- Words with Friends Cheat
- Wordle Solver
- Word Unscrambler
- Scrabble Dictionary
- Anagram Solver
- Wordscapes Answers
Make Our Dictionary Yours
Sign up for our weekly newsletters and get:
- Grammar and writing tips
- Fun language articles
- #WordOfTheDay and quizzes
By signing in, you agree to our Terms and Conditions and Privacy Policy .
We'll see you in your inbox soon.

Cruise Synonyms
Words related to cruise.
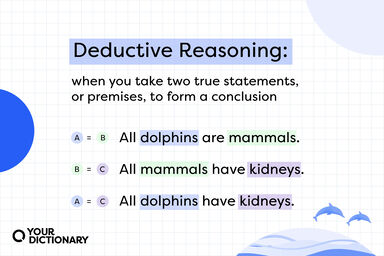
Related words are words that are directly connected to each other through their meaning, even if they are not synonyms or antonyms. This connection may be general or specific, or the words may appear frequently together.
- cruise-ship
- mini-cruises
- live-aboard
Cruise Sentence Examples
I want to take a cruise , I think, when Ashley graduates.
The British admiral, when informed that the French were at sea, justified Napoleon's estimate of his probable course in such a contingency, by making a useless cruise to Egypt.
In 1865 he started on a long canoeing cruise in his " Rob Roy " canoe, and in this way made a prolonged water tour through Europe, a record of which he published in 1866 as A Thousand Miles in the Rob Roy Canoe.
How I ended up on a cruise ?
In connexion with the last, he made a cruise in the Channel fleet, on board the "Victory," as a volunteer under the command of Admiral Sir Charles Hardy.
Related Articles
Cruise Is Also Mentioned In
- captain's table
- cruise ship
- cruising radius
- booze-cruise
- garde-manger
- cruise control
Words near Cruise in the Thesaurus
- cruise-missile
Related Words and Phrases
Bottom_desktop desktop:[300x250].
- ABBREVIATIONS
- BIOGRAPHIES
- CALCULATORS
- CONVERSIONS
- DEFINITIONS
Vocabulary
What is another word for cruise ?
Synonyms for cruise kruz cruise, this thesaurus page includes all potential synonyms, words with the same meaning and similar terms for the word cruise ., princeton's wordnet rate these synonyms: 2.2 / 6 votes.
cruise, sail verb
an ocean trip taken for pleasure
Synonyms: sheet , canvass , sail , canvas
- cruise verb
drive around aimlessly but ostentatiously and at leisure
"She cruised the neighborhood in her new convertible"
travel at a moderate speed
"Please keep your seat belt fastened while the plane is reaching cruising altitude"
look for a sexual partner in a public place
"The men were cruising the park"
sail or travel about for pleasure, relaxation, or sightseeing
"We were cruising in the Caribbean"
Matched Categories
Dictionary of english synonymes rate these synonyms: 0.0 / 0 votes.
Synonyms: rove over the sea
cruise noun
Synonyms: roving voyage
PPDB, the paraphrase database Rate these paraphrases: 0.0 / 0 votes
List of paraphrases for "cruise":
cruz , cruising , cruises , liners , flights , cruiser
How to pronounce cruise?
How to say cruise in sign language, words popularity by usage frequency, how to use cruise in a sentence.
Miles Teller :
I've been having some conversations with Miles Teller [ Tom Cruise ] about it. We'll see.
James Walker :
We receive on average a call a month from a family member who loses a parent or child at sea, so why should families in an air crash be able to seek their emotional losses against the airlines, but not passengers on a pleasure cruise ship at sea ?
Peace Boat :
There's potential with a very green cruise ship to get a lot of attention at each port of call and that can make an impact.
Mars Incrucio :
It actually happens so often the cruise companies have a policy for it.
Hans Kristensen :
A low-yield The Trident D5s warhead would be harder to defend against than a warhead delivered by a bomber or a cruise missile.
Use the citation below to add these synonyms to your bibliography:
Style: MLA Chicago APA
"cruise." Synonyms.com. STANDS4 LLC, 2024. Web. 12 Jul 2024. < https://www.synonyms.com/synonym/cruise >.
Discuss these cruise synonyms with the community:
Report Comment
We're doing our best to make sure our content is useful, accurate and safe. If by any chance you spot an inappropriate comment while navigating through our website please use this form to let us know, and we'll take care of it shortly.
You need to be logged in to favorite .
Create a new account.
Your name: * Required
Your email address: * Required
Pick a user name: * Required
Username: * Required
Password: * Required
Forgot your password? Retrieve it
Are we missing a good synonym for cruise ?
Image credit, the web's largest resource for, synonyms & antonyms, a member of the stands4 network, free, no signup required :, add to chrome, add to firefox, browse synonyms.com, are you a human thesaurus, what is the synonym of rebuke, nearby & related entries:.
- cruelly adverb
- cruelness noun
- cruelty noun
- cruise control noun
- cruise liner noun
- cruise missile noun
- cruise ship noun
- cruiser noun
Alternative searches for cruise :
- Search for cruise on Amazon

- Daily Crossword
- Word Puzzle
- Word Finder
- Word of the Day
- Synonym of the Day
- Word of the Year
- Language stories
- All featured
- Gender and sexuality
- All pop culture
- Writing hub
- Grammar essentials
- Commonly confused
- All writing tips
- Pop culture
- Writing tips
Advertisement
noun as in journey
Strongest matches
- sightseeing
Strong matches
- commutation
- peregrination
Weak matches
- globetrotting
verb as in journey on a trip or tour
- cover ground
- get through
- go into orbit
- knock around
- make a journey
- make one's way
- take a boat
- take a plane
- take a train
- take a trip
Example Sentences
You just travel light with carry-on luggage, go to cities that you love, and get to hang out with all your friends.
He did travel to China and Australia while the story was unfolding.
In doing so he exposed the failure of other airlines in the region to see the huge pent-up demand for cheap travel.
“The tribe is really made of people who put travel as a priority in their entire lifestyle,” says Evita.
Brands like Lo & Sons and Delsey are already tapping Travel Noire to connect with black travelers.
One thing was certain: Grandfather Mole could travel much faster through the water than he could underground.
The mothers know better than any one else how hard a way the little girl will have to travel through life.
He could lie in bed and string himself tales of travel and adventure while Harry was downstairs.
Under ordinary circumstances these men can travel with their burden from twenty to thirty miles a day.
The rules regulating travel on highways in this country are called, "the law of the road."
Related Words
Words related to travel are not direct synonyms, but are associated with the word travel . Browse related words to learn more about word associations.
verb as in tour
verb as in flow
- mill around
- move around
noun as in systems of information exchange
- information technology
- public relations
- telecommunications
verb as in make good time
- make headway
- make strides
verb as in sail
- keep steady pace
- push off/push on
- wander about
Viewing 5 / 93 related words
On this page you'll find 177 synonyms, antonyms, and words related to travel, such as: driving, excursion, flying, movement, navigation, and ride.
From Roget's 21st Century Thesaurus, Third Edition Copyright © 2013 by the Philip Lief Group.
- TheFreeDictionary
- Word / Article
- Starts with
- Free toolbar & extensions
- Word of the Day
- Free content
Synonyms for cruise
- travel along
- keep a steady pace
an ocean trip taken for pleasure
Related words, drive around aimlessly but ostentatiously and at leisure, travel at a moderate speed, look for a sexual partner in a public place, sail or travel about for pleasure, relaxation, or sightseeing.
- cruciferous
- cruciferous plant
- cruciferous vegetable
- crucifix fish
- crucifixion
- cruel and unusual punishment
- cruel plant
- cruet-stand
- cruise control
- cruise liner
- cruise missile
- cruise ship
- cruiserweight
- crumbliness
- cruft together
- Cruft's Dog Show
- Cruft, Charles
- Cruicible steel
- Cruikshank George
- Cruikshank, George
- Cruise 3sixty
- Cruise Agent Accreditation Scheme
- cruise around in
- cruise around in (something)
- cruise by her
- cruise by him
- cruise by it
- cruise by me
- cruise by one
- cruise by somebody
- cruise by someone
- cruise by something
- cruise by them
- cruise by us
- cruise by you
- Cruise climb
- Cruise Control Accelerate
- Cruise Control Coast
- Cruise Control Owner's Group
- Cruise Control Resume
- Cruise Control Set Switch
- Cruise Control System
- cruise controls
- Cruise Director
- Facebook Share
Definition of 'cruise'

cruise in British English
Cruise in british english, cruise in american english, examples of 'cruise' in a sentence cruise, word lists with cruise, cobuild collocations cruise, trends of cruise.
View usage for: All Years Last 10 years Last 50 years Last 100 years Last 300 years
Browse alphabetically cruise
- cruise a highway
- cruise control
- All ENGLISH words that begin with 'C'
Related terms of cruise
- boat cruise
- cruise fare
- cruise line
- cruise port
- View more related words
Wordle Helper


Scrabble Tools
Quick word challenge
Quiz Review
Score: 0 / 5

- Cambridge Dictionary +Plus
Meaning of cruise in English
Your browser doesn't support HTML5 audio
- They're going on a cruise round the Med.
- They've just set off on a round-the-world cruise.
- Do you dream of a luxury skiing holiday or a Caribbean cruise?
- age of sail
- ocean-going
- under sail idiom
- They are cruising off the west coast of Vancouver Island.
- Thousands of spectators watched the tall ships cruise the Detroit River.
- After launch , the probe will cruise for 6 months before intercepting the comet beyond Earth's orbit .
- The car is more fuel efficient because the engine can run on just three of six cylinders when cruising.
- A guy cruised up in a convertible and offered me a lift .
- He goes cruising the streets looking for places to rob .
- Our department is doing all the work while the rest of the business is cruising.
You can also find related words, phrases, and synonyms in the topics:
Related word
Cruise | american dictionary, translations of cruise.
Get a quick, free translation!

Word of the Day
used for saying that you accept that you are wrong or that something is your fault

Committing, tackling, and solving: Talking about crime

Learn more with +Plus
- Recent and Recommended {{#preferredDictionaries}} {{name}} {{/preferredDictionaries}}
- Definitions Clear explanations of natural written and spoken English English Learner’s Dictionary Essential British English Essential American English
- Grammar and thesaurus Usage explanations of natural written and spoken English Grammar Thesaurus
- Pronunciation British and American pronunciations with audio English Pronunciation
- English–Chinese (Simplified) Chinese (Simplified)–English
- English–Chinese (Traditional) Chinese (Traditional)–English
- English–Dutch Dutch–English
- English–French French–English
- English–German German–English
- English–Indonesian Indonesian–English
- English–Italian Italian–English
- English–Japanese Japanese–English
- English–Norwegian Norwegian–English
- English–Polish Polish–English
- English–Portuguese Portuguese–English
- English–Spanish Spanish–English
- English–Swedish Swedish–English
- Dictionary +Plus Word Lists
- English Noun Verb
- American Verb Noun
- Translations
- All translations
To add cruise to a word list please sign up or log in.
Add cruise to one of your lists below, or create a new one.
{{message}}
Something went wrong.
There was a problem sending your report.
- Dictionaries home
- American English
- Collocations
- German-English
- Grammar home
- Practical English Usage
- Learn & Practise Grammar (Beta)
- Word Lists home
- My Word Lists
- Recent additions
- Resources home
- Text Checker
Definition of cruise noun from the Oxford Advanced Learner's Dictionary
- I'd love to go on a round-the-world cruise.
- a luxury cruise ship
- Fire crews were called to the scene.
- He crews for a billionaire on his yacht.
- We're taking a cruise around the Mediterranean.
- I'd love to cruise down the Nile.
- package tour
- self-catering
- have/take (British English) a holiday/ (North American English) a vacation/a break/a day off/ (British English) a gap year
- go on/be on holiday/vacation/leave/honeymoon/safari/a trip/a tour/a cruise/a pilgrimage
- go backpacking/camping/hitchhiking/sightseeing
- plan a trip/a holiday/a vacation/your itinerary
- book accommodation/a hotel room/a flight/tickets
- have/make/cancel a reservation/ (especially British English) booking
- rent a villa/ (both British English) a holiday home/a holiday cottage
- (especially British English) hire/ (especially North American English) rent a car/bicycle/moped
- stay in a hotel/a bed and breakfast/a youth hostel/a villa/ (both British English) a holiday home/a caravan
- cost/charge $100 a/per night for a single/double/twin/standard/ (British English) en suite room
- check into/out of a hotel/a motel/your room
- pack/unpack your suitcase/bags
- call/order room service
- cancel/cut short a trip/holiday/vacation
- apply for/get/renew a/your passport
- take out/buy/get travel insurance
- catch/miss your plane/train/ferry/connecting flight
- fly (in)/travel in business/economy class
- make/have a brief/two-day/twelve-hour stopover/ (North American English also) layover in Hong Kong
- experience/cause/lead to delays
- check (in)/collect/get/lose (your) (especially British English) luggage/ (especially North American English) baggage
- be charged for/pay excess baggage
- board/get on/leave/get off the aircraft/plane/ship/ferry
- taxi down/leave/approach/hit/overshoot the runway
- experience/hit/encounter severe turbulence
- suffer from/recover from/get over your jet lag/travel sickness
- attract/draw/bring tourists/visitors
- encourage/promote/hurt tourism
- promote/develop ecotourism
- build/develop/visit a tourist/holiday/ (especially British English) seaside/beach/ski resort
- work for/be operated by a major hotel chain
- be served by/compete with low-cost/ (especially North American English) low-fare/budget airlines
- book something through/make a booking through/use a travel agent
- contact/check with your travel agent/tour operator
- book/be on/go on a package deal/holiday/tour
- buy/bring back (tacky/overpriced) souvenirs
- They met on a cruise.
- a cruise along the coast
- a pleasure cruise around the bay
- Modern cruise liners have every conceivable luxury on board.
- Now they could afford the world cruise they had promised themselves.
- She worked on a cruise ship as a croupier.
- They are going on a Mediterranean cruise.
- This year's cruise will visit the Norwegian fjords.
- We will be taking a cruise down the Nile.
- You can take a leisurely cruise on the lake.
- on a/the cruise
- cruise along
- cruise around
Definitions on the go
Look up any word in the dictionary offline, anytime, anywhere with the Oxford Advanced Learner’s Dictionary app.

10 Luxury Cruise Lines That Will Make You Want to Ditch Plane Travel Forever
Posted: July 11, 2024 | Last updated: July 12, 2024

Thinking about booking your next dream vacation? As stunning as land-locked adventures and beautiful hotels can be, there’s something to be said about sailing the seas. Fortunately for us, nowadays, there are cruise ships that far exceed the family-fun agenda of the classic companies so often advertised on TV. While there’s absolutely nothing wrong with those cruise liners, there’s something special about not only traversing the ocean but doing so decked out to the nines. With that in mind, we’ve rounded up the best luxury cruise lines of 2023. Ahead, uncover the company that best aligns with your idea of the ultimate water-bound getaway.

Silversea is the “jewel in the crown” of the Royal Caribbean Group, not to mention the original luxury cruise line, first entering the space in 1994. The company touts 12 all-inclusive ships with destinations all over the world. Whether you want to explore the American West Coast, South America, Northern Europe and the British Isles, Africa, Asia, Australia and New Zealand, or even Antarctica, Silversea has a cruise to fit your fancy.
Speaking of fancy, the most luxurious cruise that Silversea offers is its 125-Day Chile to Norway sail, which rings up at $94,700. You don’t have to invest that much to enjoy a Silversea cruise, though. No matter which type of suite you book, you can expect butler service, optional 24/7 in-suite dining, endless access to premium beverages and craft cocktails, and complimentary caviar around the clock.
Explore Silversea Cruises

Paul Gauguin
Paul Gaugin stands out for its single-ship escapade into the luxury cruise space. With a variety of cruises that explore French Polynesia and the South Pacific, Paul Gauguin is a small-ship cruise line with 7-, 10-, 11-, and 14-night itineraries that focus on intimate experiences, delectable cuisine, stunning stateroom balcony views, butler service, and more. With a 1:1.5 crew-to-guest ratio, you can rest assured knowing that all of your needs will be met aboard the m/s Paul Gauguin.
Explore Paul Gauguin Cruises

Scenic Luxury Cruises & Tours
Scenic is unique in that it not only offers luxury ocean cruises but river cruises, too. The brand prides itself on operating and innovating with guest experience in mind. As such, all of its cruises have so much to offer voyagers, from extensive dining, leisure, and wellness options to striking design elements that will make you want to stay aboard for much longer than your itinerary.
Scenic Luxury Cruises & Tours has nine ships with oceanic destinations spanning from the Arctic and Europe to the Caribbean and Australia. Meanwhile, if you find yourself in France, you may want to check out Scenic’s beloved river cruises, in which you can tour the Seine in the utmost style.
Explore Scenic Luxury Cruises & Tours

Ponant has a fleet of 13 luxury cruise ships with destinations dotting the globe. The award-winning French cruise line is beloved for its tailor-made voyages, in which guests have access to myriad bespoke experiences both on and off board, from in-room dining to once-in-a-lifetime immersive excursions.
Since Ponant ships offer smaller capacity—more akin to a private yacht experience—they’re able to navigate private ports and preserved locations that large-scale cruise ships are unable to access. While aboard Ponant’s all-inclusive ships, you can anticipate exceptional French cuisine, delicious fine wines, complimentary Champagne and spirits, room service, and more.
Of course, if you need further inspiration to look into the cruise line, perhaps the fact that three-mast yacht, Le Ponant, is part of the Relais & Châteaux portfolio will do the trick.
Explore Ponant Cruises

Crystal is renowned for its personalized voyages all over the world, not to mention its palatial suites that will leave you picking your jaw up off the floor. In addition to well-appointed design, the cruise line offers an impressive dining experience, with authentic cuisines from all over the world. So whether you’re in the mood for American, Italian, Peruvian, or Japanese food, you’ll have ample options to choose from.
It’s also worth mentioning that the luxury cruise line took it to the next level with its spa, Aurora Spa. The gorgeous, sea-view spa offers a variety of face, body, salon, and healing treatments, including massages, facials, acupuncture, Chinese herbal medicine, and even IV drip therapy—so you won’t have to worry about feeling hung over at sea (especially considering the cruise line offers complimentary Champagne, fine wines, and premium spirits).
Explore Crystal

Windstar Cruises
Windstar Cruises operates a six-ship fleet dedicated to extraordinary sailing experiences. With small ships that carry less than 350 passengers, Windstar prides itself on offering guests intimate, aesthetic, unforgettable voyages spanning from Asia and Australia to Italy and Iceland.
While the staterooms and suites are stunning and the shore excursions are aplenty, it’s the food that really stands out aboard Windstar. As the official cruise line of the James Beard Foundation, Windstar offers a number of themed culinary cruises with food and bev from some of the most notable chefs of today, including Maxime Bilet (The Cooking Lab) and Jose Mendin (Pubbelly Noodle Bar, Habitat, Baja Bao).
Explore Windstar Cruises

The Ritz-Carlton Yacht Collection
The Ritz-Carlton is synonymous with luxury, so it’s no surprise that the company extended into oceanic adventures with a fleet of three superyachts. Where the Evrima was built in 2021, the Ilma and Luminara yachts are forthcoming in 2024 and 2025.
While classic cruise lines have a capacity in the thousands, often edging upward of 4,000, the Ritz-Carlton superyachts offer a more curated experience to 500 passengers or less. From the outside, the yachts are sleek and serene, fitting in beautifully with the sea. Within Evrima’s walls, though, moody modern interiors with magnificent ocean views await.
Guests can look forward to soaking tubs, expansive private balconies complete with sun beds and a whirlpool, walk-in wardrobes, and more. As far as destinations are concerned, The Ritz-Carlton Yacht Collection embarks on oceanic adventures in the Mediterranean and Caribbean.
Explore The Ritz-Carlton Yacht Collection Cruises

Seabourn is a luxury cruise line that speaks to our soul—and for more reasons than the simple fact that it touts a “Veranda Suite Upgrade.” The luxury cruise line sets sail in the Arctic, Canada and New England, the Amazon, Arabia, Africa, and India, and more.
Each of the fleet’s yachts, which carry between 458 and 600 guests, is outfitted with ocean-view suites only, so no matter what excursion you book, you can anticipate traveling in luxury style with a picturesque backdrop. You can also look forward to mouth-watering cuisine courtesy of renowned chef Thomas Keller.
Explore Seabourn Cruises

Cunard is known for its iconic black funnels, yes, but more so for its unparalleled large-scale onboard experiences. Although each of the cruise line’s ships carries upwards of 1,500 passengers, the four-ship fleet is adored for its luxury itineraries, stylish design, tranquil spa offerings, delectable cuisine, and unmatched comfort at sea.
Truly, if your goal is to book an unforgettable, Instagram-worthy cruise, Cunard is the way to go. From the stunning suites (decked out in pops of rich color, sumptuous textiles, and spectacular lighting) to the picturesque destinations, Cunard has it all.
Explore Cunard Cruises

Regent Seven Seas Cruises
If you want to get the most bang for your buck when booking a luxury cruise, Regent Seven Seas Cruises is a prime pick. The all-inclusive cruise line crafts a new definition of the category with complimentary roundtrip airfare, free unlimited shore excursions, include 2- to 3-night land programs, on-the-house bar and lounge experiences, and more.
The six-fleet cruise line is also known for its gorgeous interiors, complete with modern aesthetics, Art Deco embellishments, stunning chandeliers, and more. When traveling with Regent Seven Seas Cruises, guests can traverse the seven seas, with destinations in Africa and Arabia, Asia, Australia and New Zealand, the Caribbean and more. And if you don’t want to pick a single destination, there’s always the option to book a grand voyage or world cruise, which can last up to 168 days and cost upwards of $100,000.
Explore Regent Seven Seas Cruises
More for You
MTV's “Ridiculousness” Finds New Permanent Co-Host After Chanel West Coast's Exit (Exclusive)
Opinion: Sitting down all day is killing us. The cure is surprisingly simple — and difficult
'Out of Hand': Woman Praised for Refusing to Pay 20% Tip on Sandwich
Japan removes navy chief as sweeping misconduct investigation roils military
Lake Mead Danger Sparks Warning: 'Take Immediate Action'
How Far Did Frodo & Sam Walk in The Lord of the Rings?
This Is the Average 401(k) Balance for Ages 55 to 64
The Most Intriguing Mythical Creature in Each US State
28 Common Misconceptions We Have About The World
Travis Kelce shouts out Taylor Swift after singing ‘80s classic to win karaoke contest
Woman Takes Dog to Vet, Feels as if She 'Failed' After Hearing Diagnosis
Chris Hayes Flags 'Very Striking' Moment From Biden Press Conference: It Was 'Clarifying'
Who Was Carl Vinson And Why Does He Have An Aircraft Carrier Named After Him?
Forget burpees — this 5-move low-impact workout works your whole body in just 15 minutes
Thrilling town in Ireland's smallest county is surrounded by incredible things to do
Holocaust survivor meets family he never knew he had
NASCAR News: 23XI Racing Speaks Out After Huge Bubba Wallace Misconduct Fine
Thousands evacuate in face of emergency as monstrous fire surges out of control: 'It's going to be a challenge both day and night'
Sam Altman is seen driving a car that can cost $5 million. Everyone is thanking him for helping them pass their tests.
Trump names four finalists for running mate as he compares vice presidential race to The Apprentice
Synonyms of voyage
- as in cruise
- as in to travel
- as in to sail
- More from M-W
- To save this word, you'll need to log in. Log In
Thesaurus Definition of voyage
(Entry 1 of 2)
Synonyms & Similar Words
Thesaurus Definition of voyage (Entry 2 of 2)
- peregrinate
- road - trip
- knock (about)
- perambulate
Phrases Containing voyage
Thesaurus entries near voyage, cite this entry.
“Voyage.” Merriam-Webster.com Thesaurus , Merriam-Webster, https://www.merriam-webster.com/thesaurus/voyage. Accessed 12 Jul. 2024.
More from Merriam-Webster on voyage
Nglish: Translation of voyage for Spanish Speakers
Britannica English: Translation of voyage for Arabic Speakers
Subscribe to America's largest dictionary and get thousands more definitions and advanced search—ad free!

Can you solve 4 words at once?
Word of the day.
See Definitions and Examples »
Get Word of the Day daily email!
Popular in Grammar & Usage
Plural and possessive names: a guide, commonly misspelled words, how to use em dashes (—), en dashes (–) , and hyphens (-), absent letters that are heard anyway, how to use accents and diacritical marks, popular in wordplay, it's a scorcher words for the summer heat, flower etymologies for your spring garden, 12 star wars words, 'swash', 'praya', and 12 more beachy words, 8 words for lesser-known musical instruments, games & quizzes.

- Search Please fill out this field.
- Manage Your Subscription
- Give a Gift Subscription
- Newsletters
- Sweepstakes
- World's Best
Travel + Leisure Readers' 5 Favorite Small-ship Ocean Cruise Lines of 2023
Readers shared why great things come in small (ship) packages in our annual "World’s Best Awards" survey for 2023.
Paul Brady is the news director at Travel + Leisure and the brand's expert on cruise travel. He has been covering the travel industry for more than 15 years for outlets including Condé Nast Traveler , Skift , and The Huffington Post .
:max_bytes(150000):strip_icc():format(webp)/Paul-Brady-3744fd514a6045708c9dfc18375122af.jpg)
How Voting Works
- What Readers Loved
- The Full List
This year, small ships seem to be hitting the mark. These vessels, which Travel + Leisure defines as those with 150 to 299 cabins, offer what many readers consider the perfect blend of choice and comfort, with plenty of onboard dining and activities without the at-times overwhelming selection found on much larger ships. In fact, small ships may be driving a surge of interest in cruising generally, as new and newly refreshed options in this range are drawing both longtime cruisers and those eager to try a new way of traveling.
Every year for our World's Best Awards survey, T+L asks readers to weigh in on travel experiences around the globe — to share their opinions on the top hotels, resorts, cities, islands, cruise ships, spas, airlines, and more. Nearly 165,000 T+L readers completed the 2023 survey, an increase of nearly 25 percent over pre-pandemic voting levels. A total of more than 685,000 votes were cast across over 8,500 unique properties (hotels, cities, cruise lines, etc.).
For the cruise category, respondents were asked to rate individual ships; the results were combined to generate scores for cruise lines in different categories based on number of cabins. The small-ship ocean cruise line category is only for ships with 150 to 299 cabins. Some cruise lines may appear in multiple categories depending on the makeup of their fleet.
Ships were specifically rated on the criteria below:
- Cabins/facilities
- Itineraries/destinations
- Excursions/activities
For each characteristic, respondents could choose a rating of excellent, above average, average, below average, or poor. The final scores are averages of these responses.
Tim McKenna/Courtesy of Paul Gauguin Cruises
What Readers Loved
In the 2023 voting, readers gave high marks to established brands that have reinvigorated their offerings. Consider No. 2 Windstar Cruises, which recently rebuilt three of its small ships at an investment of $250 million, adding more suites, improved culinary options, and enhanced spa facilities to each. “I'm never going to be able to get on another cruise line,” said one convert, who traveled on Star Legend .
Meanwhile Paul Gauguin Cruises (No. 3) may have slipped a bit from its 2022 ranking but still posted a score of more than 92 points. That’s thanks to its luxurious service — most rooms come with butler service — and, no doubt, its dreamy itineraries that visit remote atolls in South Pacific and the cruise line’s private beach on Bora Bora. “It's the only way to see this part of the world,” one voter shared.
This year’s small-ship leader, though, made its mark with two new vessels that are unlike anything else sailing today. Read on to see how Viking captured this category — and for more details on all the top lines.
Courtesy of Viking
Typically thought of as a midsize-ship line, Viking took top honors in this category, too, thanks to its twin ships Viking Polaris and Viking Octantis . The expedition vessels, both of which have 189 cabins, are built for out-there adventures, whether on the waters of the Great Lakes or in the Southern Ocean on the way to Antarctica. “I can't say enough about how wonderful our experience was on the Viking Octantis to Antarctica. The ship is stunning in every way,” one voter said. “The excursions were all well-planned and executed — and the science and educational sessions were excellent,” another added. While shorter trips aboard these ships are possible, Viking can also arrange for a “ longitudinal world cruise .” These multi-month journeys will take intrepid guests from Minnesota to Ushuaia, Argentina — or the other way around — in small-ship comfort, with port excursions and insightful lectures along the way.
The Full List
Reader Score: 95.35
2. Windstar Cruises
WBA Hall of Fame honoree. Reader Score: 92.72
3. Paul Gauguin Cruises
WBA Hall of Fame honoree. Reader Score: 92.56
4. Seabourn
WBA Hall of Fame honoree. Reader Score: 92.51
5. Silversea
WBA Hall of Fame honoree. Reader Score: 90.56
Related Articles
'A polluting form of tourism': Amsterdam slashes cruise ship traffic in half

- Amsterdam will slowly phase out cruise ships and ultimately shutter its cruise terminal.
- The city’s Passengers Terminal Amsterdam (PTA) will cap cruise ships to 100 per year starting in 2026.
- By 2035, Amsterdam's terminal will close.
Get more news like this delivered to your inbox by signing up for our Travel newsletter here .
Amsterdam has announced it will slowly phase out cruise ships and ultimately shutter its cruise terminal as the popular destination cracks down on overtourism .
Starting in 2026, the city’s Passengers Terminal Amsterdam will cap cruise ships to 100 a year. Currently, the maximum is 190. The terminal will reduce to just one berth by the following year and require cruise ships to use shore power.
By 2035, Amsterdam's terminal – a brief 15-minute walk to the city center – will close.
“The city council wants a liveable, clean and sustainable city,” Amsterdam Deputy Mayor Alderman Hester van Buren said in a statement. “Sea cruise is a polluting form of tourism and contributes to crowds and emissions in the city.”
Learn more: Best travel insurance
What should I pack for a cruise? Here are 5 essential items to bring.
When cruise ships use shore power, they can switch off their own machinery, which cuts down on emissions and noise pollution. About 35% of cruise ships are equipped with shore power connections, according to the Cruise Lines International Association .
The proposed measures, a result of collaborative discussions between stakeholders from the industry, city, region, and national government, reflect a shared commitment to the city's future.
In the announcement, the Dutch city acknowledges the potential economic consequences from fewer tourists spending money in shops or museums and “less tourist tax collected.” The next budget memorandum is set to include the financial consequences of the cruise ship ban.
The city also is considering possible relocation of the passengers terminal to Coenhaven, a harbor in northwest Amsterdam. This move could bring new opportunities and a breath of fresh air to the area.
“Based on this feasibility study, the council will decide in consultation with the government, the Port Authority, and the province of North Holland whether relocation is feasible by 2035,” the announcement said.
“The announcement is a great example of the cruise industry’s long-standing partnership with the Port of Amsterdam and the direct outcome of our collaborative discussions on the relocation of the passenger terminal outside the city centre, which started back in 2016,” a spokesperson for the international cruise lines association told USA TODAY.
“Amsterdam is and will remain a popular cruise destination, and cruise tourism will continue delivering important economic benefits to the city,” the spokesperson said, adding that cruise tourists bring about $105 million a year and make up 1% of the more than 21 million visitors a year to the city.
The news in Amsterdam coincides with Seattle’s new order requiring all cruise ships to use shore power by 2027 to push its own cruise industry to be more sustainable.
Kathleen Wong is a travel reporter for USA TODAY based in Hawaii. You can reach her at [email protected] .
The Key Points at the top of this article were created with the assistance of Artificial Intelligence (AI) and reviewed by a journalist before publication. No other parts of the article were generated using AI. Learn more .

IMAGES
VIDEO
COMMENTS
Synonyms for CRUISE: voyage, sail, crossing, passage, roam, wander, stroll, drift; Antonyms of CRUISE: struggle, limp, flounder, stumble, lumber, trudge, shuffle, stamp
Find 31 different ways to say CRUISE, along with antonyms, related words, and example sentences at Thesaurus.com.
Noun. A voyage on a ship or boat taken for pleasure. A trip taken for pleasure, especially one lasting a day or less. A long walk, typically a tiring one. An easy victory or achievement. Verb. To travel on water in a vessel, especially for pleasure. To travel at a constant speed. To move about aimlessly.
Synonyms for CRUISES: voyages, crossings, sails, passages, roams, wanders, strolls, drifts; Antonyms of CRUISES: struggles, flounders, stumbles, limps, shuffles ...
Synonyms of 'cruise' in British English. cruise (noun) in the sense of sail. Definition. ... to travel at a moderate and efficient speed. A black and white police car cruised past. Synonyms. travel along . coast . drift. We proceeded to drift along the river. keep a steady pace . See examples for synonyms.
A cruise is a vacation spent on a ship that sails the ocean, periodically stopping in ports for sightseeing. ... travel on water propelled by wind or by other means. verb. drive around aimlessly but ostentatiously and at leisure ... synonyms: sail. see more see less. type of: ocean trip, voyage. an act of traveling by water. verb.
Another way to say Cruise? Synonyms for Cruise (other words and phrases for Cruise). Synonyms for Cruise. 1 093 other terms for cruise- words and phrases with similar meaning. Lists. synonyms. antonyms. definitions. sentences. thesaurus. ... travel. v., n. # journey, move ...
The British admiral, when informed that the French were at sea, justified Napoleon's estimate of his probable course in such a contingency, by making a useless cruise to Egypt. In 1865 he started on a long canoeing cruise in his " Rob Roy " canoe, and in this way made a prolonged water tour through Europe, a record of which he published in 1866 ...
Sense: Verb: travel on a cruise ship. Synonyms: voyage Collocations, sail Collocations, navigate, sail the sea, go on a cruise, take a boat trip, go on a boat trip, travel Collocations, travel by ship, ferry Collocations, go sailing, circumnavigate, hit the high seas, sail the seven seas.
Another way to say Cruises? Synonyms for Cruises (other words and phrases for Cruises). Synonyms for Cruises. 317 other terms for cruises- words and phrases with similar meaning. Lists. synonyms. antonyms. definitions. sentences. thesaurus. words. phrases. Parts of speech. verbs. nouns.
CRUISE - Synonyms, related words and examples | Cambridge English Thesaurus
Most related words/phrases with sentence examples define Cruise meaning and usage. Thesaurus for Cruise Related terms for cruise - synonyms, antonyms and sentences with cruise
To depart or leave. To travel by jet aircraft. To move about restlessly and stealthily, especially in search of prey. To move through the water in a boat using a paddle or paddles. Noun. Plural for a voyage on a ship or boat taken for pleasure. Plural for a long walk, typically a tiring one. Plural for an easy victory or achievement.
Find 139 different ways to say CRUISING, along with antonyms, related words, and example sentences at Thesaurus.com.
Another way to say Cruise? Synonyms for Cruise (verbs).
an ocean trip taken for pleasure. Synonyms: sheet, canvass, sail, canvas. cruise verb. drive around aimlessly but ostentatiously and at leisure. "She cruised the neighborhood in her new convertible". cruise verb. travel at a moderate speed. "Please keep your seat belt fastened while the plane is reaching cruising altitude".
Find 95 different ways to say TRAVEL, along with antonyms, related words, and example sentences at Thesaurus.com.
Synonyms for cruise in Free Thesaurus. Antonyms for cruise. 12 synonyms for cruise: sail, voyage, boat trip, sea trip, sail, coast, voyage, travel along, coast, drift ...
Synonyms for CRUISE in English: sail, voyage, boat trip, sea trip, sail, coast, voyage, travel along, coast, drift, …
7 meanings: 1. to make a trip by sea in a liner for pleasure, usually calling at a number of ports 2. to sail or travel over (a.... Click for more definitions.
CRUISE definition: 1. a journey on a large ship for pleasure, during which you visit several places: 2. (of a ship or…. Learn more.
Collocations Travel and tourism Travel and tourism Holidays/ vacations. have/ take (British English) a holiday/ (North American English) a vacation/ a break/ a day off/ (British English) a gap year; go on/ be on holiday/ vacation/ leave/ honeymoon/ safari/ a trip/ a tour/ a cruise/ a pilgrimage; go backpacking/ camping/ hitchhiking/ sightseeing
Paul Gaugin stands out for its single-ship escapade into the luxury cruise space. With a variety of cruises that explore French Polynesia and the South Pacific, Paul Gauguin is a small-ship cruise ...
Synonyms for VOYAGE: cruise, sail, passage, crossing, travel, journey, trek, tour, trip, pilgrimage
Travel + Leisure Readers' 10 Favorite Midsize-ship Ocean Cruise Lines of 2024. With adult-focused delights, these mid-size ocean cruise lines topped the list in our annual "World's Best Awards ...
A large fight broke out on a Carnival Cruise Line ship, video footage shared on social media shows. The incident occurred in the buffet area of the Carnival Paradise around 3 a.m. on the final day ...
According to official figures, almost 26 million visitors made an overnight stay in the Barcelona region in 2023, spending €12.75 billion ($13.8 billion).
Travel + Leisure Readers' 10 Favorite River Cruise Lines of 2024. Explore the world's coolest rivers via these 10 spectacular river cruise lines, voted the best by T+L readers in the "World's ...
Travel + Leisure Readers' 5 Favorite Small-ship Ocean Cruise Lines of 2023. Readers shared why great things come in small (ship) packages in our annual "World's Best Awards" survey for 2023.
Amsterdam will slowly phase out cruise ships and ultimately shutter its cruise terminal. The city's Passengers Terminal Amsterdam (PTA) will cap cruise ships to 100 per year starting in 2026. By ...