international travel plans, both because of personal reservations and also out of concern that changing regulations will force them to cancel.
The European Union taking the United States off its “safe list,” for instance, raises uncertainty about whether European countries will change regulations when it comes to American visitors. But Mr. Borko said that even during the summer while Europe was open, travelers were still inclined toward domestic tourism — a trend he expects to continue.
“I think what you see in the data is when people become more fearful, of the pandemic, of Covid, to the extent they’re traveling, it tends to be more focused domestically than internationally,” Mr. Keyes said.
Mr. Damodaran, of Hopper, said that international bookings have been going down month over month on that platform, while domestic bookings have remained stable.
“Part of that is the ‘seasonality’ that we’re seeing just going into the fall,” when travel normally falls off, he said, “and the other part of that could be some impact from the Delta variant” making travelers more hesitant to book trans-Atlantic travel.
This unpredictability led Ms. Jordan, who had a trip planned to Italy this fall, to postpone it for next year. Though she and her friend, a nurse, were sure they wanted to go, they had not yet booked their flight.
“Normally, it would be way in advance,” she said, but “I think we were just slowly tip toeing, kind of feeling out week to week.” She ultimately decided that she didn’t want to risk getting stuck in another country.
The pandemic has changed her overall attitude toward travel, she said, making her more flexible to changes. “In previous years I would get so frustrated when things didn’t happen exactly how I wanted to,” she said. “After this last year, I almost feel like I’m a new person.”
Mukhaye Nangalama, a 33-year-old who works in business affairs for a record label in Los Angeles, also expressed reservations about booking international travel. “I really don’t want to go anywhere international until we kind of see how 2022 pans out,” Ms. Nangalama said. “Some foreign countries, their medical health infrastructure is not as good as here,” she said, adding that she would “hate to be stuck somewhere very far from home and not have access to certain medical care if I were to get sick.”
And the beach may be crowded.
Many travelers are gravitating toward beach vacations in the Caribbean, Mexico, Central America and Hawaii, which are close and provide an outdoor escape. Hawaii has been so overwhelmed by tourists amid rising coronavirus case numbers that Gov. David Ige urged travelers to stay away in an Aug. 23 news conference.
This is a trend that continues from last winter and spring, when travelers gravitated more toward these places because of the stringent restrictions in place in the European Union, for instance, said Mr. Damodaran.
Lia Avellino, 33, the director of a mental well-being program at the Well, a wellness center in New York, has traveled quite a bit throughout the pandemic, primarily to places near the city. But this fall, she is taking her family to Costa Rica for a beach surf vacation, their first international trip since the pandemic.
She said they got travel insurance in case they need to change or cancel the flight based on how the Delta variant affects the country, and she plans on keeping her young children masked.
Though she has family in Europe, Ms. Avellino said that she wanted to go somewhere closer to home for the family’s first international trip, “and then see how that feels for our nervous systems.”
You still may not be able to rent a car.
Businesses across the travel industry continue to struggle to rebuild their work force, so services are still being cut back and limited.
Car rental counters in airports have been condensed to include multiple brands, often operated by one or two agents, Ms. Twidale said. Airlines have cut some routes, offering fewer nonstop flights. There has also been a shortage in rental cars, which Ms. Twidale said may not resolve itself until 2022 because of a semiconductor chip shortage affecting car rental companies’ ability to upgrade or add vehicles to their fleets. And airline companies are scrambling to hire more call center employees to reduce call wait times, which are now several hours for most airlines.
“Everyone’s trying to get staff back in place, because the demand just spiked and surged,” Ms. Twidale said. “That’s going to be the challenge for a little while, not only the hiring but bringing the competency up to speed.”
JetBlue said in an email that it is currently working to “hire and train 4,000 new crew members” to meet increased demand and “the added steps Covid travel mandates have created, like verifying test results and other health documents.” And American Airlines said it is hiring “hundreds” of reservation agents to better support customers.
Budget carriers are making a play for you.
One area in which there appears to be growth is among the budget airlines, which have taken advantage of the shift toward leisure travel during the pandemic.
Mr. Keyes said that while the number of available “seat miles,” which refers to available seats, are down across major airlines compared to before the pandemic, budget airlines have actually added seat miles. Spirit has 14 percent more than it did the same time two years ago, while Allegiant has 28 percent more.
“You see the budget airlines really trying to not only bounce back quicker but really make a play to gobble up market share away from these sort of legacy airlines,” he said. “They’re seeing the travel landscape changing toward their sort of playing field.”
Budget airlines offer direct flights to popular vacation destinations and appeal to casual leisure travelers who are paying out of pocket. Legacy airlines, on the other hand, rely more heavily on business travel, which continues to lag, said Mr. Borko of Skift Research.
Still, the budget airlines have not been immune to the challenges the industry is facing. Spirit Airlines, for instance, canceled hundreds of flights in August .
Taking young children? Think road trip.
With vaccinations still unavailable for children under 12, families must calculate the risk of traveling with their young children.
“That’s why there’s a high propensity of road trips and domestic travel happening,” Ms. Twidale said. She encourages families to go places where they can have more control over their environments and limit the number of people with whom they interact, like national parks.
That’s the route that Dr. Amber Schmidtke, 40, and her family, who live in Kansas City, took during the pandemic. Over the summer, for example, she and her family packed up their camper and traveled for three weeks through Colorado and Utah. Camping, she said, is “sort of pandemic-proof.”
In March, after she and her husband got vaccinated, they booked a Labor Day trip to Hawaii with their children, 10 and 12, with another family of mixed vaccination status.
“We fully expected that there would be a pediatric vaccine by now,” Dr. Schmidtke said. But a few weeks ago, as she saw cases rise in Hawaii and reflected on how the virus has disproportionately harmed people of color, including Native Hawaiians, she decided to cancel her trip.
Dr. Schmidtke is particularly attuned to the spread of the Delta variant because of her work as a Covid researcher at the University of St. Mary in Kansas .
“I may be a little more paranoid than some parents,” she said, but “especially with unvaccinated kids, it’s just a risk that we weren’t willing to take.” She added that she didn’t want to “be responsible for any sort of outbreak” in Hawaii.
You really should be thinking about 2022.
Bookings have already started to pick up for next year. Gemma Jamieson, a spokeswoman for Skyscanner, a flight-booking app, said in an email that bookings for 2022 created in the last week were up 30 percent compared to the same time in July. The top bookings were to Cancún, London, Paris, Rome and Tokyo, indicating a continued demand for travel worldwide.
It’s too early to tell how these bookings will be affected by the European Union’s action this week. But, said Dia Adams, a travel expert at Forbes Advisor, “I do think the top line will scare some European travelers off booking their trips.”
Mr. Borko said that he anticipates a continued interest in domestic or regional travel, to places such as Mexico and the Caribbean.
“International travel is recovering very slowly and still very much below where we were,” he said, “and the sentiment about Covid has turned much more sharply negative.”
Despite the continued challenges to the travel industry, Ms. Twidale said that she’s optimistic about next year.
“Twenty-nineteen was a banner year for travel,” she said. “Twenty-twenty-two could be an even bigger banner year than 2019.”
Follow New York Times Travel on Instagram , Twitter and Facebook . And sign up for our weekly Travel Dispatch newsletter to receive expert tips on traveling smarter and inspiration for your next vacation. Dreaming up a future getaway or just armchair traveling? Check out our 52 Places list for 2021 .
An earlier version of this article referred incorrectly to the number of flights canceled by Spirit Airlines this summer. While the airline cancelled hundreds of flights in August, it did not cancel flights in that range in previous months.
How we handle corrections
Concepción de León is a travel reporter based in New York. More about Concepción de León
Order Your Almanac Today!

The Western flower thrips is one variety of thrips that can cause extensive damage on over 500 species of plants.

Become a better gardener! Discover our new Almanac Garden Planner features for 2024. It’s easy, fun, and free to try !

How to Identify and Get Rid of Thrips
Have you seen thrips damage on your plants? Here are tips for identifying and getting rid of thrips in your garden.
What Are Thrips?
Thrips are tiny insects about as fat as a sewing needle that dines on many plants worldwide. Also known as thysanoptera or thunderflies, thrips are sucking insects that can cause some damage to plants. However, their damage can be much worse when they transmit viruses to plants.
Thrips Life Cycle : The life cycle depends on the species of thrips as well as the location, host plant, and other factors. Adult thrips overwinter in plant debris, bark, or other materials. They become active in early spring and lay eggs in plant tissue. These eggs hatch after 3–5 days, and the nymphs then feed for 1–3 weeks before resting to molt in 1–2 weeks. Thrips can have up to 15 generations per year outdoors. Adult thrips live short lives of about one month.
Cicadas 2021 Are Coming. Tree and Yard Tips.
Protect your garden from cabbage worms, get rid of chiggers, ticks, and mosquitos in your yard, identifying thrips.
Adult thrips are slender and tiny, at 1 / 50- to 1 / 25-inches long. Their colors can be anywhere from yellow to brown or black, and if you try to get close to them, they will probably leap or fly away. They have narrow, fringed wings. The nymphs look like even smaller adults, though they tend to be light green or yellow rather than darker colors. Their wings are also not fully developed, and they sometimes have red eyes.
Thrips appear to be tiny dark slivers on your plants. It is hard to see their bodies well without a magnifying glass, but up close, they look a bit like lobsters. Shake them onto a white background in order to see them well.
Thrips Damage
Thrips damage includes streaks, silvery speckling, and small white patches. This happens because the thrips suck plant cells from many garden plants, flowers, fruits, and shade trees. If you have a major infestation of thrips, your plants might be stunted with damaged flowers and fruit. The damage that you notice might instead come from the virus that the thrips spread (usually tomato spotted wilt virus).

How to Get Rid of Thrips
- To keep thrips populations under control, try using yellow or blue sticky traps.
- Shaking branches to remove the thrips and catching them on a cloth underneath is one easy way to quickly remove the thrips from your plants.
- For onion thrips: Take a dark piece of paper into the garden and knock the onion tops against it; if thrips are present, you will spot their tan-colored bodies on the paper. A couple of treatments with insecticidal soap kills them. Follow the package directions. Spray the plants twice, three days apart, and the thrips should disappear.
- For fruit trees: Spray dormant oil on the trees.
- As a last resort, dust the undersides of leaves with diatomaceous earth.

How to Prevent Thrips
- For flower thrips on gladiolus: Mix 1 tablespoon Lysol household cleaner with 1-gallon water. Soak gladiolus corms in the liquid and plant while still wet to prevent thrips.
- You can plant various flowers to attract beneficial insects that are natural predators of thrips. Some good predators include pirate bugs, lacewings, and ladybugs. Learn more about attracting those predators .
- For onion and western flower thrips, try releasing minute pirate bugs or the predatory mite Amblyseius cucumeris .
- Reflective mulches can help to hide your plants from thrips.
- If there is a very big thrips problem in your area, some plants have resistant varieties.
- Try not to overfertilize plants, as this can lead to more thrips damage.
Do you have more tips for controlling thrips? Let us know below!
Christopher Burnett

ADVERTISEMENT

Beneficial Insects in the Garden

Tomato Hornworms

How long do you soak glad bulbs in the Lysol water before planting?
Hi Helen,
You will want to soak your gladiolus bulbs in the Lysol/water solution for 3 to 6 hours. Hope this helps!
I’m looking for help with Thrips and houseplants!! Started with battling fungus gnats brought in from the yard, my potting soil is free of pests.. Have gone through sticky tape, peroxide, Neem oil, mosquito bits and even Ortho Home Defense in the soil, yea, I saw the ones in the soil, it was either them or me.. I did not have this problem just 35 miles north of here… interesting! Any help would be appreciated and (I also use a couple of drops of dawn in my misting water and run a fan and dehumidifier).
Hi Blanche,
Sorry to hear about your thrips issue.
Try applying an insecticidal soap. Make sure leaves, flowers, and growing tips are well covered with the spray. You may need to apply the spray frequently until the problem is under control. You can also try a horticulture oil spray, which can help control thrips as it suffocates the insects. Just make sure to follow label directions to avoid damage to some plants that may be sensitive.
After you have applied control measures, keep plants moist and increase humidity. Plants that are kept too dry are more likely to be damaged by thrips.
I do Rose Photography and plant them around San Diego CA. The most problem we have is Trips and Spider Mites. The trip goes inside Blossom and eats juice of Rose paddles and the top of Paddles becomes black. I use BioAdvanced just reduce them. Spider Mites is also used by this brand. the water around F 98 spray back leaves can reduce them. you can see my roses using this web address. https://www.flickr.com/photos/irajnz/51961058998/in/dateposted/
Hello, well..... this is getting very....VERY sad. I have a 40ft Ficus tree covered with thrips top to bottom and dropping piles of infected Leaves everywhere. it is over 40 Years old and never had a problem. Also a 5 ft Ficus in a pot is also becoming covered 50 ft away Now has it. I have tried the yellow sticky things......No use at all. then Tried spraying. Not great outcome for either.... the leaves shrivel up and the VERY....VERY small bugs inside are alive......What is amazing is....something that small that can do this much damage is quite amazing.
@karenhinds -
I'm having the same exact issue with them biting me. They are driving me crazy. Have you found anything that helps?
Ive never been biten..this ariticle has some good idead.
I am having a terrible time with bug bites.....Can you tell me if you have found any solution??
Thank you! susan
I get bite alot too I have found out the safest thing to use is Avon Skin so soft I don't get bit when I use this I Hope it works for you
- More Comments

Experts Say This Is the Safest Mode of Transportation During COVID-19
By William J. McGee

All products featured on Condé Nast Traveler are independently selected by our editors. However, when you buy something through our retail links, we may earn an affiliate commission.
As the coronavirus pandemic rages on into its fifth month of lockdowns and canceled events, pent-up demand has many wondering about the safest way to travel, among the options that make the most sense now. Condé Nast Traveler consulted medical, travel, and statistical experts to weigh the relative risks when traveling by commercial airlines, Amtrak, and private cars during this pandemic—and they’re largely in agreement on which choices are best.
It's worth noting that these recommendations assume equality between choices. For example, some may not have the time to drive, while others may not have the money to fly, and of course it’s not an option to take a train from California to Hawaii. But for travelers able to choose among the three, the experts can help you decide the transportation method with which you're most comfortable .

To travel or not to travel
First things first: You need to determine who should travel, and if the trip is even necessary. The World Health Organization provides detailed advice on “essential travel” and lists those who should postpone or cancel trips, including older travelers and those with chronic illnesses, underlying health conditions, and confirmed diagnoses of COVID-19. In addition, the Centers for Disease Control’s “ Considerations for Travelers—Coronavirus in the U.S. ” page states: “Travel increases your chances of getting and spreading COVID-19. People at higher risk for severe illness need to take extra precautions.”
“I think we’re still learning a lot about this virus’s ability to transmit infectivity, plus the pre-symptomatic infection spread is daunting,” says Chris Hendel, a long-time medical researcher associated with the USC Gehr Family Center for Health Systems Science and Innovation.
What follows are breakdowns applicable to all three travel modes: air, rail, and highway.
The pros and cons of air travel
Risk of contracting the virus when traveling on airline starts at the airport. The CDC notes on its website that “air travel requires spending time in security lines and airport terminals," which "can bring you in close contact with other people and frequently touched surfaces." Once on board the plane, social distancing could be difficult, depending on the airline's policy. On crowded flights, where you might have to sit within less than six feet for hours, your chances for risk of exposure could go up.
But there’s also good news. “Most viruses and other germs do not spread easily on flights because of how air circulates and is filtered on airplanes,” according to the CDC. That's because the majority of aircraft in airline fleets have high-grade HEPA filters (high-efficiency particulate air) that can remove up to 99.999 percent of airborne particles. This provides extremely effective, but not perfect, protection against airborne viruses. Close contact between those on board in the aisles or while boarding—especially if some fliers aren't wearing masks—can mean exposure when air passengers exhale and, potentially, to the virus as well.
Compounding these concerns is that the U.S. Department of Transportation has failed to mandate any regulations for commercial air travel nationwide. In July the DOT issued a 44-page set of recommendations for commercial air travel, but since these are only suggestions and not enforceable, the nation’s airports, airlines, and passengers are left with a patchwork of different, and ineffective opt-in rules. In practical terms, this means airline policies on face coverings vary, and in some cases are not enforced. Members of Congress, flight attendant and pilot unions, as well as passenger advocates are calling on the DOT to mandate uniform protocols, and Consumer Reports has launched a petition that has more than 60,000 signatures.
What’s more, among the nation’s four largest airlines, currently two— Delta and Southwest —are blocking middle seats. But the other two— American and United —are not blocking them. Adding to the confusion is the fact that such seating policies also vary among smaller and foreign carriers.
This is particularly important because a recent study by Dr. Arnold Barnett, professor of Statistics at the Massachusetts Institute of Technology, found that on U.S. jet aircraft, “the risk of contracting COVID-19 from a nearby passenger is about 1 in 4,300." On planes with blocked middle seats, "that risk falls to about 1 in 7,700,” the study says. In fact, the coronavirus mortality risks for air travelers are now “considerably higher” than the threat of an airline crash, according to Barnett's study, a rather startling conclusion considering the usual statistical safety of commercial flight.

Trains have some safety advantages over planes.
The pros and cons of train travel
Amtrak offers health advantages that airlines can’t. Many stations are outdoors, there are fewer bottlenecks for check-in, and no security screening. Even so, the CDC does warn that “traveling on buses and trains for any length of time can involve sitting or standing within six feet of others.”
Last week a team of researchers from China and the U.K. published a lengthy analysis of the risk of COVID-19 transmission among train passengers. “Our study shows that although there is an increased risk of COVID-19 transmission on trains, a person’s seat location and travel time in relation to an infectious person can make a big difference as to whether it is passed on,” wrote the study's lead investigator, Shengjie Lai of the University of Southampton.
In this regard, Amtrak already has an advantage over most commercial aircraft since there are no middle seats on its trains. And a new initiative on Amtrak’s reserved trains is that bookings are limited, so that passengers traveling alone will have an empty adjacent seat. Also, Amtrak—like many airlines—states it has taken measures such as enhanced cleaning and mandatory face coverings for passengers and crew.

Jessica Puckett

Caitlin Morton

Olivia Morelli
Jim Mathews, president and CEO of the Rail Passengers Association, notes that an Amtrak coach changes the air about 12 to 15 times per hour, and supplies 15 pounds of fresh air per minute per passenger; social distancing and masks are critical factors as well. Overall, Mathews is optimistic. “We are reasonably confident Amtrak’s measures will be effective, with the proviso that they are actually followed.”
The pros and cons of car travel
When it comes to driving, the obvious advantage is that you can control who gets into the vehicle with you. But the CDC warns there could be other unforeseen risks. “Making stops along the way for gas, food, or bathroom breaks can put you and your traveling companions in close contact with other people and surfaces,” the agency notes. That said, your own car can provide much more protection than public forms of transportation, assuming you are traveling with family members or others who have been screened or vetted.
But what if it’s not your car? In the case of rental vehicles, major firms such as Avis , Enterprise , and Hertz have all pledged enhanced cleaning and social distancing upon check-in. Enterprise details 21 separate automotive parts that are sanitized, from mirrors to cupholders.
Which form of transportation is the safest way to travel?
Barnett, the MIT professor, expanded his analysis of airline empty middle seats by formulating a statistical study on traveling by car, exclusively for Traveler . “Assuming that the driver and passengers do not have COVID-19, the [highest] mortality risk of a 1,000 mile trip would arise from auto accidents," he says. "Assuming that those who would fly are relatively safe drivers, an estimate of the risk tied to U.S. auto deaths per billion miles driven in 2018 would be about one in three million. That is lower than the COVID-related death risk associated with a 1,000 mile flight, which I estimate as 1 death per 600,000 passengers if the plane is 2/3 full. The huge safety advantage of flying 1,000 miles nonstop rather than driving, pre-COVID, has disappeared as of August 2020.”
USC’s Hendel agrees. “If you have to—and can afford it—I think traveling by car is the safest option right now, in part because you’re not traveling with another person whose risk of infection may be unknown," he says. "Essentially you aren’t sharing the breathing space with someone who could be infected. But of course, one needs to be very cautious about stopping while traveling by car. I think train travel might possibly have an edge over air travel. Regardless, everyone should be wearing a mask on the train or in the plane.”
And Dr. Karl Neumann, a pediatric travel expert and founder of the site KidsTravelDoc.com is blunt in assessing the risks for children. “Amtrak is better than air travel, but car travel is much better than airlines and trains,” he says. “The most important [protections] are proper spacing and masks.”
Other tips to consider
- If you’re traveling on any form of public transportation, the earliest departures of the day are best, since airplanes, trains, and buses are more likely to be heavily disinfected overnight.
- Carry extra masks/face coverings, gloves, disinfectant wipes, and hand sanitizer (with at least 60 percent alcohol).
- On an airplane or train, wipe down your immediate area, including armrests, seat backs, tray tables, seatbelts, air vents, window shades, light controls, etc.
- In a rental car, wipe down “touch points” such as steering wheel, gear shift, door/window/seat handles and controls, seatbelts, mirrors, radio and control knobs, visors, etc.
We're reporting on how COVID-19 impacts travel on a daily basis. Find all of our coronavirus coverage and travel resources here.
By signing up you agree to our User Agreement (including the class action waiver and arbitration provisions ), our Privacy Policy & Cookie Statement and to receive marketing and account-related emails from Traveller. You can unsubscribe at any time. This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Travel-Acquired Illnesses Associated with Fever
The evaluation of fever in travelers poses a diagnostic challenge to clinicians for many reasons. First, there are many possible etiologies, some of which are geographically localized and are, thus, unfamiliar ( Table 20.1 ). Diagnosis may be delayed owing to lack of familiarity with routes of infection or clinical presentations of these geographically limited illnesses. Fever in travelers may be caused by infections that are potentially fatal if not recognized and treated expediently, the most common of which is malaria ( Table 20.2 ). Furthermore, some infectious diseases that cause fever in travelers are highly communicable ( Table 20.3 ). These infections represent a considerable public health danger, and some have been associated with fatal nosocomial transmission. However, most febrile illnesses in travelers are self-limited and remain unconfirmed microbiologically, such as viral upper respiratory infections and gastrointestinal infections. Thus the challenge facing the clinician in the evaluation of fever in travelers is the detection of serious treatable or communicable infections while not submitting the majority of travelers with benign, self-limited causes of fever to expensive or invasive diagnostic evaluations. To succeed, the clinician must know as much as possible about the epidemiology, distribution, mode of transmission, and clinical characteristics of the etiologies of fever in travelers.
Relative Risk of Travelers Contracting Infectious Diseases in Developing Countries
HIV , Human immunodeficiency virus.
Selected Potentially Fatal Febrile Tropical Infections with Established Treatments
TMP/SMX , Trimethoprim/sulfamethoxazole.
Selected Tropical Diseases with Documented Potential for Nosocomial Transmission
MERS-CoV , Middle East respiratory syndrome coronavirus; SARS , severe acute respiratory syndrome.
Epidemiology
Studies of fever in travelers have been impaired by the highly mobile nature of travelers and by the fact that travelers seek help abroad or fail to present to physicians at all. Large, prospective surveillance databases such as the GeoSentinel surveillance network and TropNet provide aggregate multinational data on ill travelers returning from destinations around the globe who present for care at designated “sentinel” clinics. In the GeoSentinel analysis by Wilson et al. (2007) , 28% of ill returning travelers reported fever as their chief complaint. A lack of pre-travel counseling was associated with acquisition of a febrile illness abroad, as was visiting friends and/or relatives (VFR) travel. While there was no age bias in fever presentation, male travelers were more likely than female travelers to present with fever.
In retrospective, questionnaire-based studies, the incidence of “high fever over several days” in short-term (<3 weeks) travelers was 1.9%. Of the prolonged fevers reported, 39% occurred only while the traveler was abroad, 37% occurred both abroad and at home, and 24% occurred at home only. Prolonged fever was significantly associated with longer stays (>4 weeks) in the tropics. Among a large cohort of American short-term travelers to the developing world, undifferentiated fever occurred in 3%.
Most causes of febrile illnesses remain undiagnosed in retrospective surveys of travelers. However, in the GeoSentinel analysis by Wilson et al. (2007) , malaria was the most common specific cause of fever in ill returned travelers, accounting for 21% of cases, while acute diarrheal disease and respiratory illness accounted for 15% and 14% of cases, respectively. Dengue, while less common, was still an important cause of fever, occurring in 6% of returned ill travelers; with increasing numbers of outbreaks of dengue in regions popular with tourists over the past 5 years, such as the Caribbean, dengue is becoming increasingly recognized as a specific cause of fever in the returned traveler. Enteric fever and acute hepatitis, both vaccine preventable, were less common, diagnosed in only 2% and 1%, respectively, of febrile returning travelers. Rickettsioses were also rare as a cause of fever, occurring in only 2% of cases. Rates of hospitalization due to post-travel fever range from 20 to 30%, with Plasmodium falciparum malaria being the most likely specific cause of hospitalization in this setting.
In general, high-risk areas for the acquisition of febrile illnesses include sub-Saharan Africa, Southeast Asia, and Latin America. Sub-Saharan Africa and Oceania are “hot spots” for malaria acquisition, whereas South Central Asia contributes many cases of travel-acquired enteric fever (i.e., typhoid fever and paratyphoid fever due to Salmonella enterica serotypes Typhi and Paratyphi, respectively). Travelers returning with rickettsial infections have traveled almost exclusively to sub-Saharan Africa, while dengue infections are most commonly acquired in Southeast Asia, Latin America, and, increasingly, the Caribbean. With the emergence of chikungunya in the Americas in late 2013, and Zika in late 2015, these viral infections remain on the differential diagnosis of fever in travelers returning from all parts of the Caribbean, and Central and South America, as well as areas of prior endemicity, such as the Indian Ocean islands.
Medical History
The medical history, including pre-travel preparation and the details of activities and exposures during travel, is essential in identifying the differential diagnosis of fever in travelers.
Vaccinations and Prophylaxis
First, always establish the patient's vaccination status. No vaccination is 100% effective; efficacy ranges from the near-perfect, 10-year protection provided by yellow fever vaccine to the approximately 65% efficacy of both the injectable and oral typhoid vaccines. The efficacy of the current hepatitis A and hepatitis B vaccine series is >90%. When a dose of oral polio vaccine is repeated in adult life, as recommended for risk of exposure, vaccine efficacy approaches 90-100%. Thus, a documented history of recent vaccination administered appropriately renders the diagnosis of yellow fever, hepatitis A, hepatitis B, or polio unlikely, while illnesses with poorer vaccine efficacy, such as typhoid fever and influenza, remain more probable. Similarly, administration of immune globulin within 3 months of exposure makes hepatitis A highly unlikely.
A history of compliance with prophylaxis for malaria or traveler's diarrhea is helpful, although one should bear in mind that prophylaxis for malaria is not 100% effective (see Chapters 6 and 21). It is also important to inquire as to previous diagnostic tests and treatment, some of which may have occurred while traveling.
It is important to learn the details of itinerary, duration, and style of travel, as well as the particular characteristics of a given trip, to ascertain the risk of serious disease presenting as fever. The travel itinerary is important because many diseases are limited in their geographic distribution (see TABLE 20.6 , TABLE 20.8 , TABLE 20.10 , TABLE 20.11 , TABLE 20.12 ). In addition to geographic exposure, there may be a significant association between length of travel and serious illness, and infections vary significantly between short-term travelers and immigrants exposed to similar conditions in the same geographic area.
Important Tropical Infections Associated with Spontaneous Bleeding
Important Tropical Infections Causing Meningitis and Encephalitis
TABLE 20.10
Epidemiology of Important Arboviruses a
TABLE 20.11
Epidemiology and Clinical Characteristics of Viral Hemorrhagic Fevers
DIC , Disseminated intravascular coagulopathy.
TABLE 20.12
Epidemiology of Rickettsial Diseases
For example, schistosomiasis may present as Katayama fever (acute schistosomiasis) among travelers, but this syndrome is rarely observed in individuals born and raised in endemic areas, who may present as immigrants with symptoms of chronic schistosomiasis, such as abdominal discomfort, ascites, and splenomegaly (Chapter 48). Age at time of exposure, underlying health, genetic factors, and intensity and duration of parasite exposure probably contribute to these differences.
Travel style can be associated with an increased risk of serious illness, especially if an individual resided with locals or participated in an “adventure tour” as opposed to staying in urban, first-class hotels. Travel on cruise ships is a notorious risk factor for norovirus infection and invasive bacterial gastroenteritis. Younger age and being a student also increase the risk of becoming ill while traveling.
Exposures are clues that can narrow the differential diagnosis ( Table 20.4 ). It is important to inquire specifically about arthropod bites, animal contact, sexual behavior, blood- and body-fluid exposures from injections or transfusions of blood products, caring for ill individuals (see Table 20.3 ), and ingestion of unpurified water, unpeeled raw fruits, raw vegetables, raw or undercooked meat/seafood, or unpasteurized dairy products. One should inquire about bathing or swimming in fresh water in areas where schistosomiasis or leptospirosis are prevalent. Barefoot exposure to sand or soil establishes risk for geohelminth infections such as strongyloidiasis and hookworm infection. Travelers may be reluctant to volunteer information regarding sexual contact abroad, but a complete sexual history is always warranted.
Exposures Suggesting Specific Infections
HIV , Human immunodeficiency disease; HTLV-1 , human T-cell lymphotropic virus type 1; PID , pelvic inflammatory disease.
Patients such as volunteers, missionaries, long-term expatriates, and military personnel may present with diseases seen in both travelers and immigrants, presumably reflecting more intense and prolonged exposures.
Clinical Characteristics
Incubation period.
It is important to establish the onset of fever in relation to exposures, because the incubation period of illness can narrow the diagnostic possibilities. Some infections may present long after exposure, such as amebic liver abscess, malaria (especially if due to Plasmodium vivax , P. ovale , or P. malariae ), human immunodeficiency virus (HIV), brucellosis, hepatitis B, tuberculosis, visceral leishmaniasis, and human African trypanosomiasis. It is also helpful to note whether the course of illness has been acute or chronic. Table 20.5 is helpful as a guide, but many of the chronic illnesses listed, such as American and African trypanosomiasis, may also present as acute febrile syndromes during primary infection.
Selected Febrile Illnesses of Travelers Classified by Incubation Period and Typical Clinical Course
Interval to presentation can serve as a proxy for incubation period. Falciparum malaria is most likely to present in the 7- to 14-day post-travel window, whereas malaria due to P. vivax may present beyond 42 days post-travel. Dengue seldom presents beyond 10 days post-travel, and chikungunya and rickettsioses rarely beyond 12 days. Similarly, fever due to common agents of traveler's diarrhea or influenza rarely present beyond 1 week post-travel.
Fever Patterns
Fever patterns, although potentially helpful, may not be as characteristic of certain diseases in short-term travelers as they are in immigrants. Fevers of primary malaria rarely exhibit the intermittent pattern of tertian or quartan fevers (every 2 or 3 days, respectively) characteristically experienced by partially immune individuals. “Saddle-back fever,” which refers to the phenomenon in which fever lysis is followed within several days by the resumption of high fevers, is found in 60% of cases of dengue fever but can also be seen in relapsing fever resulting from Borrelia species or with P. malariae (quartan malaria) infection, leptospirosis, and many arboviral infections other than dengue. Continuous fever with temperature/pulse dissociation (relative bradycardia) is often present in enteric (typhoid or paratyphoid) fever, tick typhus, and arboviral infections. Remittent fevers, in which the body temperature fluctuates more than 2° C (3.6° F) but does not completely return to normal, can occur in pulmonary tuberculosis but may also be seen with bacterial sepsis and bacterial abscesses.
Specific Symptoms
Specific symptoms may help establish a diagnosis. Severe myalgia and arthralgia, although characteristic of many febrile illnesses, are extremely severe in arboviral infections such as chikungunya and dengue. Chills are especially prominent in malaria, bacterial infections or sepsis, and dengue. Spontaneous bleeding suggests the possibility of infection with one of the hemorrhagic viruses (e.g., Lassa fever, yellow fever, dengue hemorrhagic fever) but is also reported with various bacterial and rickettsial diseases ( Table 20.6 ). Bleeding may range from easy bruising typical of mild dengue to severe epistaxis, gastrointestinal bleeding, and possible spontaneous central nervous system hemorrhage seen with severe hemorrhagic viral diseases.
Diarrhea associated with fever is typically caused by common bacterial agents of traveler's diarrhea such as Campylobacter species, enterohemorrhagic, enteroaggregative, and enteroinvasive Escherichia coli strains, Salmonella species, Shigella species, Entamoeba histolytica , and intestinal viruses. Occasionally, febrile diarrhea may present due to other gastrointestinal pathogens such as hookworm, coccidia such as Cyclospora cayetanensis or Cryptosporidium , and rarely with Giardia lamblia . However, many systemic illnesses can present with diarrhea, including malaria.
Respiratory symptoms that suggest viral upper respiratory infections may be manifestations of tuberculosis, bacterial pneumonia, Q fever, melioidosis, or the pulmonary migration phase of helminths such as Ascaris lumbricoides and Strongyloides stercoralis. Fever with localized respiratory signs and symptoms in a traveler to South Central or Southeast Asia should raise the specter of highly pathogenic avian influenza or severe acute respiratory syndrome (SARS). Middle East respiratory syndrome coronavirus should be considered when evaluating fever, respiratory symptoms, and recent travel to the Middle East or Korea.
Hepatosplenomegaly along with fever suggests malaria, mononucleosis, hepatic amebiasis, acute schistosomiasis (Katayama fever), visceral leishmaniasis, or enteric fever, among other infectious diseases. Lymphadenopathy evokes mononucleosis, HIV, acute schistosomiasis, plague, typhoid fever, tularemia, and trypanosomiasis, among others ( Table 20.7 ). Of course, neoplastic and collagen vascular diseases may also induce lymphadenopathy and fever.
Selected Febrile Illnesses Causing Organomegaly and/or Lymphadenopathy
− No association; + Finding is associated; ++ Finding strongly associated; +/− Finding may or may not be present. HIV , Human immunodeficiency virus; HTLV-1 , human T-cell lymphotropic virus type 1.
Meningismus, confusion, and other signs of central nervous system dysfunction may be caused by a variety of viral, parasitic, and bacterial agents ( Table 20.8 ). Many of these pathogens are restricted to certain ecologic niches, so the patient's geographic itinerary, season of travel, and exposure history are essential. For example, Japanese encephalitis virus is limited to the Far East, is a disease of summer in temperate climates, and is transmitted by mosquitoes. Spinal cord disease associated with fever can result from West Nile virus, schistosomiasis, human T-cell lymphotrophic virus type 1 (HTLV-1) infection, or polio virus infection.
Cutaneous manifestations of disease are common but seldom specific ( Table 20.9 ). The erythema chronicum migrans of Lyme disease and rose spots in typhoid fever are examples of unique, specific rashes. Nonetheless, rash can refine a differential diagnosis considerably. For example, an eschar at the site of inoculation is typical of tick typhus, boutonneuse (Mediterranean spotted) fever, and anthrax. Cutaneous ulcers are seen in leishmaniasis, tropical phagedenic ulcer, Buruli ulcer ( Mycobacterium ulcerans ), cutaneous amebiasis, arthropod bites, syphilis, yaws, tuberculosis, and leprosy. When evaluating a patient who has received previous treatment, it is important to recall that rash and fever can be caused by reactions to drugs, such as sulfa drugs, antimalarials, and other antibiotics. Rickettsial diseases are frequently associated with rash, but the absence of rash may be misleading and does not exclude the possibility of rickettsial disease (see Table 20.13 ). Genital ulcers, such as those seen with syphilis, chancroid, and lymphogranuloma venereum, should be construed as markers of exposure to other sexually transmitted diseases that should be excluded in affected travelers, as well.
Selected Infections Characteristically Associated with Fever and Cutaneous Signs
TABLE 20.13
Clinical Features of Important Rickettsial Diseases
Approach to the Traveler with Fever
A thorough but directed evaluation, bearing in mind that most fevers are self-limited, is warranted for the traveler presenting with fever. A careful history covering pre-travel prophylaxis, itinerary, travel style and exposures, apparent incubation period, fever pattern, symptoms, previous treatment, and diagnostic studies is essential. Laboratory tests to consider in the diagnostic evaluation include blood smears for malaria (and Borrelia , trypanosomes, Babesia , etc.), complete blood count and white cell differential, absolute eosinophil count, serum electrolytes, blood urea nitrogen and creatinine, glucose, bilirubin, hepatic transaminases, urinalysis, chest radiograph, tuberculin skin test, hepatitis serologies, and bacterial cultures of blood, urine, and stool. In many instances, it is prudent to obtain and save an acute serum sample for future comparative serologic studies. Suspected cases of viral hemorrhagic fevers, severe malaria, and enteric fever should be immediately hospitalized. Travel in a rural African environment is a significant risk factor for exposure to viral hemorrhagic fevers, although other hemorrhagic viruses, including those causing dengue fever, Hantaan, yellow fever, and Crimean-Congo hemorrhagic fever, have a more cosmopolitan distribution in widely scattered parts of the world ( Table 20.6 ). All cases of suspected viral hemorrhagic fevers should be reported immediately to both the local health department and the Centers for Disease Control and Prevention (CDC).
The clinically stable patient with travel-related fever in whom the initial history, physical examination, and screening laboratory studies, including at least two blood films for malaria separated by >6 but not more than 24 hours, are unremarkable may be observed. The patient should be instructed to keep a temperature record and return in 2-3 days if fever fails to resolve, or sooner if symptoms worsen. Empiric treatment for enteric fever (and/or rickettsioses) may be considered in patients who continue to have fever >48 hours after all diagnostic work-up has been initiated but in whom specific tests have been noncontributory (see Public Health Agency of Canada, Fever in the Returning Traveller 2011 ). Because the majority of travel-related febrile illnesses are self-limited viral syndromes, most fevers will resolve spontaneously. If fever persists, however, repeat malarial smears and blood cultures are warranted. Directed serologic studies to detect diseases compatible with the patient's history and physical examination should be considered. Imaging studies (e.g., abdominal computed tomography or ultrasound) and biopsies (e.g., bone marrow, liver, lymph nodes) may be indicated. Hospitalization may be justified to expedite the work-up in certain circumstances. During the evaluation of perplexing cases of apparent travel-related illness, the clinician should bear in mind that non-infectious disorders, such as pulmonary embolism, occult malignancies, systemic lupus erythematosus, and temporal arteritis, may present with fever.
Presumptive empiric therapy directed against a likely pathogen may be justified, especially when adequate diagnostic studies are not readily available or a patient is clinically deteriorating. Examples include intravenous artesunate for suspected severe infection with P. falciparum , quinolones or third-generation cephalosporins for suspected enteric fever, doxycycline for suspected rickettsioses, and ribavirin for suspected Lassa fever ( Table 20.2 ). Early initiation of appropriate therapy may significantly reduce morbidity and potential mortality from these serious febrile illnesses of travelers.
Infectious Diseases in the Traveler with Fever
Selected infectious diseases that should be considered in the traveler with fever are discussed in this section, with the goal of providing an overview. References to other chapters in this book are given as appropriate; however, the reader is encouraged to consult, when possible, standard textbooks on infectious diseases and tropical medicine and to contact the CDC for current and detailed information on the diagnosis and treatment of exotic diseases. The experts at the CDC can provide 24-hour emergency medical consultation by telephone to healthcare providers dealing with a very ill patient.
Fever in a traveler from a malarious area should be evaluated carefully, with multiple blood smears for malaria. Although malaria is discussed in greater detail in Chapter 21, key points are worth repeating here. P. falciparum infection can be life-threatening when associated with high parasitemia, blackwater fever, cerebral malaria, or acute respiratory distress syndrome. Chemoprophylaxis is often effective, but only when taken as directed. Of the 231 cases of severe malaria in travelers reported to the CDC in 2012, 75% were due to P. falciparum , and 79% of these infections were acquired in sub-Saharan Africa; only 7 of 200 patients in whom information on prophylaxis was known were adherent to their drug regimen. However, drug-resistant P. falciparum is now widespread, and even perfect compliance with prophylaxis does not provide absolute protection from malaria infection. The case-fatality rate for P. falciparum in US travelers was approximately 0.4% in 2012 (6 deaths among 1687 total cases). Clinical manifestations of P. vivax and P. ovale infections can develop up to 5 years after exposure. The diagnosis of malaria in immune individuals or individuals who have received prophylaxis or partial treatment may be complicated by low parasitemia. Multiple blood smears in combination with highly sensitive rapid diagnostic tests or, occasionally, nucleic acid amplification tests such as polymerase chain reaction may be helpful in difficult cases (see also Chapters 6 and 21).
Typhoid and Paratyphoid Fever (Enteric Fevers)
Enteric fever is caused by Salmonella enterica serovar Typhi ( S. typhi ) or Salmonella paratyphi. Persistently rising fever, relative bradycardia, rose spots, and normal leukocyte counts with mild to moderate elevation of hepatic transaminases are all clues to the diagnosis; however, these characteristics are often absent. The organism can be cultured from the blood in >80% of patients during the first week of illness and from bone marrow aspirated from the iliac crest in more than 90% of documented cases, if no antibiotics are administered before obtaining the culture. The organism can be cultured from stool during the incubation period occasionally, and in one-third to two-thirds of patients during the second through fourth weeks of illness.
Neither the oral nor the parenteral vaccine provides complete immunity (Chapter 5). In immunized populations, however, a higher percentage of individuals with enteric fever will have disease caused by S. paratyphi , although disease caused by S. typhi still occurs. Of the approximate 5700 cases of typhoid fever that occur annually in the United States, up to 75% are travel acquired. Of the 1902 laboratory-confirmed cases of typhoid fever reported by Lynch and colleagues (2009) between 1999 and 2006 in the United States where epidemiologic information was available, foreign travel in the preceding 30 days was reported by 79%, yet only 5% had received typhoid vaccine prior to travel. Seventy-three percent of cases were hospitalized, and 0.2% died. Resistance to antimicrobials has been reported for S. typhi isolates in many countries, although fluoroquinolones are usually effective against typhoid fever acquired outside the Indian sub-continent and Southeast Asia (Chapter 31).
Arboviral Diseases
Arboviral diseases are caused by arthropod-borne viruses; most are zoonoses (shared between humans and other vertebrate hosts). More than 400 arboviruses, classified into many families and genera, have been described ( Table 20.10 ). Arboviral diseases are present throughout the tropics; however, some arboviruses, such as o'nyong-nyong, Mayaro, Ross River, Oropouche, and Rift Valley fever viruses, are limited in geographic distribution. Diagnosis usually depends on clinical suspicion and serologic confirmation, the latter generally requiring acute and convalescent serum samples.
The arboviral diseases can be divided into four syndromes based on clinical presentation: (1) undifferentiated fever, (2) dengue fever, (3) hemorrhagic fever, and (4) encephalitis. The syndrome of undifferentiated fever (e.g., Oropouche, Mayaro, and sand fly fever) is generally characterized by one or more of the following: fever, headache, myalgia, pharyngitis, coryza, nausea, vomiting, and diarrhea. The dengue fever syndrome (dengue, chikungunya, o'nyong-nyong, Sindbis, West Nile, Ross River viruses) is characterized by fever, rash, arthralgia, and leukopenia. The syndrome of hemorrhagic fevers (Lassa fever, Ebola, Marburg, Crimean-Congo, Argentine, Bolivian, dengue, yellow fever viruses) ranges from mild petechiae to severe purpura and bleeding diathesis. The 2014 West African outbreak of Ebola virus disease (EVD) underscores that prior estimates of the frequency of hemorrhagic manifestations in EVD are likely inflated. In this outbreak of EVD, which has led to >27,000 cases and >11,000 deaths, bleeding and hemorrhagic manifestations have been noted to occur in 5-15% of patients ( Chertow et al. 2014 ; Qin et al. 2015 ).
Dengue Fever
Dengue is the most widespread arbovirus, distributed throughout the tropics, and frequently encountered in travelers returning from the tropics. Dengue virus is a single-stranded RNA flavivirus transmitted by the day-biting urban mosquito Aedes aegypti or the jungle mosquito Aedes albopictus. Four serotypes are recognized. Infection with one serotype results in immunity to that particular serotype; however, after a short period of cross-protection, individuals are susceptible to infection with another serotype.
Clinical infection ranges from a mild febrile syndrome to a severe dengue syndrome. Individuals with dengue who recover fully following defervescence are considered to have uncomplicated dengue, while those who deteriorate clinically are classified as having “warning signs,” which include any of the following manifestations: abdominal pain, persistent vomiting, fluid accumulation, mucosal bleeding, lethargy, hepatic enlargement, and worsening thrombocytopenia in the setting of hemoconcentration. A minority of patients with warning signs will continue to deteriorate despite fluid resuscitation, and those are considered to have severe dengue, characterized by severe plasma leakage, severe bleeding, or organ failure ( WHO 2009 ).
The incubation period of dengue is 5-8 days. A viral prodrome of nausea and vomiting is common, followed by high fever for a mean of 5 days; the fever often lyses abruptly. Myalgia and arthralgia are particularly prominent, giving rise to the common name of “breakbone fever.” Headache (especially retro-orbital), lymphadenopathy (frequently cervical), and/or rash (scarlatiniform, maculopapular, or petechial; characteristic “islands of white macules on a sea of red”) frequently develop. The rash may occur late during the course of illness, and fever may reappear after several days. ( Note : this “saddleback” fever pattern is present in about 60% of cases.)
Chikungunya
Chikungunya virus infection has been historically noted among travelers from Southeast Asia and Africa. However, in late 2013, the virus emerged for the first time in the Americas, leading to a widespread and ongoing outbreak in the Caribbean and Central and South America affecting at least 44 individual countries, with cases numbering into the hundreds of thousands. This has resulted in high numbers of cases among North American and European travelers to the Caribbean and Central America, in particular. This disease presents in a fashion similar to dengue fever, although incubation and duration of symptoms are typically more prolonged. Myalgia and arthralgia are particularly severe with chikungunya, with function-limiting arthropathy persisting for years in a minority of patients.
Zika virus was discovered in Uganda in 1947, and human infectinos were extraordinarily rare until 2015, when an epidemic began to sweep across South and Central America. Most adult patients have a clinical illness very similar to Dengue and Chikungunya, although neurological injury such as Guillan-Barre has been described. Of greatest concern is its association with microcephaly if the patient is pregnant during infection. Women who return from endemic areas with fever should be assessed for this infection, and if infected and pregnant, counseled on strategies for aggressive fetal monitoring or termination options.
Yellow Fever
In the Americas, yellow fever is transmitted by Haemagogus mosquitoes in the jungle environment and A. aegypti in urban settings. In Africa, transmission to humans occurs via Aedes spp. Historically, in both urban and rural environments, only 50-200 cases of yellow fever per year have been reported from the tropical Americas. However, yellow fever is an emerging problem in the Amazon and other jungle regions of Brazil, Colombia, Venezuela, and Peru, with resurgence of the disease in the early 2000s leading to mass vaccination initiatives. Sporadic urban transmission still occurs in large outbreaks in Africa. Although A. aegypti is ubiquitous in the Far East, yellow fever virus transmission has never been reported from this region. The reason is unclear, but either the lack of virus importation into the region or possible immune cross-resistance induced by endemic dengue immunity may be responsible. The spectrum of clinical disease ranges from a dengue fever-like illness to a severe hemorrhagic illness associated with hepatic and renal failure. The disease is almost 100% preventable by vaccination with live attenuated 17D-strain vaccine (Chapter 5). Among unvaccinated travelers from the United States and Europe, nine cases of yellow fever occurred between 1970 and 2011, five of which were acquired in sub-Saharan Africa, and four in South America. Eight of these cases were fatal.
Hemorrhagic Syndromes
Viruses causing hemorrhagic syndromes, such as Lassa fever virus, Ebola virus, Marburg virus, and Machupo virus, have been associated with life-threatening infections that can be spread nosocomially. Patients who are suspected of having one of these viruses should be placed in airborne and contact isolation. Laboratory work should be kept to a necessary minimum and the laboratory alerted to the possibility of contagious virus in patient specimens. The CDC and state health department should be contacted immediately.
An arthropod vector has not been identified for many of these viruses, such as Lassa fever, which is transmitted via contact with rodent reservoirs in rural West Africa or with infected humans. Early symptoms include fever, malaise, weakness, and myalgia. A few days later, cough, pharyngitis, and chest and epigastric pain develop. Vomiting and diarrhea occur by about day 5, associated with fever of 39-40° C. By the sixth day, respiratory distress, cardiac instability, hepatic and renal failure, and hemorrhagic phenomena begin to appear. Lassa fever can be diagnosed by either the isolation of virus or the demonstration of a four-fold increase in antibody titer. Early treatment with ribavirin may improve outcome with Lassa fever virus, Hantaan virus, and other hemorrhagic viruses with the exception of Ebola, yellow fever, and dengue viruses. Other viruses of importance are listed in Table 20.11 . (See also Chapter 28.)
Rickettsial Diseases
Rickettsial diseases are acute, usually self-limited febrile illnesses caused by obligate intracellular Gram-negative bacteria of the order Rickettsiales. Rickettsiae can be divided into the spotted fever group and the typhus fever group. All are transmitted by ticks, fleas, lice, or mites. Rickettsiae are widely distributed throughout the world ( Table 20.12 ).
The spectrum of illness ranges widely and includes subclinical infection. Incubation periods for the various diseases vary widely, on the order of 2-30 days ( Table 20.13 ). Clinical illness is generally characterized by an abrupt onset of fever, chills, and sweats, frequently associated with rash, headache, conjunctivitis, pharyngitis, epistaxis, myalgias, arthralgias, and hepatosplenomegaly. An eschar often develops at the site of the bite of the mite or tick in scrub typhus, due to Orientia tsutsugamushi , and the spotted fever group rickettsioses. Vasculitis underlies the typical pathologic manifestations of rickettsial disease. Complications are rare but include encephalitis, renal failure, and shock.
Most rickettsial disease reported in the United States is acquired domestically (e.g., Rocky Mountain spotted fever). Spotted fever group rickettsioses, including Mediterranean spotted fever/boutonneuse fever and African tick bite fever, appear to be the most common rickettsial diseases of travelers, accounting for 231 of 280 cases of rickettsial disease among travelers reported by GeoSentinel between 1996 and 2008 ( Jensenius et al. 2009 ). Typhus fever group rickettsioses are endemic to areas in southern Europe, Africa, and the Middle East, although most cases are also reported in travelers to Africa.
Diagnosis requires clinical suspicion (often mandating empiric antibiotic therapy) and specific serologies. Therapy consists of doxycycline (200 mg/day in divided doses) generally for 3-4 days after defervescence and a minimum of 1 week total therapy. Recent evidence suggests that short courses of macrolide antibiotics, such as azithromycin or clarithromycin, may be acceptable alternatives for the therapy of rickettsioses other than Rocky Mountain spotted fever.
Schistosomiasis (Bilharziasis)
Schistosomiasis is caused by a fluke and transmitted by freshwater exposure in endemic regions. Katayama fever, or acute schistosomiasis, develops 2-10 weeks after exposure. This serum sickness-like illness is believed to represent a reaction against antigen–antibody complexes formed as a result of egg deposition. This syndrome is most severe in Schistosoma japonicum infections, in which egg production is greatest. Characteristic clinical manifestations include fevers, chills, sweating, headache, cough, lymphadenopathy, hepatosplenomegaly, and eosinophilia. Although death has been reported in S. japonicum infections, most patients with Katayama fever experience a self-limited illness that is commonly undiagnosed. Travelers appear to be more likely to develop this syndrome than those raised in endemic areas. Serologic studies are helpful in the diagnosis. Recommended treatment involves administration of praziquantel and corticosteroids (see Chapter 48). Mounting evidence suggests that asymptomatic travelers returning from high-risk areas should be screened (serologically and/or with stool/urine ova and parasites, the latter >6 weeks after exposure) and treated.
The filariasis syndromes associated with fever include onchocerciasis (river blindness), lymphatic filariasis (lymphangitis, often complicated by bacterial superinfection), loiasis, and nocturnal fever with or without pulmonary symptoms resulting from circulating microfilariae. Of these entities, loiasis is most commonly seen in travelers and short-term residents of risk areas (rainforest regions of Central Africa). Eosinophilia is common in patients with filariasis. The diagnosis is usually established by the demonstration of microfilariae in skin snips (onchocerciasis) or in blood. ( Note : in lymphatic filariasis, the microfilariae circulate nocturnally, while microfilaremia of Loa loa peaks in the late afternoon.) Serologic study may be helpful when the disease is suspected (see Chapter 47).
Strongyloidiasis
Strongyloidiasis, usually acquired when larvae in contaminated soil penetrate the skin, rarely causes a febrile illness in travelers. However, a Löffler syndrome, characterized by pulmonary infiltrates with eosinophilia, may occur during the obligate lung migration phase of larvae and may be accompanied by fever. Immunocompromised hosts, particularly due to HTLV-1 or corticosteroids, can develop a life-threatening hyperinfection syndrome, which is frequently complicated by significant disseminated strongyloidiasis outside the gastrointestinal tract (see Chapter 45).
Trichinosis
Trichinosis, usually associated with high-grade eosinophilia, muscle pain, and fever, can be acquired by travelers who ingest undercooked meat (see Chapter 49).
Paragonimiasis
Paragonimiasis is an illness caused by a lung fluke that induces a febrile response either during its migration to the lungs or by its obstruction or destruction of lung parenchyma. Hemoptysis can occur, mimicking pulmonary tuberculosis. The disease is usually acquired by ingestion of raw freshwater crustaceans in Asia, South America, and Africa, though case series are reported in the United States from imported freshwater crab or local crawfish ingestion. Diagnosis can be established by examination of the sputum and stool for ova. Serologic studies are available (see Chapter 48).
Echinococcosis
The ingestion of food or water contaminated by echinococcal eggs from canid feces can cause hydatid cyst disease involving the lungs or liver. Fever is usually absent unless the cyst or cysts become secondarily infected or rupture (see Chapter 46).
E. histolytica is usually acquired by ingesting cysts in water or food contaminated by human feces but may be transmitted sexually. Both amebic dysentery and amebic liver abscess may cause fever. Amebic liver abscess is associated with right upper quadrant discomfort, hepatomegaly, an elevated right hemidiaphragm, and high serologic reactivity to E. histolytica antigens. Often, E. histolytica cannot be identified in the stool at the time of presentation of amebic abscess. Treatment is with metronidazole plus another agent to clear luminal cysts, such as iodoquinol (see Chapter 32).
Chagas Disease
Chagas disease (American trypanosomiasis), caused by infection with Trypanosoma cruzi , is typically acquired by dwelling in mud or thatched-roof housing, via the feces of the reduviid bug, which defecates on the patient during a silent blood meal. In addition, transmission in Latin America is often congenital or via blood transfusion in endemic countries and occasionally in the United States. It is increasingly recognized as a food-borne illness when cane-sweetened juices are contaminated by crushed reduviid bugs. In typical transmission, after an incubation period of 1-2 weeks, T. cruzi causes a febrile illness during the acute stage of infection that persists for 2-4 weeks. The illness is accompanied by local swelling at the site of inoculation of trypanosomes (Romaña sign), lymphadenopathy, hepatosplenomegaly, and influenza-like symptoms. Trypanosomes may be seen during the acute stage of infection in peripheral blood by blood smear or in biopsy specimens obtained from the site of inoculation. Serology studies may be helpful. Treatment during the acute stage of infection with benznidazole or nifurtimox is beneficial in attenuating the progression to chronic Chagas disease. This disease is rare among travelers but is increasingly recognized in non-endemic countries among Latin American immigrants (see Chapter 26).
African Trypanosomiasis
African trypanosomiasis (infection with Trypanosoma brucei gambiense or T. brucei rhodesiense ) cause febrile syndromes due to circulating trypanosomes. West African disease often presents in a subacute or chronic fashion, whereas East African disease is less well adapted to humans and thus has a more fulminant course. Both diseases are transmitted by the bite of the tsetse fly in Africa. Occasionally, a chancre can be seen at the site of inoculation during acute infection. Lymphadenopathy is common, particularly in the posterior cervical chain. Later, the trypanosomes invade the central nervous system, and lumbar puncture must be performed to determine which treatment regimen should be administered. If disease has progressed to the central nervous system, treatment with arsenicals, such as melarsoprol, or difluoromethylornithine is recommended for East and West African trypanosomiasis, respectively. African trypanosomiasis is uncommon among travelers, although clusters have been reported, mainly in travelers returning from East Africa. Both East and West African disease are ultimately fatal without treatment, so recognition and rapid action is essential (see Chapter 27).
Visceral Leishmaniasis
Visceral leishmaniasis, or kala-azar, is characterized by hepatosplenomegaly, severe wasting, and fevers, a syndrome evocative of lymphoma. Leishmania spp. are transmitted by the bite of the sand fly. The kala-azar syndrome is usually caused by Leishmania donovani. Visceral leishmaniasis is extremely uncommon among travelers. Treatment is with amphotericin B in lipid formulations, pentavalent antimonials, or miltefosine (see Chapter 39).
Toxoplasmosis
Toxoplasmosis, which can cause an acute febrile syndrome, may be acquired by travelers via the consumption of undercooked meat. Transmission may occur in unexpected places, such as France, where infection with Toxoplasma gondii is much more common because of the popular ingestion of uncooked meat.
Tuberculosis
Tuberculosis is an uncommon disease among short-term travelers ( Table 20.1 ). Travelers at increased risk are those going abroad to perform medical service and those residing abroad for prolonged lengths of time. Occasionally, tuberculosis transmission has been reported among air travelers as the result of relatively poor air turnover on airlines and the presence of a passenger with active pulmonary tuberculosis. In a study of American healthcare workers returning from Botswana, tuberculin skin test conversion occurred in 4.2%, corresponding to a rate of 6.87 per 1000 person-weeks of travel ( Szep et al. 2014 ). Healthcare workers, missionaries, teachers, and others who anticipate close daily contact with resident populations in countries where the incidence of tuberculosis is high should receive the tuberculin skin test before travel to establish a baseline status, and 8-12 weeks following travel (see Chapter 25).
Meningococcal Meningitis
Meningococcal infection occurs sporadically in travelers to endemic areas (sub-Saharan Africa and Nepal) and in epidemics during times of crowding. An example of the latter is the reported high incidence of meningococcal disease and carriage after pilgrimage to Mecca. Purpuric lesions and signs of meningismus are helpful diagnostic clues, but individuals may present with only fever and respiratory symptoms. Diagnosis is established by culture of blood and cerebrospinal fluid, and treatment with parenteral ceftriaxone is usually effective. Close contacts of documented cases should receive prophylaxis with rifampin or ciprofloxacin. Travelers going to areas of known meningococcal transmission should undergo meningococcal vaccination before departure (see Chapter 5).
Leptospirosis
Leptospirosis is acquired by contact with water contaminated by animal urine containing spirochetes. It is common in the tropics and subtropics (Chapter 23). This disease may be contracted by abattoir workers, swimmers, and campers. Large outbreaks have occurred among triathletes in Illinois (98 cases) and competitive swimmers in Borneo (70 cases). Clinical illness ranges from relatively mild disease to fulminant hepatic failure with icterohemorrhagic fever (Weil's disease). Definitive diagnosis is based on either serologic studies or the demonstration of leptospires in specimens of clinical fluids. As with rickettsioses, empiric treatment is often considered.
Brucellosis
Brucellosis is usually transmitted by unpasteurized dairy products but may be encountered in abattoirs. Illness ranges from an indolent febrile syndrome to fulminant endocarditis. Brucellosis is occasionally encountered in the post-travel setting, although laboratory acquisition is well documented and remains a risk for medical and laboratory workers who volunteer or work overseas. In their study of >42,000 ill returned travelers entered into the GeoSentinel database between 2007 and 2011, Leder and colleagues (2013) reported 33 cases of acute brucellosis, most of which were acquired in India, the Sudan, and Iraq.
Plague is reported to be epidemic in humans in certain regions of Vietnam and is endemic in rodent populations in the southwestern United States and other areas of the world. Larger outbreaks can occur, as in India in 1994. Plague causes a clinical syndrome of painful regional lymphadenitis associated with necrotizing pneumonia and septicemia. Prophylactic doxycycline may be given to travelers at risk, since the plague vaccine is not widely available (see Chapter 5).
Melioidosis
Melioidosis, caused by the Gram-negative bacterium Burkholderia pseudomallei , produces a tuberculosis-like illness or septicemia. The disease is particularly prevalent in Southeast Asia, where it is especially common in rice-paddy workers. Many Vietnam veterans have serologic evidence of past infection with B. pseudomallei. Like tuberculosis, the bacteria may remain dormant for many years before reactivating and causing illness.
Relapsing Fever
Relapsing fever (caused by Borrelia species) is a worldwide tick-borne endemic disease, but louse-borne human–human transmission still occurs in highlands of Ethiopia, Sudan, Somalia, Chad, Bolivia, and Peru. Diagnosis depends on the demonstration of extracellular spirochetes by blood smear and Giemsa staining.
Bartonellosis (Oroya Fever)
Bartonellosis, caused by Bartonella bacilliformis , is transmitted by sand flies only in Andean river valleys with elevations between 2000 and 8000 ft in Peru, Ecuador, and Colombia. This infection can lead to acute hemolysis (i.e., Oroya fever), in which intraerythrocytic organisms may be detected on pathologic stains (e.g., Giemsa) or in chronic, angioproliferative skin lesions (i.e., verruga peruana, lesions that may be sessile, miliary, nodular, pedunculated, or confluent and may be as large as 1-2 cm). A newly described species, Bartonella rochalimae , was reported to cause an Oroya fever-like illness, characterized by anemia, fever, and splenomegaly, in an American traveler to Peru ( Eremeeva et al. 2007 ). The patient had been traveling in an area endemic for B. bacilliformis , but to date, no clear vector has been identified. This case highlights the sustained possibility of discovering novel pathogens as international travel becomes increasingly attractive and affordable.
Cutaneous anthrax generally has been associated with exposure to infected animals, contaminated animal hides, and wool. Because Bacillus anthracis spores can survive for prolonged periods, contaminated hides or wool remain infectious and may rarely be responsible for disease transmission. Anthrax is sometimes associated with a local eschar, where bacteria proliferate and invade the bloodstream. Travelers purchasing souvenirs or articles of clothing made with contaminated animal hides or wool are a group at theoretical risk for the acquisition of anthrax; hunters are another potential group at risk. In contrast, inhalational anthrax is usually thought to be associated with bioterrorism.
Sexually Transmitted Infections
Gonorrhea, syphilis, chlamydia, lymphogranuloma venereum, herpes simplex virus, HIV, granuloma inguinale, and chancroid are all sexually transmitted diseases that may give rise to fevers (see Chapters 41-44Chapter 41Chapter 42Chapter 43Chapter 44).
Respiratory and Enteric Viruses
Common respiratory and enteric viruses are the most common causes of fever in travelers, accounting for over 50% of cases of febrile illness in travelers in most case series.
Hepatitis viruses are a relatively common cause of fever in travelers (100-200/100,000 travelers); prodromal symptoms associated with fever may precede icterus. Hepatitis A occurs most frequently, but >90% of cases could be prevented by pre-travel immunization with hepatitis A vaccine. Adults over the age of 40 years who acquire hepatitis A are at much greater risk of having a complicated course or dying of their disease than are those who are younger. Hepatitis B and C may occur in healthcare workers, individuals with a history of sexual contact abroad, and patients who receive blood transfusions, although the hepatitis B immunization is also highly effective (see Chapter 22). Hepatitis E has been serologically confirmed in many returned travelers; it undoubtedly occurs more often. In long-term travelers to the developing world, the seroconversion rate for hepatitis E is ~5%.
Human Immunodeficiency Virus (HIV)
Acute HIV infection, resulting from sexual activity, blood transfusion, and intravenous drug use, has been reported among returned travelers (see Chapter 41). In their analysis of GeoSentinel data, Leder and colleagues (2013) reported 84 cases of acute HIV among >42,000 ill returned travelers, making HIV the seventh most common specific cause of fever in this group. Rash and lymphadenopathy combined with appropriate history can be clues to suspect primary infection. Plasma RNA levels are more sensitive than serodiagnostic tests, which may be negative in the early period of infection.
Infectious Mononucleosis
Acute infection with Epstein-Barr virus (EBV) may occur in susceptible travelers, especially in the 15- to 30-year-old age group. Hepatosplenomegaly, lymphadenopathy, mucopurulent pharyngitis, heterophile antibodies, and the presence of atypical lymphocytes on the blood smear are helpful clues. Specific EBV serologies are useful to establish the diagnosis of acute infection. Cytomegalovirus (CMV) infections may cause an infectious mononucleosis-like illness with elevated hepatic transaminases in travelers and may be diagnosed by CMV serologies.
Rubeola (measles) remains an important cause of morbidity and mortality in developing countries and poses a substantial risk to travelers who have not received adequate immunization. Furthermore, the syndrome of atypical measles may result from exposure to wild virus in individuals who may have received killed virus vaccine (used in the United States before 1963). A large outbreak involving a US theme park in 2014 underscored the risk of measles to unvaccinated individuals and the risk of exported disease via commercial air travel. Complications of measles include progressive pneumonitis (especially in pregnant or immunocompromised patients), pulmonary bacterial superinfection, and encephalitis.
Endemic mycoses such as histoplasmosis and coccidioidomycosis are becoming increasingly recognized among international travelers and can present as undifferentiated fever. Among 13 cases of acute pulmonary histoplasmosis in a group of US travelers to Martinique, trekking through a mountain tunnel full of bats emerged as the common epidemiologic risk factor. Participation in construction projects at an orphanage in Tecate, Mexico was similarly associated with a cluster of cases of coccidioidomycosis among US travelers. Penicilliosis can also be acquired by travelers. Endemic mycoses can present as a systemic febrile or flu-like illness, with or without accompanying respiratory, cutaneous, or articular manifestations, and should therefore be considered in the differential diagnosis of post-travel fever.
Further Reading
- Abramowicz M. Drugs for parasitic infections. Med. Lett. 2013; 11 (Suppl.):1. (Ed.) [ Google Scholar ]
- Ackers M.L., Puhr N.D., Tauxe R.V. Laboratory-based surveillance of Salmonella serotype Typhi infections in the United States: antimicrobial resistance on the rise. JAMA. 2000; 283 :2668–2673. [ PubMed ] [ Google Scholar ]
- Boggild A., Ghesquiere W., McCarthy A. Fever in the returning international traveller: initial assessment guidelines. Can. Commun. Dis. Rep. 2011; 37 (ACS-3):1–15. http://www.phac-aspc.gc.ca/publicat/ccdr-rmtc/11vol37/acs-3/index-eng.php Available at. accessed July 2, 2015. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bottieau E., Clerinx J., Van den Enden E. Etiology and outcome of fever after a stay in the tropics. Arch. Intern. Med. 2006; 166 :1642. [ PubMed ] [ Google Scholar ]
- Cairns L., Blythe D., Kao A. Outbreak of coccidioidomycosis in Washington state residents returning from Mexico. Clin. Infect. Dis. 2000; 30 :61. [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention Update: outbreak of acute febrile illness among athletes participating in Eco-Challenge-Sabah 2000—Borneo, Malaysia, 2000. MMWR. 2001; 50 :21–24. [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention Summary of notifiable diseases—United States, 2013. MMWR. 2014; 63 (32):702–715. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6332a6.htm Available at. accessed July 2, 2015. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chertow D.S., Kleine C., Edwards J.K. Ebola virus disease in West Africa: clinical manifestations and management. N. Engl. J. Med. 2014; 371 (22):2054–2057. doi: 10.1056/NEJMp1413084. E-pub ahead of print. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- El Bashir H., Coen P.G., Haworth E. Meningococcal W135 carriage; enhanced surveillance amongst east London Muslim pilgrims and their household contacts before and after attending the 2002 Hajj. Travel Med. Infect. Dis. 2004; 2 :13–15. [ PubMed ] [ Google Scholar ]
- Eremeeva M.E., Gerns H.L., Lydy S.L. Bacteremia, fever, and splenomegaly caused by a newly recognized Bartonella species. N. Engl. J. Med. 2007; 356 :2381. [ PubMed ] [ Google Scholar ]
- Freedman D.O., Weld L.H., Kozarsky P.E. Spectrum of disease and relationship to place of exposure in ill returned travelers. N. Engl. J. Med. 2006; 354 :119. [ PubMed ] [ Google Scholar ]
- Hill D.R. Health problems in a large cohort of Americans traveling to developing countries. J. Travel Med. 2000; 7 :259–266. [ PubMed ] [ Google Scholar ]
- Huggins J.W. Prospects for treatment of viral hemorrhagic fevers with ribavirin, a broad-spectrum antiviral drug. Rev. Infect. Dis. 1989; 11 :S750–S761. [ PubMed ] [ Google Scholar ]
- Janisch T., Preiser W., Berger A. Emerging viral pathogens in long-term expatriates (I): hepatitis E virus. Trop. Med. Int. Health. 1997; 2 :885–891. [ PubMed ] [ Google Scholar ]
- Jelinek T., Bisoffi Z., Bonazzi L. Cluster of African trypanosomiasis in travelers to Tanzanian national parks. Emerg. Infect. Dis. 2002; 8 :634–635. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jensenius M., Davis X., von Sonnenburg F., GeoSentinel Surveillance Network Multicenter GeoSentinel analysis of rickettsial diseases in international travelers, 1996-2008. Emerg. Infect. Dis. 2009; 15 (11):1791–1798. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Leder K., Torresi J., Libman M. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Int Med. 2013; 158 :456–468. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Levy M.J., Herrera J.L., DiPalma J.A. Immune globulin and vaccine therapy to prevent hepatitis A infection. Am. J. Med. 1998; 105 :416–423. [ PubMed ] [ Google Scholar ]
- Lewis M.D., Serichantalergs O., Pitarangsi C. Typhoid fever: a massive, single-point source, multidrug resistant outbreak in Nepal. Clin. Infect. Dis. 2005; 40 :554–561. [ PubMed ] [ Google Scholar ]
- Liles W.C., Van Voorhis W.C. Fever in travelers to tropical countries. In: Root R.K., Waldvogel F., Corey L., Stamm W.E., editors. Clinical Infectious Diseases: A Practical Approach. Oxford University Press; New York: 1999. [ Google Scholar ]
- Lynch M.F., Blanton E.M., Bulens S. Typhoid fever in the United States, 1999–2006. JAMA. 2009; 302 (8):859–865. [ PubMed ] [ Google Scholar ]
- Meltzer E., Artom G., Marra E. Schistosomiasis among travelers: new aspects of an old disease. Emerg. Infect. Dis. 2006; 12 :1696–1700. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Morgan J., Bornstein S.L., Karpati A.M. Outbreak of leptospirosis among triathlon participants and community residents in Springfield, Illinois, 1998. Clin. Infect. Dis. 1998; 34 :1593. [ PubMed ] [ Google Scholar ]
- Panackal A.A., Hajjeh R.A., Cetron M.S. Fungal infections among returned travelers. Clin. Infect. Dis. 2002; 35 :1088. [ PubMed ] [ Google Scholar ]
- Public Health Agency of Canada, Committee to Advise on Tropical Medicine and Travel Fever in the Returning International Traveller. 2011. http://www.phac-aspc.gc.ca/publicat/ccdr-rmtc/11vol37/acs-3/index-eng.php Available at. [ PMC free article ] [ PubMed ]
- Qin E., Bi J., Zhao M. Clinical features of patients with Ebola virus disease in Sierra Leone. Clin. Infect. Dis. 2015; 61 :491–495. E-pub ahead of print, May 20. pii: civ319. [ PubMed ] [ Google Scholar ]
- Rigau-Perez J.G., Clark G.G., Gubler D.J. Dengue and haemorrhagic fever. Lancet. 1998; 352 :971. [ PubMed ] [ Google Scholar ]
- Ryan E.T., Wilson M.E., Kain K.C. Illness after international travel. N. Engl. J. Med. 2002; 347 :505. [ PubMed ] [ Google Scholar ]
- Salata R.A., Olds R.G. Infectious diseases in travelers and immigrants. In: Warren K.S., Mahmoud A.A.F., editors. Tropical and Geographic Medicine. second ed. McGraw-Hill; New York: 1990. [ Google Scholar ]
- Salomon J., Flament Saillour M., De Truchis P. An outbreak of acute pulmonary histoplasmosis in members of a trekking trip in Martinique, French West Indies. J. Travel Med. 2003; 10 :87. [ PubMed ] [ Google Scholar ]
- Schwartz E., Shlim D.R., Eaton M. The effect of oral and parenteral typhoid vaccination on the rate of infection with Salmonella typhi and Salmonella paratyphi A among foreigners in Nepal. Arch. Intern. Med. 1990; 150 :349. [ PubMed ] [ Google Scholar ]
- Slom T.J., Cortese M.M., Gerber S.I. An outbreak of eosinophilic meningitis caused by travelers returning from the Caribbean. N. Engl. J. Med. 2002; 346 :668. [ PubMed ] [ Google Scholar ]
- Steffen R., Rickenbach M., Wilhelm U. Health problems after travel to developing countries. J. Infect. Dis. 1987; 156 :84. [ PubMed ] [ Google Scholar ]
- Szep Z., Kim R., Ratcliffe S.J. Tuberculin skin test conversion rate among short-term health care workers returning from Gaborone, Botswana. Travel Med. Infect. Dis. 2014; 12 (4):396–400. [ PubMed ] [ Google Scholar ]
- Wilder-Smith A., Schwartz E. Dengue in travelers. N. Engl. J. Med. 2005; 353 :924. [ PubMed ] [ Google Scholar ]
- Wilson M.E. Oxford University Press; New York: 1991. A World Guide to Infections: Diseases, Distribution, Diagnosis. [ Google Scholar ]
- Wilson M.E., Weld L.H., Boggild A. Fever in returned travelers: Results from the GeoSentinel Surveillance Network. Clin. Infect. Dis. 2007; 44 :1560. [ PubMed ] [ Google Scholar ]
- World Health Organization (WHO) WHO; Geneva: 2009. Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. [ PubMed ] [ Google Scholar ]
National Geographic content straight to your inbox—sign up for our popular newsletters here

- CORONAVIRUS COVERAGE
What vaccines mean for the return of travel
COVID-19 jabs will eventually help tourism start again, but expect a trip full of immunity passports, mouthwash tests, and wary travelers.
Passengers line up at a check-in point at Berlin’s Brandenberg Airport on December 21, 2020. Many countries, including Germany, have temporarily banned travelers from the United Kingdom due to a more transmissible strain of COVID-19 discovered there.
At the end of December 2020, hope returned to the world, including hope for restarting travel, as countries began approving the Pfizer/BioNTech, Moderna, and Oxford-AstraZeneca vaccines. Sometime in 2021, when enough people are vaccinated against—and immune from—COVID-19, this could mean a return to globetrotting (or at least less-risky domestic vacations).
Yet anxiety surrounding travel isn’t going away as medical workers and older Americans begin to get jabbed. In the United States, people are still reluctant to plan future trips. A December 2020 National Geographic and Morning Consult poll asked how respondents would approach travel after the coronavirus pandemic was under control. Forty-nine percent said they would “travel less due to concern of exposure to other people” and a third (34 percent) said they didn’t expect to travel more in 2021 to make up for the lack of trips in 2020.
What do COVID-19 vaccines mean for travel in the near and short term, and how will attitudes toward them speed up (or slow down) the process of getting back on the road or into the skies? Here’s what we’ve learned.
There’s no vaccination for fear
“Vaccine hesitancy is a critical obstacle to overcome,” says Dr. Tom Kenyon, the chief health officer of Project HOPE , a global health and humanitarian relief organization, and a former director at U.S. Centers for Disease Control and Prevention (CDC). To get back to travel, the U.S. and the world need herd immunity, thought to be achieved when about 70 percent of the population has protective antibodies. Kenyon says, though, that “70 percent is an arbitrary figure, and there is no ‘off/on’ switch with herd immunity.” Recent news about more transmissible strains of COVID-19 suggests that herd immunity might only come when 90 percent of citizens have antibodies.
“In order to bring COVID-19 under control, a vast majority of Americans (upwards of 75 to 80 percent) will need to get vaccinated,” says Michelle Williams, epidemiologist and dean of faculty at Harvard T.H. Chan School of Public Health . But vaccine rollout is already taking longer than expected— only about three million of the promised 20 million doses were injected into American arms in December. The U.K. says it might take a year to vaccinate its population.
Every country needs herd immunity for travel to resume the way it did pre-pandemic. “We are part of a global community whose health, economy, and futures are linked and impacted by the pandemic,” says Dr. Jewel Mullen, associate dean for health equity and associate professor of population health and internal medicine at the University of Texas at Austin’s Dell Medical School .
It may be tough to reach that herd stage in the U.S., though. Just 47 percent of people who responded to the National Geographic and Morning Consult poll said they’d get a COVID-19 vaccine as soon as it was available, and more than a quarter (27 percent) disagreed with that statement. Still, 58 percent of respondents said they would eventually get a vaccine.
Sleeves rolled up, masks on
The new COVID vaccines are better than predicted at preventing vaccinated people from getting sick. Health experts were hoping for a vaccine with 50 to 70 percent efficacy . Clinical trials show Pfizer/BioNTech’s vaccine— approved now in dozens of countries including the U.S. —is a whopping 95 percent effective. It’s fully effective a month after the first dose (you need a second jab at least 21 days later) and it starts to work 10 to 12 days after the first shot. The Moderna vaccine is similar.
However, it’s still not clear if vaccinated people can spread COVID-19 . “We don’t yet have data on whether any COVID vaccines reduce risk of spread/transmission; right now data only shows that vaccines reduce risk of illness,” says ABC News chief medical correspondent Dr. Jennifer Ashton.
The virus that causes COVID-19 is a novel one and there’s still a lot to learn about it. The CDC says more than half of all COVID-19 infections are spread by asymptomatic people ; 35 percent before the infected person feels any symptoms and 24 percent by people who never develop symptoms. Kenyon says that “leaves open the possibility that some vaccinated people could still get infected without developing symptoms, and could then silently transmit the virus.”

A man receives a COVID-19 test at Los Angeles International Airport amid a coronavirus surge in California on December 22, 2020.
Everyone wants to go on vacation again, but the priority for vaccine developers was preventing illness and death, not restarting cruises. “Trials thus far have only tracked how many vaccinated people became sick with COVID-19 compared with unvaccinated people,” says Kenyon. While there’s a good chance the antibodies triggered by the vaccine will result in a lowered likelihood of spreading the virus to others, we won’t know until more studies are done.
That’s the key reason why, a month after getting your first shot, you can’t just shop in a crowded Moroccan souk like it’s 2019. Until research tells us more, Mullen says “travelers must not abandon the measures we already know help reduce the risk of transmission—masks, good hygiene, physical distancing, and not traveling if one has symptoms.”
It’s reassuring that the majority of Americans in the National Geographic and Morning Consult poll (67 percent) plan to continue to always or sometimes wear masks during flu season, when running errands and grocery shopping (63 percent), and if there’s bad air pollution (64 percent).
The world needs immunity
Getting the world immunized won’t be quick or easy. According to the People’s Vaccine Alliance —a movement of health and humanitarian organizations including Amnesty International and Oxfam— rich countries secured 54 percent of the most promising vaccine candidates , even though they have only 14 percent of the world’s population. Without urgent action, the People’s Vaccine Alliance says that only 10 percent of the populations of 67 developing countries can be vaccinated in 2021. That puts citizens of popular tourism destinations like Cambodia , Kenya , Sri Lanka , and Uganda at risk.
Rich nations securing vaccine contracts was an important part of funding vaccine development. The Vaccine Alliance accused rich nations of hoarding vaccines, and some might. Over the coming months, we’ll learn how equitable global vaccine distribution really is. Canada secured more potential vaccines than any other country—about 10 doses per person from seven vaccine candidates—and intends to share extra doses of what’s proven safe and effective. Developing countries are anxious to know how and when.
( Even friendly borders, like the ones between the U.S. and Canada, have shut during the pandemic. Here’s why. )
A key solution is the Access to COVID-19 Tools (ACT) Accelerator initiative and its COVAX vaccines project , co-led by the World Health Organization and other partners. COVAX’s aim is to accelerate vaccine creation and ensure equitable global distribution, first delivering enough doses for the most vulnerable 20 percent of 184 participating countries’ populations, from Afghanistan to Zimbabwe. Rich countries help fund poorer countries, although Russia and the U.S. have yet to join. The ACT Accelerator initiative is still underfunded , needing at least $23.7 billion in 2021.
Until the world has herd immunity, travel needs to be approached cautiously: As Mullen says, “being overly, or prematurely, confident about the vaccines’ effectiveness can lead to putting people in other countries at risk. Travel gives us a chance to contribute to their faltering economies. But contributing to disease spread undermines that.”
What’s a vaccine passport?
After the most vulnerable get their life-saving shots, eventually we’ll have enough to start inoculating the general population. That’s when vaccination status will matter. It’s unlikely you’ll need to be vaccinated to travel, but it will be a lot easier if you are.
Qantas was the first airline to announce it will require international passengers to be vaccinated. Cyprus, as of March 1, 2021, plans to allow anyone who can prove they’ve been vaccinated to skip the requirement for a negative test. Singapore is considering relaxing its quarantine rules for vaccinated travelers if clinical trials show vaccines lower transmission risks.
Even at home, being vaccinated will save you time and money: Live Nation/TicketMaster is exploring how to verify that people attending its events are either vaccinated or have a recent negative COVID test, which local authorities may require. Tourist attractions, stores, and restaurants could follow suit.
( If you must travel now, here’s how to make it safer .)
Until vaccines are readily available, COVID-19 tests will remain a necessary part of travel. However, testing is getting easier and more accurate—for example, there’s a new test (supposedly 99 percent accurate) that uses a mouthwash-like swish , not a nose swab.
How you’ll prove your vaccination status is still being figured out. Fake COVID test documents are already a problem, as is assurance that the person who took the test is the same one brandishing the certificate.
Several “vaccine passports” are being marketed, but CommonPass looks the most promising. A collaboration between the World Economic Forum and nonprofit The Commons Project , CommonPass is a secure way to validate individuals’ COVID test and vaccination credentials and is being piloted internationally. The first government to sign on to the CommonTrust Network was Aruba , allowing travelers to securely prove their COVID status to enjoy its Caribbean beaches by February 2021.
Vaccine tourism won’t be a thing—yet
COVID-19 vaccines are one of the world’s hottest commodities, which means people with money or status will try to jump the queue. Most nations say their vulnerable citizens—essential workers and the elderly—will get it first, but politicians were among the first to roll up their sleeves in the U.S ., and the rich are offering donations in hopes of skipping the line.
Related: epic photos from an airplane window
Until there’s an abundance of approved and delivered vaccines, it’s all but impossible for anyone outside government-identified priority groups to get a shot. Yet, as soon as the U.K. approved the Pfizer/BioNTech vaccine, travel agents in India started fielding requests for quick vaccination trips to the U.K., even though that would require a complex web of dual citizenship, quarantines, and more. Attention is now on the U.S. and Russia as possible vaccine destinations .
Mark Warner, a trade lawyer and principal of MAAW Law in Toronto, says that, before booking a vaccination vacation, you should ask yourself how can you be certain you’re “reliably being injected with the advertised approved vaccine” versus a counterfeit. Also ponder how you can “be certain that the chain of custody has been reliably maintained at all stages,” including that proper temperatures were maintained. On top of that, will your vaccination certification be valid?
No one is safe until everyone is safe
“This is not about me , it’s about we ,” says Ashton. “This pandemic has unroofed a dichotomy between responsible behavior for our own personal health and that for others’ personal health.” COVID-19 has reminded us that we live in a shared world—for all of us to be healthy and prosperous, we need to take care of each other.
Safe and effective COVID-19 vaccines mean that life, including travel, are likely to get back to normal one day. Assuming that vaccines also protect against most virus mutations as well as against spreading the virus, COVID restrictions should end once herd immunity is achieved. The whole world needs that herd immunity, and achieving that in 2021 is unlikely. Until then, reminds Mullen, “the privilege to travel somewhere should not come at the expense of the residents of those destinations.”
Related Topics
- PUBLIC HEALTH
You May Also Like

What’s that smell? It might just be the next big thing in travel.

5 pandemic tech innovations that will change travel forever
Free bonus issue.

New tools offer peace of mind for pandemic travel

Should you buy carbon offsets for your air travel?

What families can do now that kids are getting the vaccine
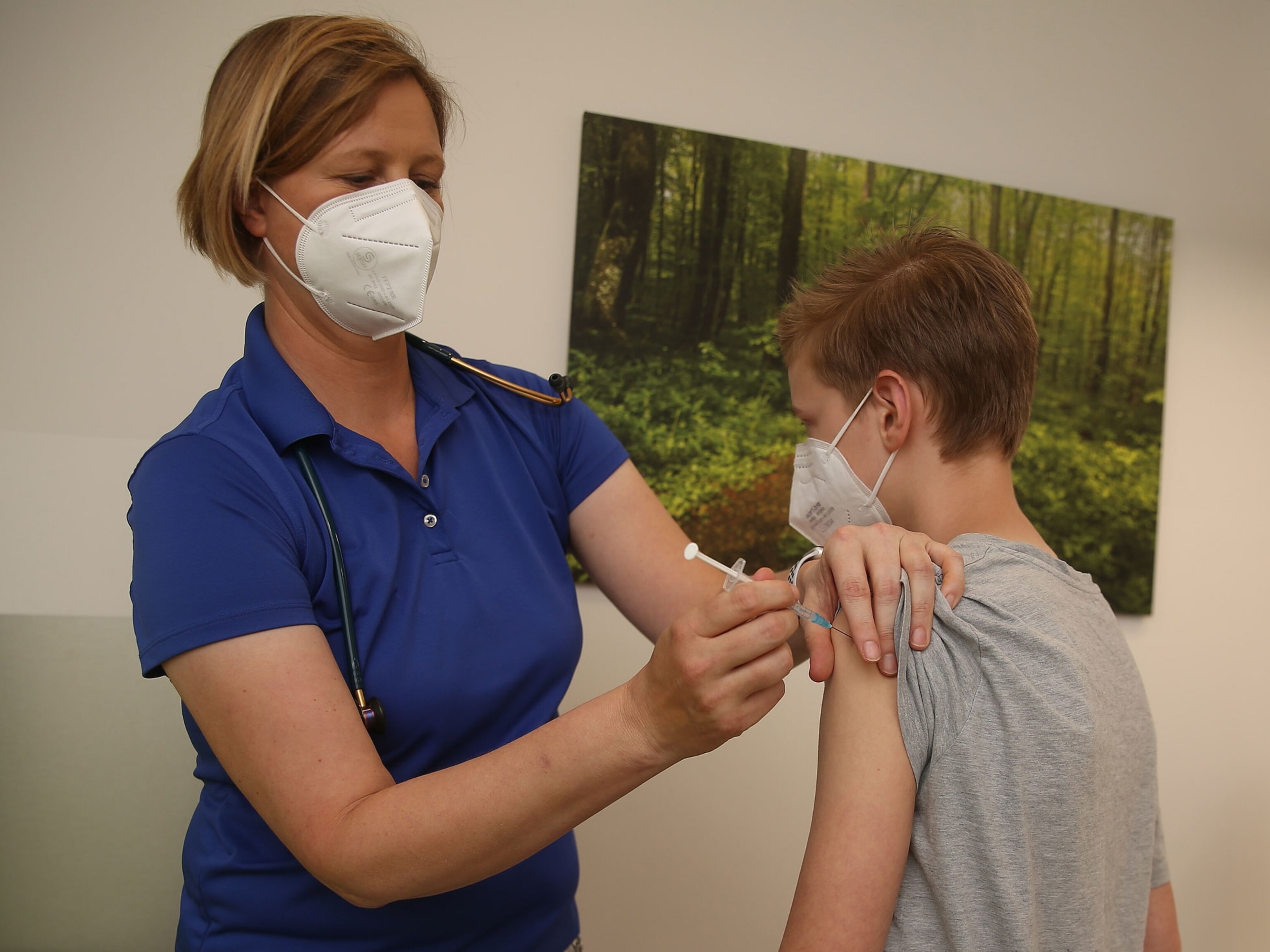
What to expect with COVID-19 vaccines for kids ages 5 to 11

How to sleep soundly on a plane
- History & Culture
- Environment
- Paid Content
History & Culture
- History Magazine
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 10 - Vietnam
- Section 11 - Rapid Diagnostic Tests for Infectious Diseases
General Approach to the Returned Traveler
Cdc yellow book 2024.
Author(s): Jessica Fairley
The Posttravel Evaluation
Common syndromes, general management.
As many as 43%–79% of travelers to low- and middle-income countries become ill with a travel-associated health problem. Although most of these illnesses are mild, some travelers become sick enough to seek care from a health care provider. Most posttravel infections become apparent soon after returning from abroad, but incubation periods vary, and some syndromes can present months to years after initial infection or after travel.
When evaluating a patient with a probable travel-associated illness, approach the differential diagnosis by incorporating both the patient presentation and risk factors related to travel (e.g., destination, duration of travel, and exposures; see Table 11-01 ). Salient points of the history of present illness and the travel and medical history, descriptions of common nonfebrile syndromes, and initial management steps are outlined below. The differential diagnosis and management for a traveler with fever (or febrile syndrome) is discussed in detail in Sec. 11, Ch. 4, Fever in the Returned Traveler .
Table 11-01 Elements of a complete travel history in an ill returned traveler
HISTORY OF THE PRESENT ILLNESS
Symptoms: primary & associated
Date of symptom or illness onset
Geographic location at time of symptom onset (e.g., while away, in transit, after return)
Healthcare received while abroad and after return (e.g., medications, hospitalizations)
TRAVEL DETAILS
Destinations visited and itineraries
Duration of travel (date of departure and date of return)
Reason for travel
- Business (include details about possible exposures and type of work done)
- Immigration
- Missionary, volunteer, humanitarian aid work
- Providing or receiving medical care
- Research or education
- Visiting friends & relatives
Accommodations and sleeping arrangements
- Hotel with or without air conditioning, window screens, or mosquito nets
- Safari, including camping outdoors, in a lodge, in a luxury tent
- Someone’s home
Transportation used
RECREATIONAL ACTIVITIES
Camping and hiking
Sightseeing
Water exposures
- Boating or rafting
- Fresh water (lake, river, stream) bathing, boating, swimming, wading
- Hot springs
- Hot tubs, swimming pools
- Ocean (diving, snorkeling, surfing; consider marine life exposure)
Other activities
Animal or arthropod bites, stings, scratches
Drinking water (bottled, purified, tap, use of ice)
- Raw fruits, vegetables
- Undercooked meat
- Unpasteurized dairy products
Insect bites (mosquito, tick, sand fly, tsetse fly)
Medical or dental care (planned or unplanned)
Disease outbreaks in visited destinations
Sexual activity during travel (document condom use, new partner[s])
Tattoos or piercings while traveling
VECTORBORNE DISEASE PRECAUTIONS
Adherence to malaria prophylaxis
Insect repellent use (25%–40% DEET or other Environmental Protection Agency–registered product)
Mosquito nets
VACCINES RECEIVED
Coronavirus disease 2019 (COVID-19)
Hepatitis A
Hepatitis B
Japanese encephalitis
Measles-mumps-rubella (MMR)
Meningococcal disease
Tetanus-diphtheria-acellular pertussis (Tdap)
Yellow fever
MEDICATIONS TAKEN
Malaria prophylaxis
All medicines taken (whether routinely or for symptomatic treatment), including antibiotics
- Herbal, complementary, alternative
- Over the counter
- Prescription
PAST MEDICAL HISTORY
Chronic medical conditions
- Autoimmune disease
- Heart disease
- Immunosuppressive conditions
Recent illnesses or surgeries
ADDITIONAL INFORMATION
Alcohol, tobacco, illicit drug use
Family history
Recent travel, domestic or international, especially ≤6 months
History of the Present Illness
As with any medical evaluation, the history of the present illness and associated clinical factors are the first considerations when approaching an ill returned traveler. Information about the timing of illness, immunization and prophylaxis history, itinerary, exposures, and comorbidities can help refine the diagnosis.
Timing of Illness in Relation to Travel
Because most common travel-associated infections have short incubation periods, most ill travelers will seek medical attention ≤1 month of returning from their destinations. Dengue and other arboviral infections, influenza, and travelers’ diarrhea are examples of infections with shorter incubation periods (<2 weeks). Diseases with slightly longer incubation periods, ≤4–6 weeks, include viral hepatitis, acute HIV, leishmaniasis, malaria, and typhoid fever, among others. Occasionally, some infections (e.g., leishmaniasis, malaria, schistosomiasis, tuberculosis) might become manifest months or even years after a traveler returns. Consider malaria in the differential diagnosis of any traveler who traveled to a malaria-endemic area ≤1 year of presentation. A detailed travel history that extends beyond a few months before presentation is important. The most common travel-associated infections by incubation period are listed in Table 11-02 , Table 11-03 , and Table 11-04 .
Table 11-02 Common travel-associated infections by incubation period: <14 days
Table 11-03 common travel-associated infections by incubation period: 14 days–6 weeks, table 11-04 common travel-associated infections by incubation period: >6 weeks, immunization & prophylaxis history.
When evaluating an ill returned traveler, review the traveler’s vaccination history and malaria prophylaxis used. Fewer than half of US travelers who visit low- and middle-income countries seek pretravel medical advice, increasing the likelihood that they did not receive pretravel vaccines and did not receive or take antimalarial drugs. Although adherence to malaria prophylaxis does not rule out the possibility of malaria, it substantially reduces the risk and increases the possibility of an alternative diagnosis.
Likewise, history of vaccination against hepatitis A and yellow fever would make these diseases unlikely causes of hepatitis or jaundice in a returning traveler. Remember to ask about routine vaccinations like measles-mumps-rubella (MMR) and tetanus-diphtheria-pertussis (Tdap). The most common vaccine-preventable diseases among returned travelers seeking care at GeoSentinel clinics during 1997–2010 included hepatitis A, hepatitis B, influenza, and typhoid fever. More than half of these patients with vaccine-preventable diseases were hospitalized.
Itinerary & Travel Duration
A traveler’s itinerary is crucial to formulating a differential diagnosis because exposures differ depending on the region of travel and the specific areas (e.g., rural vs. urban). A febrile illness with nonspecific symptoms could be dengue, malaria, rickettsial disease, or typhoid fever, among others, depending on the itinerary and endemicity of these infections. Being able to exclude certain infections based on the travel itinerary can help avoid unnecessary testing.
A 2013 study from the GeoSentinel Surveillance Network found that the frequency of certain diseases varied depending on the region of the world visited; among travelers with fevers, for example, dengue was diagnosed most frequently among travelers coming from Asia, while malaria was diagnosed most frequently among travelers returning from Africa.
Travel duration is also a factor because the risk for a travel-associated illness increases with the length of the trip. A tropical medicine specialist can assist with the differential diagnosis and might be aware of outbreaks or the current prevalence of an infectious disease in an area. The 2014–2015 Ebola virus epidemic in West Africa highlighted the importance of epidemiologic factors and travel itineraries in managing patients and protecting staff and the community.
Knowing a patient’s exposures during travel (e.g., consumption of contaminated food or water, insect bites, freshwater swimming) also can assist with the differential diagnosis. In addition to malarial parasites, mosquitoes transmit viruses (e.g., chikungunya, dengue, yellow fever, Zika) and filarial parasites (e.g., Wuchereria bancrofti ). Depending on the clinical syndrome, a history of a tick bite could suggest a diagnosis of tick-borne encephalitis, African tick-bite fever, or other rickettsial infections. Tsetse flies are the vector for transmission of Trypanosoma brucei , a protozoan that causes African sleeping sickness. Tsetse flies are large, and their bites are painful; patients often recall being bitten. Freshwater bathing, swimming, wading, or other contact can put travelers at risk for leptospirosis, schistosomiasis, and other diseases.
Accommodations and activities also can influence the risk of acquiring certain diseases while abroad. Travelers who visit friends and relatives are at greater risk for malaria, typhoid fever, and other diseases, often because they stay longer, travel to more remote destinations, have more contact with local water sources, and typically do not seek pretravel advice (see Sec. 9, Ch. 9, Visiting Friends & Relatives: VFR Travel ). Travelers backpacking and camping in rural areas have a greater risk for certain diseases than those staying in luxury, air-conditioned hotels.
Comorbidities
Underlying illnesses can affect a traveler’s susceptibility to infection as well as the clinical manifestations and severity of disease. An increasing number of international travelers are immunosuppressed, whether due to HIV infection, treatment with immune-modulating medications, being an organ transplant recipient, or other primary or acquired immunodeficiencies (see Sec. 3, Ch. 1, Immunocompromised Travelers ). In addition, several factors associated with travel can exacerbate underlying conditions (e.g., chronic lung disease, inflammatory bowel disease, ischemic heart disease).
Symptoms & Illness Severity
Although the symptoms of many infectious and travel-associated syndromes overlap, the initial symptoms and presentation should ultimately guide the differential diagnosis: gastrointestinal symptoms and febrile illnesses are the most common syndromes in returning travelers. Remember that conditions such as appendicitis, urinary tract infections, and domestically acquired viral infections also can present in returning travelers.
Severity of illness is not only important for patient triage but also can help clinicians distinguish certain infections. Is the traveler hemodynamically stable? Is the infection potentially life-threatening (e.g., malaria)? Does the traveler have a severe respiratory syndrome or signs of hemorrhagic fever? Some suspected illnesses might necessitate prompt involvement of public health authorities. For more details, see General Management, later in this chapter.
The 3 most common clinical syndromes after travel to low- and middle-income countries are dermatologic conditions, diarrheal diseases, and systemic febrile illnesses, each of which is described in more detail elsewhere in this section (see Dermatologic Conditions , Persistent Diarrhea in Returned Travelers , and Fever in the Returned Traveler ). Evaluate febrile travelers returning from malaria-endemic destinations immediately. Other common clinical presentations and findings include animal bites and scratches, asymptomatic eosinophilia, and respiratory illnesses.
Animal Bites & Scratches
Promptly evaluate any traveler who reports animal exposures during travel (see Sec. 4, Ch. 7, Zoonotic Exposures: Bites, Stings, Scratches & Other Hazards ). Consider travelers with animal bites and scratches as high-risk for rabies exposure, and provide rabies postexposure prophylaxis, as indicated (see Sec. 5, Part 2, Ch. 18, Rabies ). If the traveler was exposed to a macaque, herpes B postexposure prophylaxis might be indicated (see Sec. 5, Part 2, Ch. 1, B Virus ).
Asymptomatic Eosinophilia
Eosinophilia in a returning traveler suggests possible helminth infection. Allergic diseases, hematologic disorders, and a few other viral, fungal, and protozoan infections also can cause eosinophilia. Eosinophilia can be present during pulmonary migration of parasites (e.g., Ascaris , hookworm, schistosomiasis, Strongyloides ).
Other parasitic infections associated with eosinophilia include lymphatic filariasis, chronic strongyloidiasis, acute trichinellosis, and visceral larva migrans. These infections might be asymptomatic, but also could have associated symptoms (e.g., rash, swelling). In an outbreak of sarcocystosis among travelers returning from Tioman Island, Malaysia, those affected presented with eosinophilia and myalgias and had eosinophilic myositis on muscle biopsy (see Sec. 5, Part 3, Ch. 18, Sarcocystosis ).
Parasitic infections are rare in most travelers, so consider other etiologies for eosinophilia; for instance, eosinophilia can be a sign of a hematologic malignancy. See Section 5 for more information on specific diseases.
Respiratory Illnesses
Respiratory illnesses are frequent among returned travelers and are typically associated with common respiratory viruses, including influenza and now, severe acute respiratory syndrome coronavirus 2, the cause of coronavirus disease 2019 (COVID-19). Since the pandemic began in early 2020, coronavirus disease (COVID-19) has overtaken influenza in overall global incidence. And although historically influenza has been the most common vaccine-preventable disease associated with international travel, COVID-19 could surpass it in that regard. To make that determination, however, a better understanding of the epidemiology of travel-associated COVID-19 transmission is needed (see Sec. 5, Part 2, Ch. 3, COVID-19 ).
If the travel history is appropriate and respiratory symptoms do not have a clear alternative diagnosis, include other emerging respiratory infections (e.g., avian influenza, Middle East respiratory syndrome [MERS]) in the differential diagnosis. In suspected cases of an emerging respiratory infection, alert local public health authorities and the Centers for Disease Control and Prevention (CDC) immediately. See relevant chapters in Section 5 for more information on these emerging infections; for a list of febrile respiratory illnesses that can occur after exposures in tropical destinations, see Table 11-10 in the chapter, Fever in the Returned Traveler .
Delayed illness onset and chronic cough after travel could be tuberculosis, especially in a long-term traveler or health care worker. Helminths and helminth infections associated with pulmonary symptoms include Ascaris , hookworms ( Ancylostoma or Necator ), paragonimiasis, schistosomiasis, and strongyloidiasis.
Most posttravel illnesses can be managed on an outpatient basis, but some patients, especially those with systemic febrile illnesses, might need to be hospitalized. Furthermore, potentially severe, transmissible infections (e.g., COVID-19, Ebola, MERS) require enhanced infection control measures and often, higher levels of care. Severe clinical presentations (e.g., acute respiratory distress, hemodynamic instability, mental status changes) require inpatient care. Have a low threshold for admitting a febrile patient if malaria is suspected; complications can occur rapidly. Management in an inpatient setting is especially vital for patients unlikely to follow up reliably or who have no one at home to assist if symptoms quickly worsen.
Initial Evaluation
After conducting a thorough physical exam, paying particular attention to skin manifestations or evidence of prior insect bites, order tests based on chief complaint and exposure history. Frequently useful tests include complete blood count with differential (to look for anemia, eosinophilia, leukocytosis, leukopenia, thrombocytopenia); blood cultures and malaria rapid diagnostic tests (depending on the presence of fever and travel itinerary); a complete metabolic profile (to identify electrolyte, renal, or liver dysfunction); serologic or PCR tests for arboviral infections (as needed); and stool cultures and ova and parasite exams. These tests often can help narrow the differential diagnosis and determine disease severity.
Antimicrobial Resistance
Be aware of the risk to international travelers for acquiring antimicrobial resistant organisms. Carefully consider travel history when caring for patients, both to identify effective treatments for infections and to ensure infection control interventions are in place to prevent spread of antimicrobial resistance (see Sec. 11, Ch. 5, Antimicrobial Resistance ).
Consultation
Consult an infectious disease specialist when managing complicated or severe travel-associated infections, or when the diagnosis remains unclear. A tropical medicine or infectious disease specialist should be involved in cases that require specialized treatment (e.g., leishmaniasis, severe malaria, and neurocysticercosis).
Involve local, state, and federal public health authorities whenever managing transmissible, high-consequence infections. CDC provides on-call assistance with the diagnosis and management of parasitic infections at 404-718-4745 (for parasitic infections other than malaria) or 770-488-7788 (toll-free at 855-856-4713) for malaria, during business hours. After business hours or for other conditions, call the CDC Emergency Operations Center at 770-488-7100.
The following authors contributed to the previous version of this chapter: Jessica K. Fairley
Bibliography
Angelo KM, Kozarsky PE, Ryan ET, Chen LH, Sotir MJ. What proportion of international travellers acquire a travel-related illness? A review of the literature. J Travel Med. 2017;24(5):tax046.
Boggild AK, Castelli F, Gautret P, Torresi J, von Sonnenburg F, Barnett ED, et al. Vaccine preventable diseases in returned international travelers: results from the GeoSentinel Surveillance Network. Vaccine. 2010;28(46):7389–95.
Centers for Disease Control and Prevention. Notes from the field: acute muscular sarcocystosis among returning travelers—Tioman Island, Malaysia, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(2):37–8.
Chen LH, Wilson ME, Davis X, Loutan L, Schwartz E, Keystone J, et al. Illness in long-term travelers visiting GeoSentinel clinics. Emerg Infect Dis. 2009;15(11):1773–82.
Fairley JK, Kozarsky PE, Kraft CS, Guarner J, Steinberg JP, Anderson E, et al. Ebola or not? Evaluating the ill traveler from Ebola-affected countries in West Africa. Open Forum Infect Dis. 2016;3(1):ofw005.
Hamer DH, Connor BA. Travel health knowledge, attitudes and practices among United States travelers. J Travel Med. 2004;11(1):23–6.
Hendel-Paterson B, Swanson SJ. Pediatric travelers visiting friends and relatives (VFR) abroad: illnesses, barriers and pre-travel recommendations. Travel Med Infect Dis. 2011;9(4):192–203.
Leder K, Torresi J, Libman MD, Cramer JP, Castelli F, Schlagenhauf P, et al. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Intern Med. 2013;158(6):456–68.
Ryan ET, Wilson ME, Kain KC. Illness after international travel. N Engl J Med. 2002;347(7):505–16.
Schulte C, Krebs B, Jelinek T, Nothdurft HD, von Sonnenburg F, Loscher T. Diagnostic significance of blood eosinophilia in returning travelers. Clin Infect Dis. 2002;34(3):407–11.
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Bird flu outbreak is an 'evolving situation.' Here's what to know about symptoms, spread.
Many Americans are brimming with questions after officials in Texas last week announced the state's first case of bird flu in a human .
On April 1, Texas health officials said a person became infected with bird flu, or avian influenza A(H5N1) virus , after close contact with infected cows. The week prior, sick dairy cattle in Texas and Kansas tested positive for bird flu. Bird flu was later reported in a Michigan dairy herd that included cows transported from Texas. Cattle in New Mexico and Idaho are also presumed to be positive for the disease, officials said.
The only symptom reported by the Texas patient was pink eye, or conjunctivitis, according to an update April 1 from the U.S. Centers for Disease Control and Prevention.
Officials say the risk to public health remains low. They note that there are steps people can take to curb the spread of the potentially dangerous virus. The events in Texas, they say, raise future concerns about how the bird flu virus evolves.
"This is definitely an evolving situation," Dr. Diego Diel, director of Cornell University's virology laboratory at the Animal Health Diagnostic Center, which worked to sequence the virus, told USA TODAY. "Right now, I think the viruses that have been detected in cattle and in other animals in these farms don't contain any mutations that would indicate increased transmissibility or pathogenesis to humans."
But if the virus is being transmitted from cow to cow, Diel stressed, it's important to continue monitoring the virus in the long term to see whether there are potential mutations that could cause spillover into other species, including humans.
CDC says cases rising: What to know about meningococcal disease
How does bird flu spread?
Bird flu primarily spreads through contact with infected birds. Most cases in humans have occurred after a person had unprotected exposure to sick or dead infected animals.
Avian flu viruses infect birds’ respiratory and gastrointestinal tracts, which causes them to shed the virus via their saliva, mucous and feces, the CDC said. Humans and other mammals can get it when they get enough virus in their eyes, nose, or mouth or inhale it into their lungs.
People who have close contact or unprotected contact for long periods are at greater risk of infection. The disease can cause mild upper respiratory issues or severe illness, including pneumonia and multiple organ failure that leads to death.
In the U.S., the disease tends to spread from wild birds. However, outbreaks in commercial poultry or backyard flocks that led to deaths have been reported in 48 states since February 2022.
Can cats get bird flu?
Officials identified the latest bird flu cases in unpasteurized milk from sick cattle at dairy farms in Kansas and Texas, in addition to a positive throat swab of a cow at another Texas dairy farm. This spread to cows is believed to be the first for the species. The other species caught the virus directly from wild birds: cats.
Cornell researchers believe the virus was transmitted to Texas dairy cows through contaminated water and other food sources from infected birds migrating through the area. The virus then likely spread among cows who were near each other or the birds, however, there isn't yet definitive proof of this, said Diel, who is an associate professor of virology.
In early March, Dr. Elisha Frye, an assistant professor of practice at Cornell's Department of Population Medicine and Diagnostic Sciences, received a call about an outbreak among Texas dairy herds of a disease of unknown origin. Samples of milk and manure and nasal swabs from the cattle showed bird flu was present. Researchers also found evidence of bird flu in the testing of dead birds and one of three cats found dead at the dairy facilities around the same time.
"It was kind of the same timeline as when we found it in the cattle samples, but it did kind of link it together," Frye told USA TODAY. "The birds, the cat and milk from the cows all having the same pathogen in them made sense at the time for that being the main cause of illness."
How do humans get bird flu?
It's rare for humans to be infected with bird flu. The only other human case in the U.S. occurred in 2022, in a person incarcerated in a Colorado prison who was exposed to poultry infected with avian flu.
On Tuesday, the CDC said the current public health risk is low, and there is no person-to-person spread of bird flu so far. That is a vital measurement that would prompt concern for the spread of the disease.
There remains an increased risk for poultry, livestock and farmers and workers in these sectors, as well as veterinarians, veterinary staff and first responders who respond to cases, officials said.
Ozempic and Wegovy: Weight-loss drugs cost $1,000 a month but less than $25 to make. Why do we pay so much?
Do eggs carry bird flu? What about dairy products?
Food production officials have been taking steps to prevent the distribution of milk or eggs from infected animals. Cooked eggs and pasteurized milk, in general, should be safe for consumers.
Last week, the largest U.S. chicken egg supplier reported positive tests for bird flu at its facility in the Texas Panhandle. In a news release , Cal-Maine Foods said production at the Panhandle facility stopped temporarily, following protocols to prevent bird flu set by the U.S. Department of Agriculture. Personnel at the company killed about 1.6 million laying hens and 337,000 young hens to curb the spread of the virus.
There isn't as simple of a solution to reduce the risk of bird flu since the eggs can carry the virus, so the traditional method has been to destroy products and kill the poultry, said Diel, of Cornell.
Among dairy cows, milk from animals suspected or confirmed to have the virus is being removed from human food supplies. However, even if milk from infected cows makes it to the commercial milk supply, pasteurization effectively inactivates bacteria and viruses, including influenza, according to a March 29 joint news release from the CDC, USDA and the Food and Drug Administration . In addition to protecting against bird flu, pasteurization is central to other health efforts. The FDA says that unpasteurized raw milk can have microorganisms dangerous to human health.
Dr. Meghan Davis, an associate professor at the Johns Hopkins Bloomberg School of Public Health and a former dairy veterinarian, said it’s important to note differences among industries in poultry and cattle, and how the virus gets treated: Chicken culling, or killing, has been a steadfast way to curb disease spread, whereas this is a first for cattle, and it appears cows aren’t getting as sick.
She said people are at risk if they consume raw milk and cheese or live near an area with intensive dairy production.
The spread among cows is a red flag for public health officials and veterinary care professionals. But Davis said she was encouraged by the fact that the person with bird flu only had mild eye problems and the cows had mild symptoms.
“If that’s the worst we see, then that’s good,” she said. “But we don’t yet know."
How can bird flu be stopped?
The latest developments are reminders for Americans to take standard precautions when storing, cooking and consuming food, said Darin Detwiler, a professor of food policy at Northeastern University , who has advised the USDA and FDA on food safety. The recommendations include frequent hand-washing when preparing food, properly cooking eggs and meat and reducing consumption of unpasteurized dairy products.
Detwiler believes consumers should be proactive if they have concerns about outbreaks.
"That's our power as consumers that are stakeholders in this," he told USA TODAY. "We don't have to wait until we're harmed to voice our support or concern over some of these issues."
Other ways to avoid contracting bird flu include eliminating unprotected exposure to sick or dead animals, including wild birds, poultry or domesticated birds, or other sick or dead wild or domesticated animals. This includes contact with animal feces, waste, or materials contaminated by animals suspected or confirmed with bird flu.
People working directly with animals who could be infected should wear personal protective equipment such as face masks – ideally approved particulate respirators such as N95 masks, as well as goggles, gloves, boots and boot covers. Additionally, they should use fluid-resistant coveralls and disposable head covers or hair covers.
People who have spent time near animals confirmed or suspected of being sick should be monitored for signs and symptoms for 10 days after the exposure. This includes those who were wearing PPE.
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
What’s Happening With Dairy Cows and Bird Flu
Though the virus is circulating in dairy cows, human exposure remains low.
Public Health On Call
The H5N1 strain of avian influenza—commonly known as bird flu—has been circulating among wild migratory birds for the past two years, with substantial spillover into poultry farms.
But what's sparking concern among scientists and public health officials alike is the recent discovery of the virus in dairy cows and the subsequent infection of a dairy farm employee—the second person in America ever documented to be infected with H5N1. The virus has now spread to 16 herds in six states according to the USDA, fueling concerns about potential further transmission to humans.
In this Q&A, adapted from the April 8 episode of Public Health On Call , Stephanie Desmon speaks with Meghan Davis , DVM, PhD ’12, MPH ’08, associate professor in Environmental Health and Engineering , and Andrew Pekosz , PhD, professor in Molecular Microbiology and Immunology , about H5N1’s jump between species, what that means for the virus’s pandemic potential, and what the appearance of the virus in dairy means for consumers.
What’s going on with the avian flu?
AP: This virus has been around for over 20 years. It's been mutating over time, and something happened in the last couple of years to cause an explosion of cases in wild birds. Not surprisingly, that's led to spillover infections in some poultry farms. There's also been an increase in mammals that have been infected, such as skunks, bears, and foxes, presumably from feeding on dead infected birds. And recently, we've seen spillover of this virus into dairy cows.
Cattle have not been reported to be infected with any of the influenza A viruses—human or animal—to date. Anytime this virus enters a new host, we set off some alarm bells in the scientific community to see what's going on.
Can we expect to see more cases in humans?
AP: I expect that over the next few weeks, we're going to be seeing more cases in cows and humans, because humans are in close contact with cows during many dairy processes. Hopefully, this will not be a large outbreak, but we certainly expect to see more cases.
Were you surprised by this outbreak?
MD: I am surprised that it's in dairy cows, because when we think about animal models for influenza, we think about mustelids, like ferrets or mink. We have also seen a number of sick farm cats that tested positive. What is most interesting about seeing [H5N1] in dairy is that researchers haven't been focusing on biosecurity and biocontainment for things like avian influenza—which is typically transmitted from a bird reservoir. Dairy farms are often quite open to the air—birds might spend time in areas where the cows eat, for example.
One of the other things we are seeing is some symptoms of disease in the cows. I've not heard of high mortality yet, but they have been showing fairly nonspecific signs, like not eating or milking well. Most of these tend to be somewhat older cows because adult cows who are lactating are in a different category of susceptibility than young calves. What we don't know yet is if perhaps the virus is in all the populations within the farm, and only some of them are showing symptoms.
Is the milk they produce safe for consumption?
MD: For the average person buying commercial milk, we don't have any evidence that would suggest concern. If you buy pasteurized milk from a commercial dairy processor, the risk is extremely low. Pasteurization, which involves temperature and pressure and time, is designed to inactivate microbes to make the milk safer to consume and to give it longer shelf life. I strongly advise against consuming raw milk products, no matter where you live, because there are other risks, not just avian influenza.
What can the surveillance data from infected cows tell us?
AP: Two things are really important. One is: The virus has gone from the respiratory tract through lots of different organs, through the blood, and made it all the way to the milk. In humans, the influenza virus stays within the respiratory tract. We have seen H5N1 move out of the respiratory tract in other animals, but usually that's associated with a really fast mortality. As soon as the virus leaves the lungs, the animals are so sick that they die. We're seeing a case here where the animals don't seem to be really sick, but the virus is making it to other parts of the animal. That's going to tell us something perhaps unique about the H5N1 virus compared to seasonal human viruses.
The second critical thing is: If there is spread of this virus from cow to cow, is the virus changing and getting better adapted to replicating or spreading in cows? Bird flu jumping to mammals is important because anything that allows the virus to adapt to a mammal has the potential for making it better able to infect humans. Understanding what happens now with the spread of the virus and how the sequence of the virus changes is going to be critically important. The first sequences [from cows] look like the virus is almost identical to the bird virus. But we haven't really sampled animals that presumably acquired the infection from other cows.
If it's spreading from cow to cow, is that a wholly different problem?
MD: There is a lot of swapping of cows in the dairy industry, and there is a diverse population of farmers, each of them has their own way of doing things. And that means that we may need to educate farmers about perhaps restricting certain sales or trade of dairy cows if evidence shows that you could introduce avian flu through a cow brought in from outside the farm.
Something I'm very interested in is: Where were each of these cows exposed? To what degree was this one event that is now spreading through these networks of sale and trade and movement of dairy cows? Or is this multiple events in which you've had an introduction [of the virus] from birds? Because that also changes the dynamics as we think about genetics and the potential for evolution.
Is H5N1 considered a major threat at this time?
AP: H5N1 registers as what we call “a virus with pandemic potential.” Humans presumably all have some immunity to H1 and H3 influenza viruses, which can cause seasonal epidemics, but they can't cause pandemics at the level of what we saw with COVID because there's just too much immunity in the population that limits the spread and dampens down disease severity.
However, the human population is essentially completely naive—has no preexisting immunity—to H5 viruses. Therefore, similar to what we saw with COVID, in the worst case scenario, if this virus enters humans and starts to spread, all of us are susceptible, and we could see massive increases in numbers of cases.
H5 viruses are rather deadly in poultry. They're not so deadly in wild birds, but they seem to be deadly in mammals, and we don't know what they'll do in humans.
MD: Right now, the average person should just be aware and avoid things like raw milk products. However, because we are seeing the potential for disease in cats, and we don't know yet if that came from cows or birds or some other pathway—it's a good idea to prevent your cats from having contact with wild birds. If they're indoors, keep them indoors, and if they become ill, consult your veterinarian.
This interview was edited for length and clarity by Morgan Coulson, an editorial associate in the Office of External Affairs at the Johns Hopkins Bloomberg School of Public Health.
How Concerned Should We Be About Bird Flu?
What You Need to Know About H5N1
The Bird Flu Spilling Over Into Mammals (Podcast)
Related Content

How Dangerous is Dengue?

New Johns Hopkins Institute Aims to Safeguard Human Health on a Rapidly Changing Planet

9 Things to Know About Sun Safety and Skin Cancer

The Omnipresence of PFAS—and What We Can Do About Them

Five Reasons Why the Global Health Community Should Help Save Forests
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- March Madness
- AP Top 25 Poll
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
AT&T says a data breach leaked millions of customers’ information online. Were you affected?
FILE - The sign in front of an AT&T retail store is seen in Miami, July 18, 2019. The theft of sensitive information belonging to millions of AT&T’s current and former customers has been recently discovered online, the telecommunications giant said Saturday, March 30, 2024. In an announcement addressing the data breach, AT&T said that a dataset found on the dark web contains information including some Social Security numbers and passcodes for about 7.6 million current account holders and 65.4 million former account holders. (AP Photo/Lynne Sladky, File)
- Copy Link copied
NEW YORK (AP) — The theft of sensitive information belonging to millions of AT&T’s current and former customers has been recently discovered online, the telecommunications giant said this weekend.
In a Saturday announcement addressing the data breach, AT&T said that a dataset found on the “dark web” contains information including some Social Security numbers and passcodes for about 7.6 million current account holders and 65.4 million former account holders.
Whether the data “originated from AT&T or one of its vendors” is still unknown, the Dallas-based company noted — adding that it had launched an investigation into the incident. AT&T has also begun notifying customers whose personal information was compromised.
Here’s what you need to know.
WHAT INFORMATION WAS COMPROMISED IN THIS BREACH?
Although varying by each customer and account, AT&T says that information involved in this breach included Social Security numbers and passcodes — which, unlike passwords, are numerical PINS that are typically four digits long.
Full names, email addresses, mailing address, phone numbers, dates of birth and AT&T account numbers may have also been compromised. The impacted data is from 2019 or earlier and does not appear to include financial information or call history, the company said.
HOW DO I KNOW IF I WAS AFFECTED?
Consumers impacted by this breach should be receiving an email or letter directly from AT&T about the incident. The email notices began going out on Saturday, an AT&T spokesperson confirmed to The Associated Press.
WHAT ACTION HAS AT&T TAKEN?
Beyond these notifications, AT&T said that it had already reset the passcodes of current users. The company added that it would pay for credit monitoring services where applicable.
AT&T also said that it “launched a robust investigation” with internal and external cybersecurity experts to investigate the situation further.
HAS AT&T SEEN DATA BREACHES LIKE THIS BEFORE?
AT&T has seen several data breaches that range in size and impact over the years .
While the company says the data in this latest breach surfaced on a hacking forum nearly two weeks ago, it closely resembles a similar breach that surfaced in 2021 but which AT&T never acknowledged, cybersecurity researcher Troy Hunt told the AP Saturday.
“If they assess this and they made the wrong call on it, and we’ve had a course of years pass without them being able to notify impacted customers,” then it’s likely the company will soon face class action lawsuits, said Hunt, founder of an Australia-based website that warns people when their personal information has been exposed.
A spokesperson for AT&T declined to comment further when asked about these similarities Sunday.
HOW CAN I PROTECT MYSELF GOING FORWARD?
Avoiding data breaches entirely can be tricky in our ever-digitized world, but consumers can take some steps to help protect themselves going forward.
The basics include creating hard-to-guess passwords and using multifactor authentication when possible. If you receive a notice about a breach, it’s good idea to change your password and monitor account activity for any suspicious transactions. You’ll also want to visit a company’s official website for reliable contact information — as scammers sometimes try to take advantage of news like data breaches to gain your trust through look-alike phishing emails or phone calls.
In addition, the Federal Trade Commission notes that nationwide credit bureaus — such as Equifax, Experian and TransUnion — offer free credit freezes and fraud alerts that consumers can set up to help protect themselves from identity theft and other malicious activity.
AP Reporter Matt O’Brien contributed to this report from Providence, Rhode Island.

IMAGES
COMMENTS
Captain Trips is a nickname for the constantly-shifting antigen virus that exterminates 99.4% of the human population in The Stand. The meaning of the nickname is never revealed. Developed under the codename Project Blue by a biological weapon's laboratory located beneath California's Mojave Desert, it is also known as Blue virus (Blue Virus), 848-AB, A-prime, A6, the rales, superflu, choking ...
In each one, the virus is referred to as Captain Trips on several occasions. It even appears in King's short story "Night Surf," that was published in 1969 and served as inspiration for the larger epic. In the 2020 miniseries version of The Stand (made for CBS All Access), the term Captain Trips is used in the first episode.
That means the fatality rate for this virus is 99 percent. That means we're the future." The mind-boggling twist will leave one question buzzing through your mind if you haven't read King's novel: Why are Stu, Frannie and Harold not infected with Captain Trips? Ready for spoilers from the book? Well, read at your own risk.
"Captain Trips" does, however, appear in the book as a colloquial phrase used by young people to identify the virus. The virus was initially created by a military biological weapons lab under ...
The Stand: Captain Trips Is STILL the Most Ridiculous Name for a Fictional Virus. Captain Trips is one of the names of the virus in The Stand, and it makes no sense in universe. WARNING: The following contains spoilers for The Stand Episode 1, "The End," now streaming on CBS All Access. Talk to any Stephen King fan, and they will acknowledge ...
The TRIPS waiver refers to a proposal, advanced by the governments of South Africa and India, to the World Trade Organization to waive intellectual property rights protection for technologies needed to prevent, contain, or treat COVID-19 "until widespread vaccination is in place globally, and the majority of the world's population has ...
There's no scientific definition for this term; it simply refers to a collision of RSV (respiratory syncytial virus), flu, and COVID-19 to the extent that it might overwhelm hospital emergency departments. While all three viruses are present right now, they aren't each peaking at the same time. Pediatric RSV and flu cases are now down ...
When I talk about bad trips, I mean the trips that register in the body as a trauma or injury to the nervous system. And that is not, in fact, the same thing as a difficult trip. What happens when we deny this truth is that we inadvertently alienate those who have had traumatic or harmful experiences. These people have endured a trauma, and are ...
Traveler's diarrhea is a digestive tract disorder that commonly causes loose stools and stomach cramps. It's caused by eating contaminated food or drinking contaminated water. Fortunately, traveler's diarrhea usually isn't serious in most people — it's just unpleasant. When you visit a place where the climate or sanitary practices are ...
At a meeting of the Council for Trade-Related Aspects of Intellectual Property Rights (TRIPS) on 6 June, WTO members welcomed the adoption of the TRIPS waiver decision on COVID-19 vaccines at the 12th Ministerial Conference (MC12) and began discussions on a possible extension to cover the production and supply of COVID-19 diagnostics and therapeutics. Trade officials also exchanged views on ...
The phrase is mentioned in the first episode of the CBS All Access limited series, but not explained. According to some online sci-fi fan forums, the best explanation of where the phrase comes ...
Via CNBC, recent data suggests the flu-like coronavirus has a mortality rate among those it infects of 3.4 percent worldwide.And with a comparatively small proportion of the world's population infected, imagining coronavirus as a sweeping phenomenon — one capable of toppling governments and hitting the reset button on law and order generally — appears to be on the pessimistically bleak side.
Counting on 'Endemic': The Travel Industry Readies for a New Phase. A growing call to consider the coronavirus a permanent fixture in our lives is resonating among travel operators. But that ...
A recent survey by Skift Research found that 73 percent of respondents intended to take a road trip in 2020, and Mr. Borko said that the E.U. action will likely accelerate that trend. Because so ...
Follow the package directions. Spray the plants twice, three days apart, and the thrips should disappear. For fruit trees: Spray dormant oil on the trees. As a last resort, dust the undersides of leaves with diatomaceous earth. Black thrips and thrip damage on a fig tree.
Road trips have soared in popularity during the pandemic, and driving to your holiday destination—while avoiding contact with others—does mean less indoor time with strangers than flying.
Browse our specialists and get the care you need. There are different types of travel-associated infections that cause fever, along with other symptoms to include diarrhea, vomiting, rashes, and muscle aches. The most common of these include malaria, dengue, typhoid fever, and chikungunya.
What follows are breakdowns applicable to all three travel modes: air, rail, and highway. The pros and cons of air travel. Risk of contracting the virus when traveling on airline starts at the ...
Viral infections are any illness you get from a virus (a small germ that uses your cells to reproduce). Common viral illnesses include colds, the flu, COVID-19, norovirus ("stomach flu"), HPV (warts) and herpes simplex virus (cold sores). Many viruses go away on their own, but some cause life-threatening or chronic illnesses.
There may also be rules and precautions for COVID-19 while you're travelling and at both where your trip originates and where you are going. Always, follow travel advisories issued by both the country of origin and of destination. ... reduce the likelihood of importing the virus; and/or as a means to detect potential new variants of concern ...
The .gov means it's official. ... and style of travel, as well as the particular characteristics of a given trip, to ascertain the risk of serious disease presenting as fever. The travel itinerary is important because many diseases are limited in their geographic distribution ... Zika virus was discovered in Uganda in 1947, and human ...
Safe and effective COVID-19 vaccines mean that life, including travel, are likely to get back to normal one day. Assuming that vaccines also protect against most virus mutations as well as against ...
Okay. So. Trip and Virus have a six year age gap, and they met as teenagers. That means that upon meeting they were 13 and 19, respectively. They had also known Aoba for a while while Aoba was also a teenager, between ages of 13-19. We know he couldn't have been 19 because that would make Virus the same age as him - and if Virus is currently 23 ...
CDC Yellow Book 2024. As many as 43%-79% of travelers to low- and middle-income countries become ill with a travel-associated health problem. Although most of these illnesses are mild, some travelers become sick enough to seek care from a health care provider. Most posttravel infections become apparent soon after returning from abroad, but ...
Bird flu outbreak is an 'evolving situation.'. Here's what to know about symptoms, spread. Many Americans are brimming with questions after officials in Texas last week announced the state's first ...
AP: This virus has been around for over 20 years. It's been mutating over time, and something happened in the last couple of years to cause an explosion of cases in wild birds. Not surprisingly, that's led to spillover infections in some poultry farms. There's also been an increase in mammals that have been infected, such as skunks, bears, and ...
TSWV (Tomato Spotted Wilt Virus) Observado por primera vez en el año 1906. En 1919 se publicó la primera descripción de esta nueva enfermedad en cultivos de tomate en Australia. En 1930 se determinó que el agente causal de la enfermedad era un virus y lo llamaron "Tomato Spotted Wilt Virus". En 1920 E.U.A. y Canadá.
NEW YORK (AP) — The theft of sensitive information belonging to millions of AT&T's current and former customers has been recently discovered online, the telecommunications giant said this weekend. In a Saturday announcement addressing the data breach, AT&T said that a dataset found on the "dark web" contains information including some ...